Enfermedad de Whipple: revisión sistemática de la literatura
DOI:
https://doi.org/10.22516/25007440.966Palabras clave:
Enfermedad de Whipple, Tropheryma, Revisión SistemáticaResumen
Introducción: La enfermedad de Whipple es una enfermedad crónica sistémica con predilección por el aparato digestivo, especialmente el intestino delgado. Fue descrita por vez primera en 1907 por George H. Whipple quien la denominó "lipodistrofia intestinal". Es causada por una bacteria grampositiva perteneciente a la familia de los Actinomycetaceae denominada Tropheryma whipplei.
Objetivos: Caracterizar a los pacientes con enfermedad de Whipple.
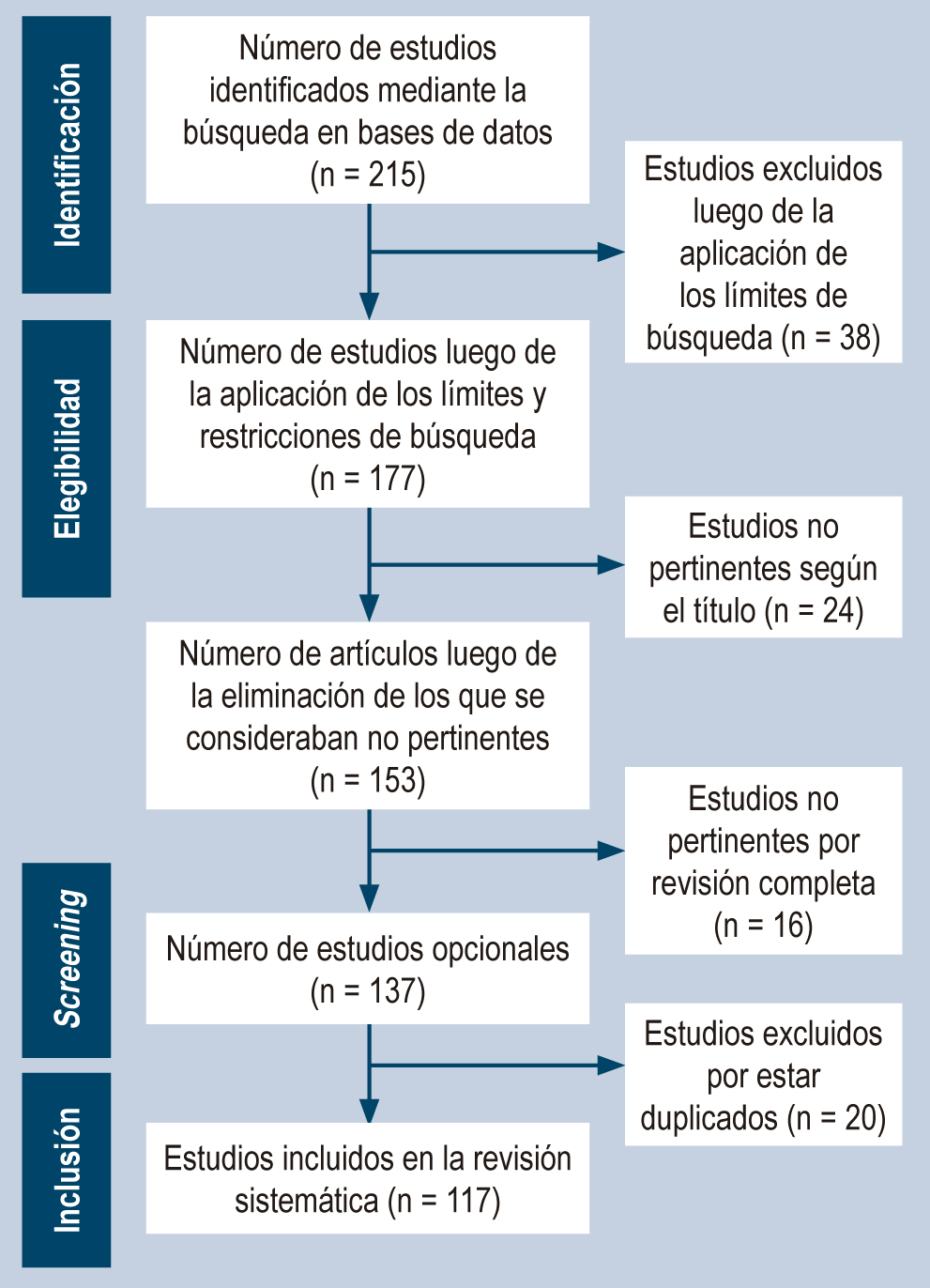
Materiales y métodos: Se realizó una revisión sistemática de la literatura, de los términos MeSH “enfermedad de whipple (whipple Disease) y/o (Tropheryma whipplei), en las bases de datos Pubmed/Medline, Scopus, Scielo y Sciencedirect, Embase, Cochrane Library, BIREME, Proquest y Redalyc; se analizaron 123 artículos.
