Disorders of Gut-Brain Interaction (Functional Gastrointestinal Disorders): Neuromodulators in Clinical Practice (Part I)
DOI:
https://doi.org/10.22516/25007440.1132Keywords:
Antidepressants, antipsychotics, central neuromodulators, disorders of gut brain interaction, functional gastrointestinal disorderAbstract
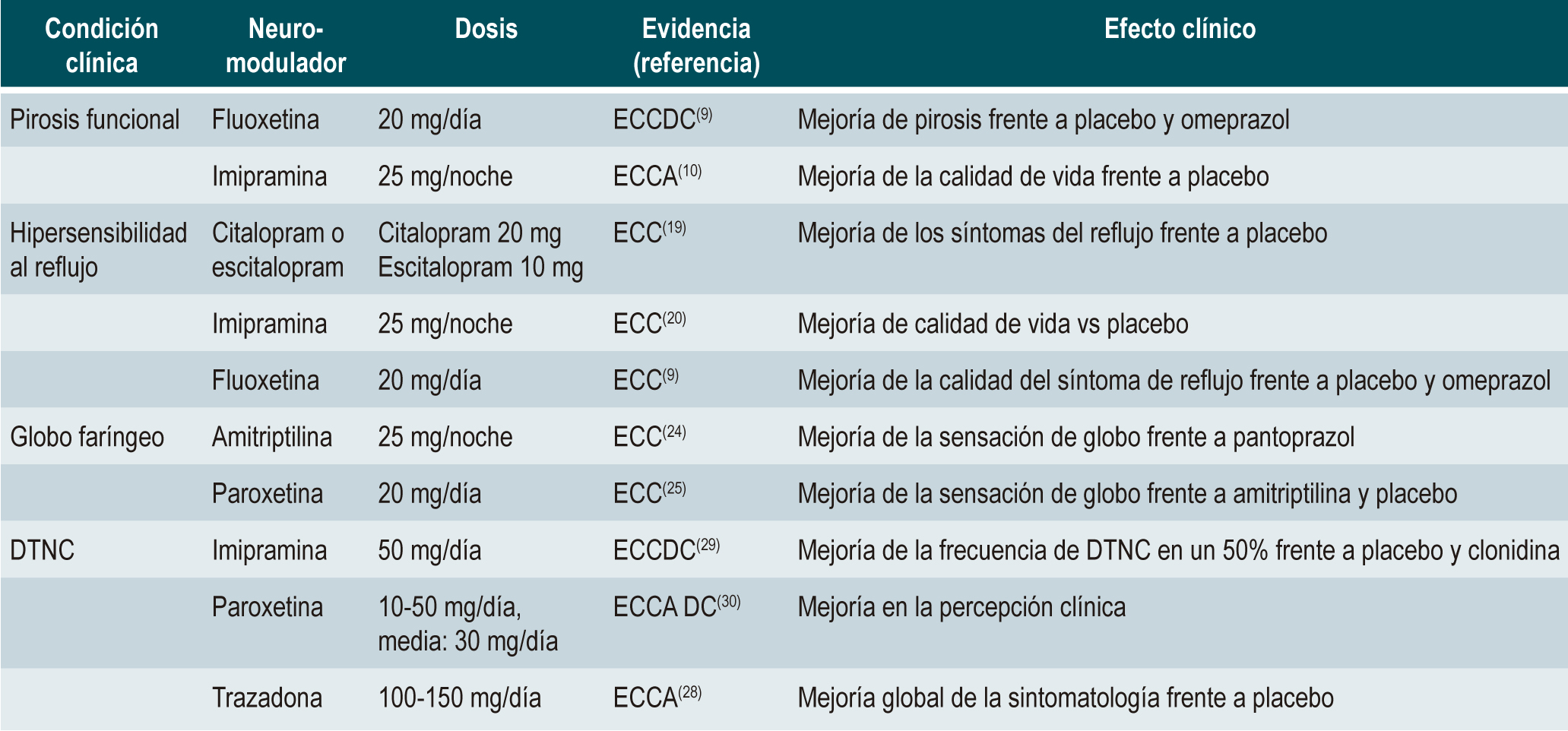
Introduction: This review article develops the basic principles for the use and action mechanisms of neuromodulators applied in clinical practice and their role in treating different disorders of gutbrain interaction (DGBI), particularly, esophageal disorders in part I.
