Characterization of Achalasia Subtypes Based on High-Resolution Manometry in Patients at a Reference Hospital in Colombia
DOI:
https://doi.org/10.22516/25007440.1017Keywords:
Achalasia, High-resolution esophageal manometry, DysphagiaAbstract
Introduction: Limited information is available regarding the clinical and manometric characteristics of different subtypes of achalasia. This study aims to describe these characteristics in patients treated at a prominent hospital in Colombia.
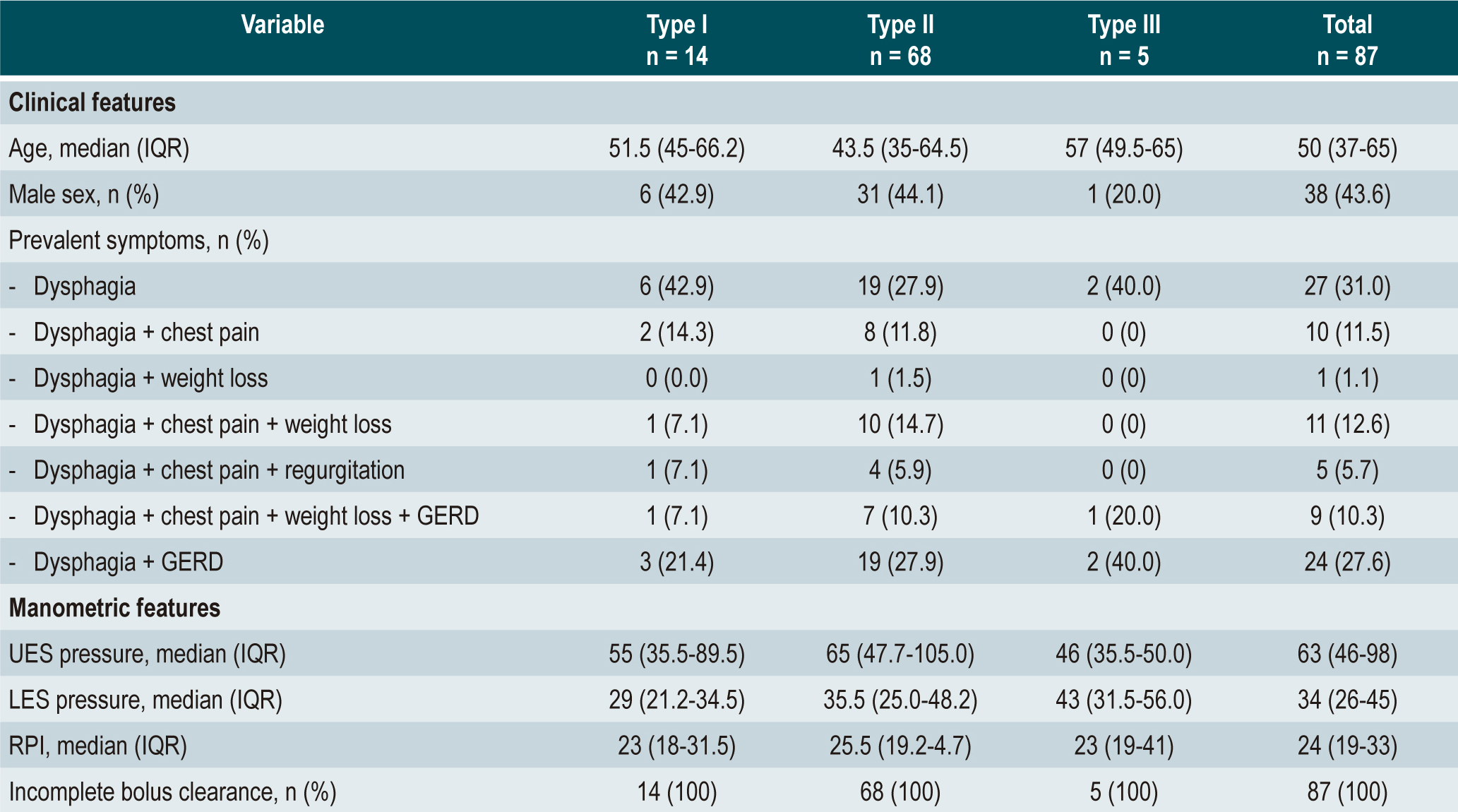
Methods: This descriptive observational study included patients diagnosed with achalasia using high-resolution esophageal manometry at Hospital Universitario San Ignacio in Bogotá, Colombia, between 2016 and 2020. We documented the clinical manifestations, manometric findings, treatment approaches, and response to treatment based on the subtype of achalasia.
Results: A total of 87 patients were enrolled, with a median age of 51 years, and 56.4% of them were female. The majority had type II achalasia (78.1%), followed by type I (16%) and type III (5.7%). All patients presented with dysphagia, 40.2% experienced chest pain, and 27.6% had gastroesophageal reflux. The clinical parameters, including integrated relaxation pressure value (IRP; median: 24 mmHg, interquartile range [IQR]: 19-33), upper esophageal sphincter pressure (UES; median: 63 mmHg, IQR: 46-98), and lower esophageal sphincter pressure (LES; median: 34 mm Hg, IQR: 26-45), were similar across the different subtypes. Esophageal clearance was incomplete in all patients. Among the 35 patients who received intervention, Heller’s myotomy was the most commonly employed procedure (68.5%), followed by esophageal dilation (28.6%). All patients experienced symptomatic improvement, with a median pre-treatment Eckardt score of 5 (IQR: 5-6) and a post-treatment score of 1 (IQR: 1-2).
Conclusions: Type II achalasia is the most prevalent subtype. The clinical and manometric findings, as well as treatment response, exhibit similarities among the different subtypes of achalasia. In Colombia, the outcomes of this condition align with those reported in other parts of the world.