Resultados: Se analizaron 123 artículos publicados que correspondían a reportes y series de casos en los cuales se evidencio mayor prevalencia en varones (70,6%). La manifestación más frecuente fueron los síntomas articulares (61%), seguida de pérdida de peso (47,1%) y diarrea (43,4%). El método diagnóstico más fue la reacción en cadena polimerasa (PCR) (63,2%), seguida por la biopsia (50.7%); y por último examen anatomopatológico con gránulos PAS (47,8%). El manejo más empleado fue la antibioticoterapia con predominio de trimetoprim sulfametoxazol y ceftriaxona.
Conclusiones: La enfermedad de Whipple tiene una baja prevalencia, se presenta con mayor frecuencia en personas de raza blanca, afecta principalmente a los adultos mayores, además, tiene predilección por el sexo masculino y se caracteriza por ser una enfermedad crónica sistémica con predilección por el aparato digestivo, especialmente el intestino delgado.
Descargas
Referencias bibliográficas
Valdés Álvarez K, Nievas Sánchez M. Enfermedad de Whipple en paciente con fiebre de origen desconocido. Rev Cubana Med. 2018;57(1):33-7.
Dolmans RA, Boel CH, Lacle MM, Kusters JG. Clinical Manifestations, Treatment, and Diagnosis of Tropheryma whipplei Infections. Clin Microbiol Rev. 2017;30(2):529-555. https://doi.org/10.1128/CMR.00033-16
Cardoso J, Gomes L, Santos S, Moreira H, Gomes P, Rua J, et al. Whipple’s disease: A rare cause of malabsorption syndrome. GE Port J Gastroenterol. 2020;27(4):283–9. https://doi.org/10.1159/000504760
Pankl S, Baez M, Young P, Bruetman J, Rausch A, Zubiarurre I, et al. Enfermedad de Whipple e hipertensión pulmonar reversible. Medicina. 2021;81(1):91-95.
Kadian R, Wang J, Freitas E. Could CT abdomen and PET/CT be helpful in early diagnosis of Whipple’s disease? A case report. IDCases. 2021;26(e01286):e01286. https://doi.org/10.1016/j.idcr.2021.e01286
Brönnimann D, Vareil M-O, Sibon I, Lagier J-C, Lepidi H, Puges M, et al. Limbic encephalitis as a relapse of Whipple’s disease with digestive involvement and spondylodiscitis. Infection. 2019;47(4):637-41. https://doi.org/10.1007/s15010-018-1173-x
Lopes A, Santos AF, Alvarenga MJ, Mello E, Silva A. Whipple’s disease: a rare case of malabsorption. BMJ Case Rep. 2018; 2018:bcr2017222955. http://dx.doi.org/10.1136/bcr-2017-222955
Crespo E, Lemus A, Gonzáles S. Enfermedad de Whipple, una causa poco frecuente de diarrea, Rev Ciencias Médicas. 2017. 21(3):133-137.
Parodi R, Ibarzábal J, Román R, Alasino M, Varela M, Díaz S. Enfermedad de Whipple. Comunicación de un caso y revisión de la literatura. Acta Gastroenterológica Latinoamericana. 2019;49(3):229-240.