Materials and methods: The working group reviewed the most frequent pathologies and medications used according to the most recent literature and presented those with the best clinical evidence in each case.
Results: Due to the diversity of disorders, types of studies, and therapeutic options, we decided to present the evidence with the best results for each case. We determined the doses used, their results, and the side effects of each one.
Conclusions: The basic principles of the use and mechanisms of action of the main neuromodulators were reviewed, including their use in this section in the main esophageal gastrointestinal functional disorders. Given that the available evidence is not definitive, more controlled clinical trials are needed for each condition to confirm the effectiveness and safety of neuromodulators.
Downloads
References
Drossman DA. Presidential address: Gastrointestinal illness and the biopsychosocial model. Psychosom Med. 1998;60(3):258-67. https://doi.org/10.1097/00006842-199805000-00007
Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016;150(6):1262-1279.e2. https://doi.org/10.1053/j.gastro.2016.02.032
Drossman DA, Tack J, Ford AC, Szigethy E, Törnblom H, Van Oudenhove L. Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gut-Brain Interaction): A Rome Foundation Working Team Report. Gastroenterology. 2018;154(4):1140-1171.e1. https://doi.org/10.1053/j.gastro.2017.11.279
Elbe D. Stahl’s Essential Psychopharmacology: Neuroscientific Basis and Practical Applications, Third Edition. J Can Acad Child Adolesc Psychiatry. 2010;19(3):230.
Törnblom H, Drossman DA. Centrally targeted pharmacotherapy for chronic abdominal pain. Neurogastroenterol Motil. 2015;27(4):455-67. https://doi.org/10.1111/nmo.12509
Lunn MPT, Hughes RAC, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev. 2014;2014(1):CD007115. https://doi.org/10.1002/14651858.CD007115.pub3
Gale JD, Houghton LA. Alpha 2 Delta (α(2)δ) Ligands, Gabapentin and Pregabalin: What is the Evidence for Potential Use of These Ligands in Irritable Bowel Syndrome. Front Pharmacol. 2011;2:28. https://doi.org/10.3389/fphar.2011.00028
Aziz Q, Fass R, Gyawali CP, Miwa H, Pandolfino JE, Zerbib F. Functional Esophageal Disorders. Gastroenterology. 2016;150(6):1368-79. https://doi.org/10.1053/j.gastro.2016.02.012
Ostovaneh MR, Saeidi B, Hajifathalian K, Farrokhi-Khajeh-Pasha Y, Fotouhi A, Mirbagheri SS, et al. Comparing omeprazole with fluoxetine for treatment of patients with heartburn and normal endoscopy who failed once daily proton pump inhibitors: double-blind placebo-controlled trial. Neurogastroenterol Motil. 2014;26(5):670-8. https://doi.org/10.1111/nmo.12313
Limsrivilai J, Charatcharoenwitthaya P, Pausawasdi N, Leelakusolvong S. Imipramine for Treatment of Esophageal Hypersensitivity and Functional Heartburn: A Randomized Placebo-Controlled Trial. Am J Gastroenterol. 2016;111(2):217-24. https://doi.org/10.1038/ajg.2015.413
Savarino E, Marabotto E, Zentilin P, Frazzoni M, Sammito G, Bonfanti D, et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig Liver Dis. 2011;43(7):542-7. https://doi.org/10.1016/j.dld.2011.01.016
Savarino E, Zentilin P, Tutuian R, Pohl D, Casa DD, Frazzoni M, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103(11):2685-93. https://doi.org/10.1111/j.1572-0241.2008.02119.x
Watson RGP, Tham TCK, Johnston BT, McDougall NI. Double blind cross-over placebo controlled study of omeprazole in the treatment of patients with reflux symptoms and physiological levels of acid reflux--the “sensitive oesophagus.” Gut. 1997;40(5):587-90. https://doi.org/10.1136/gut.40.5.587