Downloads
References
Savarino E, Bhatia S, Roman S, Sifrim D, Tack J, Thompson SK, et al. Achalasia. Nat Rev Dis Prim. 2022;8(1):28. https://doi.org/10.1038/s41572-022-00356-8
Vela MF, Richter JE, Wachsberger D, et al. Complexities of managing achalasia at a tertiary referral center: use of pneumatic dilatation, Heller myotomy, and botulinum toxin injection. Am J Gastroenterol 2004;99:1029-36. https://doi.org/10.1111/j.1572-0241.2004.30199.x
Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013;108(8):1238-49. https://doi.org/10.1038/ajg.2013.196
Khashab MA, Vela MF, et al. ASGE guideline on the management of acalasia Gastrointest Endosc 2020;91:213-27. https://doi.org/10.1016/j.gie.2019.04.231
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil Off J Eur Gastrointest Motil Soc. 2015;27(2):160 - 74. https://doi.org/10.1111/nmo.12477
Hani A, Bernal W. Leguízamo A, Zuluaga C, Vargas R, Vergara H, et al. Cómo realizar e interpretar una manometría esofágica de alta resolución usando la clasificación de Chicago 3.0. Revista Colombiana de Gastroenterología. 2017;32:369-78. doi: 10.22516/25007440.181. https://doi.org/10.22516/25007440.181
Hani A, Leguízamo A, Carvajal J, Mosquera-Klinger G, Costa V. Cómo realizar e interpretar una manometría esofágica de alta resolución. Revista Colombiana de Gastroenterología. 2015;30:74-83. https://doi.org/10.22516/25007440.25
Zhou MJ, Kamal A, Freedberg DE, Markowitz D, Clarke JO, Jodorkovsky D. Type II Achalasia Is Increasing in Prevalence. Dig Dis Sci [Internet]. 2021;66(10):3490-4. https://doi.org/10.1007/s10620-020-06668-7
Fisichella PM, Raz D, Palazzo F, Niponmick I, Patti MG. Clinical, radiological, and manometric profile in 145 patients with untreated achalasia. World J Surg. 2008;32(9):1974-9. https://doi.org/10.1007/s00268-008-9656-z
Khoudari G, Saleh MA, Sarmini MT, Parikh MP, Vega KJ, Sanaka MR. The Prevalence and Epidemiology of Achalasia in the USA: A Population-Based Study. Off JAm Coll Gastroenterol | ACG [Internet]. 2019;114. https://doi.org/10.14309/01.ajg.0000591384.93014.6c
Ren Y, Tang X, Chen Y, Chen F, Zou Y, Deng Z, Wu J, Li Y, Huang S, Jiang B, Gong W. Pre-treatment Eckardt score is a simple factor for predicting one-year peroral endoscopic myotomy failure in patients with achalasia. Surg Endosc. 2017;31(8):3234-3241. https://doi.org/10.1007/s00464-016-5352-5
Gockel I, Junginger T. The value of scoring achalasia: a comparison of current systems and the impact on treatment--the surgeon's viewpoint. Am Surg. 2007; 73(4):327-31. https://doi.org/10.1177/000313480707300403
Panesso-Gómez S, Pavia P, Rodríguez-Mantilla IE, et al. Detección de Trypanosoma cruzi en pacientes colombianos con diagnóstico de acalasia esofágica. Am J Trop Med Hyg. 2018; 98 (3): 717-723. https://doi.org/10.4269/ajtmh.17-0417
Roman S, Zerbib F, Queneherve L, et al. The Chicago classification for achalasia in a French multicentric cohort.Dig Liver Dis. 2012; 44 : 976-980. https://doi.org/10.1016/j.dld.2012.07.019
Oude Nijhuis RAB, Zaninotto G, Roman S, Boeckxstaens GE, et al. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United European Gastroenterol J. 2020;8(1):13-33. https://doi.org/10.1177/2050640620903213
Meillier A, Midani D, Caroline D, Saadi M, Parkman H, Schey R, Difference of achalasia subtypes based on clinical symptoms, radiographic findings, and stasis scores. Revista de Gastroenterología de México (English Edition). 2018. 83 (1); 3-8. https://doi.org/10.1016/j.rgmxen.2017.03.013
Jung HK, Hong SJ, Lee OY, Pandolfino J, Park H, et al. Korean Society of Neurogastroenterology and Motility. 2019 Seoul Consensus on Esophageal Achalasia Guidelines. J Neurogastroenterol Motil. 2020;26(2):180-203. https://doi.org/10.5056/jnm20014
Fox M, Sweis R, Yadlapati R, Pandolfino J, Hani A, et al. Chicago Classification version 4.0 © Technical Review: Update on Standard High Resolution Manometry Protocol for the Assessment of Esophageal Motility. 2021 Neurogastroenterol Motil. 2021 ;33(4): e14120. https://doi.org/10.1111/nmo.14120
Yadlapati R, Kahrilas PJ, Fox MR, Hani A, Pandolfino JE, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021 Jan;33(1):e14058. doi: 10.1111/nmo.14058. Erratum in: Neurogastroenterol Motil. 2022;:e14179.
Rohof, W. O., Salvador, R., Annese, V., Bruley des Varannes, S., Chaussade, S., Costantini, M., Elizalde, J. et al .Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology. 2013 ; 144(4): 718-e14. https://doi.org/10.1053/j.gastro.2012.12.027
Ou, Y. H., Nie, X. M., Li, L. F., Wei, Z. J., & Jiang, B. High-resolution manometric subtypes as a predictive factor for the treatment of achalasia: A meta-analysis and systematic review. Journal of digestive diseases; 2016; 17(4): 222-235. https://doi.org/10.1111/1751-2980.12327
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