Kukull B, Mahlow J, Hale G, Perry LJ. Whipple’s disease: a fatal mimic. Autops Case Rep. 2021;11:e2020237. https://doi.org/10.4322/acr.2020.237
Melas N, Amin R, Gyllemark P, Younes AH, Almer S. Whipple’s disease: the great masquerader-a high level of suspicion is the key to diagnosis. BMC Gastroenterol. 2021;21(1):128. https://doi.org/10.1186/s12876-021-01664-1
da Silva GAR, Neto JSP. Whipple’s disease manifested as difficult-to-diagnose polyarthralgia: a case report and literature review. Rev Bras Reumatol Engl Ed. 2017;57(5):483–6. https://doi.org/10.1016/j.rbre.2015.05.003
Turcan S, Tofan-Scutaru L, Istrate V, Tirbu V. Whipple’s disease? A case report and discussion. Med Pharm Rep. 2021;94(Suppl 1):S76-8. https://doi.org/10.15386/mpr-2237
Alsarhani WK, Alkhalifah MI, Alkatan HM, Alsolami AL, Maktabi AMY, Alsuhaibani AH. Whipple’s disease scleral nodules: a novel presentation in 2 consecutive patients. BMC Ophthalmol. 2020;20(1):413. https://doi.org/10.1186/s12886-020-01695-4
Brevet P, Rottenberg P, Viacroze C, Schleifer D, Lequerre T, Vittecoq O. A case of Whipple’s disease mimicking auto-inflammatory disease and revealed by severe right cardiac failure under anakinra. Joint Bone Spine. 2020;87(4):365-6. https://doi.org/10.1016/j.jbspin.2019.11.004
Gruber JR, Sarro R, Delaloye J, Surmely J-F, Siniscalchi G, Tozzi P, et al. Tropheryma whipplei bivalvular endocarditis and polyarthralgia: a case report. J Med Case Rep. 2015;9(1):259. https://doi.org/10.1186/s13256-015-0746-x
Ramos JM, Pasquau F, Galipienso N, Valero B, Navarro A, Martinez A, et al. Whipple’s disease diagnosed during anti-tumor necrosis factor alpha treatment: two case reports and review of the literature. J Med Case Rep. 2015;9(1):165. https://doi.org/10.1186/s13256-015-0632-6
Scheurwater MA, Verduin CM, van Dantzig J-M. Whipple’s endocarditis: a case report of a blood culture-negative endocarditis. Eur Heart J Case Rep. 2019;3(4):1-6. https://doi.org/10.1093/ehjcr/ytz222
Alozie A, Zimpfer A, Köller K, Westphal B, Obliers A, Erbersdobler A, et al. Arthralgia and blood culture-negative endocarditis in middle Age Men suggest tropheryma whipplei infection: report of two cases and review of the literature. BMC Infect Dis. 2015;15(1):339. https://doi.org/10.1186/s12879-015-1078-6
Li W, Zhang Q, Xu Y, Zhang X, Huang Q, Su Z. Severe pneumonia in adults caused by Tropheryma whipplei and Candida sp. infection: a 2019 case series. BMC Pulm Med. 2021;21(1):29. https://doi.org/10.1186/s12890-020-01384-4
McGee M, Brienesse S, Chong B, Levendel A, Lai K. Tropheryma whipplei Endocarditis: Case Presentation and Review of the Literature. Open Forum Infect Dis. 2019;6(1):ofy330. https://doi.org/10.1093/ofid/ofy330
Jos S-L, Angelakis E, Caus T, Raoult D. Positron emission tomography in the diagnosis of Whipple’s endocarditis: a case report. BMC Res Notes. 2015;8(1):56. https://doi.org/10.1186/s13104-015-1022-2
Testi I, Tognon MS, Gupta V. Ocular Whipple disease: Report of three cases. Ocul Immunol Inflamm. 2019;27(7):1117-20. https://doi.org/10.1080/09273948.2018.1518461
Dick J, Krauß P, Hillenkamp J, Kohlmorgen B, Schoen C. Postoperative Tropheryma whipplei endophthalmitis - a case report highlighting the additive value of molecular testing. JMM Case Rep. 2017;4(10):e005124. https://doi.org/10.1099/jmmcr.0.005124
Liersch J, Carlotti A, Theunis A, Leonard A, Barrett M, Carlson JA, et al. Erythema nodosum leprosum-like lesions are a histopathologic pattern in Whipple’s disease and a sign of the immune reconstitution inflammatory syndrome: A case series and review of the literature: A case series and review of the literature. Am J Dermatopathol. 2017;39(4):259-66. https://doi.org/10.1097/DAD.0000000000000641