Zerbib F, Belhocine K, Simon M, Capdepont M, Mion F, Des Varannes SB, et al. Clinical, but not oesophageal pH-impedance, profiles predict response to proton pump inhibitors in gastro-oesophageal reflux disease. Gut. 2012;61(4):501-6. https://doi.org/10.1136/gutjnl-2011-300798
Sawada A, Sifrim D, Fujiwara Y. Esophageal Reflux Hypersensitivity: A Comprehensive Review. Gut Liver. 2023;17(6):831-842. https://doi.org/10.5009/gnl220373
Hoshikawa Y, Hoshino S, Kawami N, Iwakiri K. Prevalence of behavioral disorders in patients with vonoprazan-refractory reflux symptoms. J Gastroenterol. 2021;56(2):117-124. https://doi.org/10.1007/s00535-020-01751-2
Yadlapati R, Gyawali CP, Pandolfino JE, Chang K, Kahrilas PJ, Katz PO, et al. AGA Clinical Practice Update on the Personalized Approach to the Evaluation and Management of GERD: Expert Review. Clin Gastroenterol Hepatol. 2022;20(5):984-994.e1. https://doi.org/10.1016/j.cgh.2022.01.025
Spechler SJ, Hunter JG, Jones KM, Lee R, Smith BR, Mashimo H, et al. Randomized Trial of Medical versus Surgical Treatment for Refractory Heartburn. N Engl J Med. 2019;381(16):1513-23. https://doi.org/10.1056/NEJMoa1811424
Limsrivilai J, Charatcharoenwitthaya P, Pausawasdi N, Leelakusolvong S. Imipramine for Treatment of Esophageal Hypersensitivity and Functional Heartburn: A Randomized Placebo-Controlled Trial. Am J Gastroenterol. 2016;111(2):217-24. https://doi.org/10.1038/ajg.2015.413
Viazis N, Keyoglou A, Kanellopoulos AK, Karamanolis G, Vlachogiannakos J, Triantafyllou K, et al. Selective serotonin reuptake inhibitors for the treatment of hypersensitive esophagus: a randomized, double-blind, placebo-controlled study. Am J Gastroenterol. 2012;107(11):1662-7. https://doi.org/10.1038/ajg.2011.179
Zerbib F, Rommel N, Pandolfino J, Gyawali CP. ESNM/ANMS Review. Diagnosis and management of globus sensation: A clinical challenge. Neurogastroenterol Motil. 2020;32(9):e13850. https://doi.org/10.1111/nmo.13850
Brown SR, Schwartz JM, Summergrad P, Jenike MA. Globus hystericus syndrome responsive to antidepressants. Am J Psychiatry. 1986;143(7):917-8. https://doi.org/10.1176/ajp.143.7.917
Kiebles JL, Kwiatek MA, Pandolfino JE, Kahrilas PJ, Keefer L. Do patients with globus sensation respond to hypnotically assisted relaxation therapy? A case series report. Dis Esophagus. 2010;23(7):545-53. https://doi.org/10.1111/j.1442-2050.2010.01064.x
Khalil HS, Bridger MW, Hilton-Pierce M, Vincent J. The use of speech therapy in the treatment of globus pharyngeus patients. A randomised controlled trial. Rev Laryngol Otol Rhinol (Bord). 2003;124(3):187-90.25. You LQ, Liu J, Jia L, Jiang SM, Wang GQ. Effect of low-dose amitriptyline on globus pharyngeus and its side effects. World J Gastroenterol. 2013;19(42):7455-60. https://doi.org/10.3748/wjg.v19.i42.7455
Zhou WC, Jia L, Chen DY, Liu Y, Liu J, Jiang SM, et al. The effects of paroxetine and amitriptyline on the upper esophageal sphincter (UES) pressure and its natural history in globus pharyngeus. Dig Liver Dis. 2017;49(7):757-763. https://doi.org/10.1016/j.dld.2017.02.00827. Yamasaki T, Fass R. Reflux Hypersensitivity: A New Functional Esophageal Disorder. J Neurogastroenterol Motil. 2017;23(4):495-503. https://doi.org/10.5056/jnm17097
Shibli F, Tawil J, Fass R. Diagnosis and Management of Functional Chest Pain in the Rome IV Era. J Neurogastroenterol Motil. 2019;25(4):487-98. https://doi.org/10.5056/jnm19146
George N, Abdallah J, Maradey-Romero C, Gerson L, Fass R. Review article: the current treatment of non-cardiac chest pain. Aliment Pharmacol Ther. 2016;43(2):213-39. https://doi.org/10.1111/apt.13458
Nguyen TMT, Eslick GD. Systematic review: The treatment of noncardiac chest pain with antidepressants. Aliment Pharmacol Ther. 2012;35(5):493-500. https://doi.org/10.1111/j.1365-2036.2011.04978.x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |
