Vural A, Acar NP, Soylemezoglu F, Oguz KK, Dericioğlu N, Saka E. Isolated central nervous system Whipple’s disease: Two cases. Clin Neurol Neurosurg. 2015;139:91–4. https://doi.org/10.1016/j.clineuro.2015.08.028
Peregrin J, Malikova H. Primary Whipple disease of the brain: case report with long-term clinical and MRI follow-up. Neuropsychiatr Dis Treat. 2015;11:2461–9. https://doi.org/10.2147/NDT.S92066
Karlowee V, Kolakshyapati M, Amatya VJ, Takayasu T, Nosaka R, Sugiyama K, et al. Diffuse leptomeningeal glioneuronal tumor (DLGNT) mimicking Whipple’s disease: a case report and literature review. Childs Nerv Syst. 2017;33(8):1411–4. https://doi.org/10.1007/s00381-017-3405-2
de Saint-Martin G, Urbanski G, Beucher A-B, Ebran J-M. An ophthalmologic complication of Whipple’s disease: Case report. J Fr Ophtalmol. 2018;41(8):e387–9. https://doi.org/10.1016/j.jfo.2017.11.036
Citerne Q, Honstettre S, Ouichka R, Loeuille D, Gillet P, Chary-Valckenaere I. Atypical response of spondyloarthritis to biologics revealing Whipple’s disease: A case-report. Therapie. 2018;73(5):437–9. https://doi.org/doi:10.1016/j.therap.2018.02.008
Sampaio F, Moreira J, Jordão S, Vieira B, Pereira S, Carvalho R. Whipple’s disease orbitopathy: case report and review of literature. Orbit. 2022;41(1):112-117. https://doi.org/10.1080/01676830.2020.1820044
Saraci G. Enfoque diagnóstico de una condición rara: la enfermedad de Whipple. Rev Gastroenterol Méx (Engl Ed). 2020;85(4):477–8. https://doi.org/10.1016/j.rgmx.2020.07.006
Santos Seoane SM, Martínez Gutiérrez R, Venta Menéndez VI. Whipple’s disease: when diarrhea is absent. Rev Esp Enferm Dig. 2019;111(6):492–3. https://doi.org/10.17235/reed.2019.6015/2018
Chou J-W, Hsu B-C, Chang C-H. A rare cause of chronic diarrhea and fever. Gastroenterology. 2020;158(8):e5-6. https://doi.org/10.1053/j.gastro.2020.01.018
Saito H, Shiode J, Ohya S, Yao A, Saito S, Fujii M, et al. Whipple’s disease with long-term endoscopic follow-up. Intern Med. 2018;57(12):1707–13. https://doi.org/10.2169/internalmedicine.9631-17
Damaraju D, Steiner T, Wade J, Gin K, FitzGerald JM. Clinical problem-solving. A surprising cause of chronic cough. N Engl J Med. 2015;373(6):561–6. https://doi.org/10.1056/NEJMcps1303787
Ruggiero E, Zurlo A, Giantin V, Galeazzi F, Mescoli C, Nante G, et al. Short article: Relapsing Whipple’s disease: a case report and literature review. Eur J Gastroenterol Hepatol. 2016;28(3):267–70. https://doi.org/10.1097/MEG.0000000000000539
Guiomar V, Pinto MJ, Gomes C, Correia C, Tavares S, Chaves V, et al. Whipple’s disease as the first manifestation of chronic Lymphocytic leukaemia. Eur J Case Rep Intern Med. 2019;6(10):001270. https://doi.org/10.12890/2019_001270
Fontana M, Cerri S, Bernardelli G, Brugioni L, Clini E, Tonelli R. Unusual effectiveness of systemic steroids in Whipple disease. Pulmonology. 2020;26(6):415-7. https://doi.org/10.1016/j.pulmoe.2020.02.007
Sullivan A, Shrestha P, Basnet S, Herb R, Zagorski E. A rare case of Whipple’s disease with endocarditis in a patient with dextrocardia. SAGE Open Med Case Rep. 2020;8:2050313X20936952. https://doi.org/10.1177/2050313X20936952
Balducci C, Foresti S, Ciervo A, Mancini F, Nastasi G, Marzorati L, et al. Primary Whipple disease of the Central Nervous System presenting with rhombencephalitis. Int J Infect Dis. 2019;88:149–51. https://doi.org/10.1016/j.ijid.2019.08.019
Sid’Amar S, Puppa G. Whipple’s disease affecting ileal Peyer’s patches: The first case report. Case Rep Pathol. 2019;2019:1509745. https://doi.org/10.1155/2019/1509745
Juanmartiñena Fernández JF, Oyón Lara D, Rázquin Lizarraga S, Fernández Urien I. Whipple’s disease under the vision of capsule endoscopy. Rev Esp Enferm Dig. 2016;108(9):606. https://doi.org/10.17235/reed.2016.4362/2016
Bally JF, Méneret A, Roze E, Anderson M, Grabli D, Lang AE. Systematic review of movement disorders and oculomotor abnormalities in Whipple’s disease: Movement Disorders in Whipple’s Disease. Mov Disord. 2018;33(11):1700–11. https://doi.org/10.1002/mds.27419
Priest DH, Grote TH, Staley SL, Berger WS, Norman ES, Smith BS. Secondary immune thrombocytopenia (ITP) as an initial presentation of Whipple’s disease. IDCases. 2018;12:e4–6. https://doi.org/10.1016/j.idcr.2017.05.010
Gaudé M, Tébib J, Puéchal X. Atypical focal forms of Whipple’s disease seen by rheumatologists. Joint Bone Spine. 2015;82(1):56–9. https://doi.org/10.1016/j.jbspin.2014.08.005
Ankli B, Khanlari B, Pegios V, Zettl A, Daikeler T. Whipple’s disease mimicking an auto-inflammatory disease with myositis and soft tissue inflammation. Joint Bone Spine 2018;85(5):645-646. https://doi.org/10.1016/j.jbspin.2018.01.003
Seddon O, Hettiarachchi I. Whipple’s endocarditis presenting as ulnar artery aneurysm; if you don’t look, you won’t find. BMJ Case Rep. 2017;bcr2017221327. https://doi.org/10.1136/bcr-2017-221327
Olano C, Dorelo R, Oricchio M, Mendez D, Canavesi A, Pitetta C. Capsule endoscopy aiding diagnosis of a rare condition - Whipple’s disease. Endoscopy. 2019;51(9):E272-3. https://doi.org/10.1055/a-0896-2269
Totschnig D, Seitz T, Zoufaly A, Hagenauer-Drektraan S, Wenisch C. Whipple’s disease diagnosed in a patient with suspected sarcoidosis. Int J Infect Dis. 2021;106:41–2. https://doi.org/10.1016/j.ijid.2021.03.053
Hamza Bin Waqar S, Diks J, Zaman U, Sharif S, Sheikh T, Kolla S, et al. Refractory effusions, crumbly bones, mystifying cachexia and an absent mind: An unusual presentation of Whipple’s disease with review of literature. Am J Med Case Rep. 2021;9(7):348–53. https://doi.org/10.12691/ajmcr-9-7-2
Loiodice A, Losurdo G, Iannone A, Rossi R, Fiore MG, Piscitelli D. Transmission electron microscopy helpfulness in Whipple’s disease masked by immunosuppressant therapy for arthritis. APMIS. 2018;126(1):92–6. https://doi.org/10.1111/apm.12782
Kono M, Yamamoto K, Nagamatsu M, Kutsuna S. Use of polymerase chain reaction in the diagnosis of Whipple’s disease. J Infect Chemother. 2015;21(12):885-8. https://doi.org/10.1016/j.jiac.2015.08.010
Boban M, Gjadrov-Kuveždić K, Jakić-Razumović J. Cytology of cerebrospinal fluid in CNS Whipple disease. Acta Neurol Belg. 2017;117(4):935-936. https://doi.org/10.1007/s13760-017-0824-5
Wartique L, Lagier JC, Raoult D, Jamilloux Y, Sève P. Mesenteric lymphadenitis as a presenting feature of Whipple’s disease: Value of PCR analysis. Int J Infect Dis. 2018;75:15-17. https://doi.org/10.1016/j.ijid.2018.08.003
Giunchi D, Marcoli N, Deabate L, Delcogliano M, Testa E, Candrian C, et al. Isolated Knee Arthritis as Early and Only Symptom of Whipple’s Disease. Case Rep Med. 2018;2018:3417934. https://doi.org/10.1155/2018/3417934
Kundu A, Sen P, Khurana S. Isolated CNS Whipple’s disease: a diagnostic dilemma. BMJ Case Rep. 2015;2015:bcr2015211784. https://doi.org/10.1136/bcr-2015-211784
Gundling F, Wittenburg H, Tannapfel A, Mossner J. Neurological presentation of Whipple’s disease after long-term antibiotic treatment: a case report. J Med Case Rep. 2008;2:191. https://doi.org/10.1186/1752-1947-2-191
Zhang WM, Xu L. Pulmonary parenchymal involvement caused by Tropheryma whipplei. Open Med (Warsz). 2021;16(1):843–6. https://doi.org/10.1515/med-2021-0297
Zhu B, Tang J, Fang R, Fei X, Wang Q, Wang W, et al. Pulmonary coinfection of Mycobacterium tuberculosis and Tropheryma whipplei: a case report. J Med Case Rep. 2021;15(1):359. https://doi.org/10.1186/s13256-021-02899-y
Obma KL, Marx GE, Mauchley D, Seres T, Babu A, Saveli CC, et al. CASE 12--2015: Tropheryma Whipplei Endocarditis. J Cardiothorac Vasc Anesth. 2015;29(6):1712-6. https://doi.org/10.1053/j.jvca.2014.11.011
Vindigni SM, Taylor J, Quilter LAS, Hyun TS, Liu C, Rosinski SL, et al. Tropheryma whipplei infection (Whipple’s disease) in a patient after liver transplantation. Transpl Infect Dis. 2016;18(4):617–24. https://doi.org/10.1111/tid.12562
Muretti M, Keiralla A, Jeffery K, Krasopoulos G. Tropheryma whipplei endocarditis: An uncommon infection with potentially fatal consequences. J Card Surg. 2020;35(4):923–5. https://doi.org/10.1111/jocs.14467
Heavener T, Thompson M, Patel C, Forrester L, Rawls D. An unusual presentation of Tropheryma whipplei infection. Proc (Bayl Univ Med Cent). 2017;30(4):429–30. https://doi.org/10.1080/08998280.2017.11930215
Lagier JC, Cammilleri S, Raoult D. Classic Whipple’s disease diagnosed by (18)F-fluorodeoxyglucose PET. Lancet Infect Dis. 2016;16(1):130. https://doi.org/10.1016/S1473-3099(15)00503-4
He YT, Peterson K, Crothers J, Dejace J, Hale AJ. Endocarditis and systemic embolization from Whipple’s disease. IDCases. 2021;24(e01105):e01105. https://doi.org/10.1016/j.idcr.2021.e01105
Tatsuki M, Ishige T, Igarashi Y, Hatori R, Hokama A, Hirato J, et al. Whipple disease mimicking inflammatory bowel disease. Intest Res. 2021;19(1):119–25. https://doi.org/10.5217/ir.2019.09177
Sanchez A, Del Giudice P, Mantion C, Mazellier S, Boukari F, Roger P-M, et al. Erythematous skin nodules during treatment of Whipple’s disease. Med Mal Infect. 2021;51(4):397–9. https://doi.org/10.1016/j.medmal.2020.10.006
Yan J, Zhang B, Zhang Z, Shi J, Liu S, Qi J, et al. Case report: Tropheryma whipplei hide in an AIDS patient with Pneumocystis pneumonia. Front Public Health. 2021;9:663093. https://doi.org/10.3389/fpubh.2021.663093
Branquinho DF, Pinto-Gouveia M, Mendes S, Sofia C. From past sailors’ eras to the present day: scurvy as a surprising manifestation of an uncommon gastrointestinal disease. BMJ Case Rep. 2015;2015:bcr2015210744. ttps://doi.org/10.1136/bcr-2015-210744
Rezk A, Gunnerson AC, Komar M. A disease that is often missed without gastrointestinal symptoms. Gastroenterology. 2016;150(5):1096–7. https://doi.org/10.1053/j.gastro.2015.11.054
Chizinga M, Schiliro D, Mullin B, Barrie RL. Mesenteric lymphadenitis as a presenting feature of Whipple’s disease. IDCases. 2017;9:50-2. https://doi.org/10.1016/j.idcr.2017.06.002
De Francesco V, Corsi F, Pennella A, Bellesia A, Fiorini G, Vaira D, et al. Whipple’s disease: case report and review of the literature. J Gastrointestin Liver Dis. 2018;27(3):331–6. https://doi.org/10.15403/jgld.2014.1121.273.fra
Henriques MS de M, da Paz AR, Gaertner ABP, Melo CI, Filgueiras PL, Jerome RA. Deep vein thrombosis as initial manifestation of Whipple disease. Case Rep Gastroenterol. 2016;10(3):640–5. https://doi.org/10.1159/000452206
Parkash V, Mudhar HS, Wagner BE, Raoult D, Batty R, Lepidi H, et al. Bilateral ocular myositis associated with Whipple’s disease. Ocul Oncol Pathol. 2017;3(1):17–21. https://doi.org/10.1159/000448622
Kilani M, Njim L, Nsir AB, Hattab MN. Whipple disease presenting as cystic brain tumor: Case report and review of the literature. Turk Neurosurg. 2018;28(3):495–9. https://doi.org/10.5137/1019-5149.JTN.17111-16.2
Puéchal X, London J. Clinical image: Whipple’s destructive septic arthritis. Arthritis rheumatol. 2017;69(3):559. https://doi.org/10.1002/art.39999
Elfanagely Y, Jamot S, Dapaah-Afriyie K, Fine S. Whipple’s disease mimicking common digestive disorders. R I Med J (2013). 2021;104(4):43–5.
Papakonstantinou D, Riste MJ, Langman G, Moran E. Misdiagnosing Whipple’s disease in the young. BMJ Case Rep. 2017;2017:bcr2016218866. https://doi.org/10.1136/bcr-2016-218866
Dubost J-J, Couderc M, Mathieu S, Tournadre A, Soubrier M. Chronic bursitis and tenosynovitis revealing Whipple’s disease. Joint Bone Spine. 2020;87(5):481–2. https://doi.org/10.1016/j.jbspin.2020.01.010
Sarvananthan S, Velissaris T, Miskolczi S, Yam T, Shah BN. Tropheryma whipplei endocarditis. Echocardiography. 2021;38(4):697–700. https://doi.org/10.1111/echo.15007
Vayssade M, Tournadre A, D’Incan M, Soubrier M, Dubost J-J. Immune reconstitution inflammatory syndrome during treatment of Whipple’s disease. Joint Bone Spine. 2015;82(2):122–4. https://doi.org/10.1016/j.jbspin.2014.09.002
Quartuccio L, Giovannini I, Pizzolitto S, Scarpa M, De Vita S. Seronegative arthritis and Whipple disease: Risk of misdiagnosis in the era of biologic agents. Case Rep Rheumatol. 2019;2019:3410468. https://doi.org/10.1155/2019/3410468
Emonet S, Wuillemin T, Harbarth S, Wassilew N, Cikirikcioglu M, Schrenzel J, et al. Relapse of Tropheryma whipplei endocarditis treated by trimethoprim/sulfamethoxazole, cured by hydroxychloroquine plus doxycycline. Int J Infect Dis. 2015;30:17–9. https://doi.org/10.1016/j.ijid.2014.11.003
Moreno García MS, Casorrán Berges M, Del Río-Martínez PS, Bosque Peralta MT. The great unknown, Whipple’s disease. Reumatol Clin. 2017;13(4):243–4. https://doi.org/10.1016/j.reuma.2016.08.002
Van der Bent S, van Vugt M, Amir A, van der Wal A, Mekkes J. Cutaneous manifestations in treated Whipple’s disease. Int J Dermatol. 2017;56(4):e82-e84. https://doi.org/10.1111/ijd.13479
Chiu M, Moore S. Bilateral optic disc swelling in Whipple’s disease: Letter to the Editor. Clin Experiment Ophthalmol. 2017;45(6):641–3. https://doi.org/10.1111/ceo.12933
Van Bockstal M, Hoorens A, Van den Bosch F, Creytens D, Verbeke S, Van Dorpe J. Whipple’s disease in granulomatous disguise: a challenging diagnosis with many histopathological pitfalls. Virchows Arch. 2017;470(4):465–8. https://doi.org/10.1007/s00428-017-2084-4
Aamar A, Madhani K, Anwar MS, Singh P, Garsten J. Whipple’s disease manifested as recurrent ascites. Cureus. 2017;9(3):e1108. https://doi.org/10.7759/cureus.1108
Chandra SR, Raj P, Pai AR, Reddy N. A case of Whipple’s disease: A very rare cause for rapidly progressive dementia. Indian J Psychol Med. 2018;40(3):280–3. https://doi.org/10.4103/IJPSYM.IJPSYM_149_17
Fernández-Mondelo J, Cervero-Jiménez M. Forma atípica de presentación de la enfermedad de Whipple. Reporte de un caso. Rev Esp Casos Clin Med Intern (RECCMI). 2018;3(2):56-58.
Brönnimann D, Vandenhende M-A, Viallard J-F. Gamma delta T cell expansion in Whipple’s disease with muscular granulomatous vasculitis. Infection. 2018;46(4):573-6. https://doi.org/10.1007/s15010-018-1143-3
Herráez A, Valmaseda M, Chao M, Reinoso M. Manifestaciones neuropsiquiátricas de la enfermedad de Whipple en una adolescente: a propósito de un caso. Dig Liver Dis. 2018;27(2):92-5.
Methotrexate: Masking and worsening of Whipple’s disease: case report. React Wkly. 2018;1692(1):224. https://doi.org/10.1007/s40278-018-42751-4
Kutlu O, Erhan SS, Gökden Y, Kandemir O, Tükekc T. Whipple’s Disease: A Case Report. Med Princ Pract. 2020; 29(1):90-93. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7024871/
Loiodice A. The conundrum of arthritis and chronic diarrhea could be unveiled as Whipple’s disease. Dig Liver Dis. 2017;2:3-10. https://doi.org/10.1016/S1590-8658(17)30459-0
Bosa L. Tropheryma whipplei infection in a pediatric kidney transplanted patient: A case report. Dig Liver Dis. 2017;49(4):E257. https://doi.org/10.1016/j.dld.2017.09.041
Herbette M, Cren JB, Joffres L, Lucas C, Ricard E, Salliot C, et al. Usefulness of polymerase chain reaction for diagnosing Whipple’s disease in rheumatology. PLoS ONE. 2018;13(7):e0200645. https://doi.org/10.1371/journal.pone.0200645
Maciorkowska M, Ustymowicz, Zakrzewski M, Pryczynicz A, Markowski A, Romatowski J, et al. Whipple’s disease as a systemic infectious disease – a case presentation. Prog Health Sci. 2018;8(1):212-218. https://doi.org/10.5604/01.3001.0012.1332
Delarbre D, Gan L, Antoine C, Poisnel E, Cambon A, Dutasta F, et al. Difficultés diagnostiques de la maladie de Whipple au cours des rhumatismes inflammatoires chroniques: trois observations. La Revue de Médecine Interne. 2021;42(11):801-804.
Lenfant M, Callemeyn J, Alerts H, Meersseman W, Van Moerkercke W. Whipple’s disease in a man of north african descent: Case report and brief review of the literature. Acta Gastroenterol Belg. 2019;82(1):83-86.
Thornton S, Wang Y, Köebel M, Bernard K, Burdz T, Maitland A, et al. Another Whipple’s triad? Pericardial, myocardial and valvular disease in an unusual case presentation from a Canadian perspective. BMC Cardiovascular Disorders. 2019;19(1):312. https://doi.org/10.1186/s12872-019-1257-2
Spoerl D, Bär D, Cooper J, Vogt T, Tyndall A, Walker UA. Multisegmental spondylitis due to Tropheryma whipplei: case report. Orphanet J Rare Dis. 2019;4:13. https://doi.org/10.1186/1750-1172-4-13
Le Blay P, Rakotonirain H, Lagier JC, Raoult D, Puechal X, Pers YM. A severe Whipple disease with an immune reconstitution inflammatory syndrome: an additional case of thalidomide efficiency. Joint Bone Spine. 2014;81(3):260-2. https://doi.org/10.1016/j.jbspin.2013.10.007
Fenollar F, Nicoli F, Paquet C, Lepidi H, Cozzone P, Antoine J-C, et al. Progressive dementia associated with ataxia or obesity in patients with Tropheryma whipplei encephalitis. BMC Infect Dis. 2018;11:171.
Erak P, Murillo D. Enfermedad de Whipple: presentación clínica sin afección articular. Rev Clin Esc Med. 2019;9(4):64-68.
Hujoel IA, Johnson DH, Lebwohl B, Leffler D, Kupfer S, Wu TT, et al. Tropheryma whipplei Infection (Whipple Disease) in the USA. Dig Dis Sci. 2019;64(1):213-223. https://doi.org/10.1007/s10620-018-5033-4
Lenfant M, Callemeyn J, Alaerts H, Meersseman W, Van Moerkercke W. Whipple’s disease in a man of North African descent: case report and brief review of the literature. Acta Gastroenterol Belg. 2019;82(1):83-86.
Kutlua O, Şengiz Erhanb S, Gökdena Y, Kandemira O, Tükekc T. Whipple’s Disease: A Case Report. Med Princ Pract 2020;29(1):90-93. https://doi.org/10.1159/000498909
Aguiar A, Gomes P, Curvo-Semedo L, Donato P. Whipple’s disease: imaging contribution for a challenging case. BMJ Case Rep. 2020;13(2):e233071. https://doi.org/10.1136/bcr-2019-233071
Al-Hamoudi W, Habbab F, Nudo C, Nahal A, Flegel K. Eosinophilic vasculitis: a rare presentation of Whipple’s disease. Can J Gastroenterol. 2017;21(3):189-91.
Verbrugghe L, Verraes K, Vanderschueren S, Vermeire S, Pollet S, De Leyn P, et al. Mesenteric panniculitis as a presentation of Whipple›s disease: case report and review of the literature. Acta Gastroenterol Belg. 2020;83(4):666-668.
Olivier M, Licitra C, Field Z, Ge L, Hill D, Madruga M, et al. Thrombocytopenia and endocarditis in a patient with Whipple’s disease: case report. BMC Infect Dis. 2020;20(1):71. https://doi.org/10.1186/s12879-020-4799-0
Rey R, Orozco L, Marrugo K, Lopez R, Perez E, De la Hoz J, et al. Whipple disease diagnosed by enteroscopy: first case report in Colombia of an underdiagnosed disease and literature review. BMC Gastroenterol. 2020;20(1):197. https://doi.org/10.1186/s12876-020-01302-2
Foteinogiannopoulou K, Mouzas I, Tzardi M, Orfanoudaki E, Theodoraki E, Kofteridis D. First case of Whipple’s disease successfully treated with tigecycline. Germs. 2021;11(1):105-110. https://doi.org/10.18683/germs.2021.1246
Hofmann P, Durisch N, Buetikofer C, Helmchen B. Granulomatous lung disease and immune reconstitution inflammatory syndrome in Whipple’s disease. BMJ Case Rep. 2021;14(6):e243633. https://doi.org/10.1136/bcr-2021-243633
Tandon P, Huang V, Jaffer N, Kirsch R, Croitoru K. A rare presentation of hypovolemic shock secondary to Whipple’s disease. Eur J Gastroenterol Hepatol. 2019;31(5):642-5. https://doi.org/10.1097/MEG.0000000000001363
Descargas
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |













