Endoscopic retrograde cholangiopancreatography at a leading cancer center
DOI:
https://doi.org/10.22516/25007440.512Keywords:
Endoscopic cholangiopancreatography, cancer, reference centerAbstract
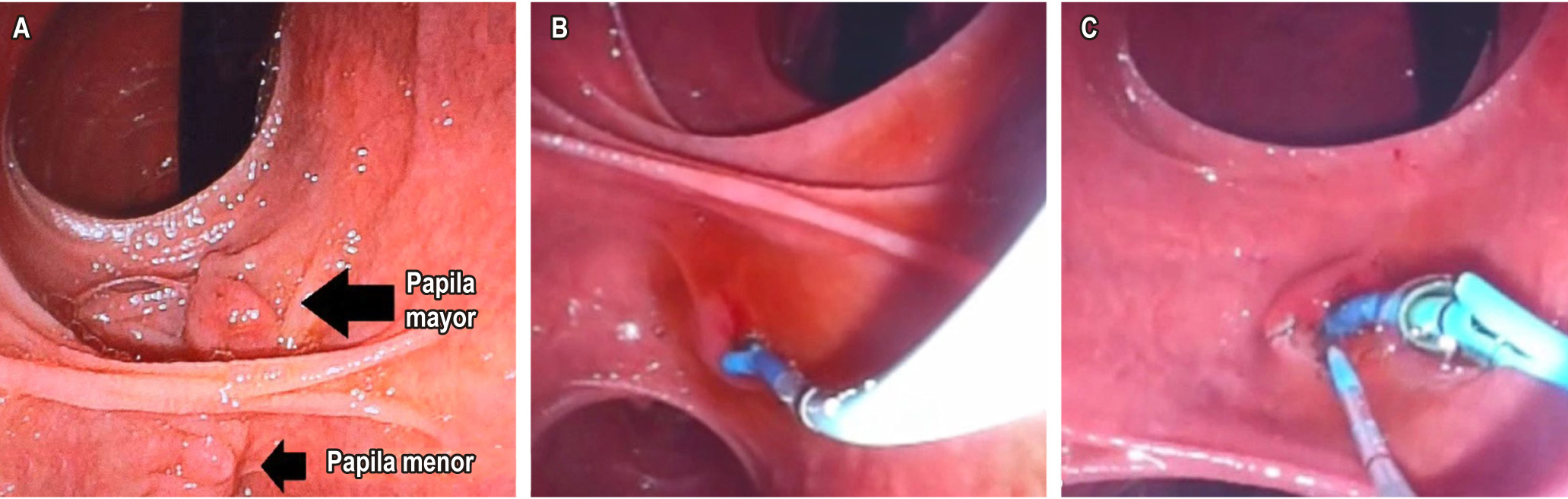
Introduction: Endoscopy is one of the tools necessary to treat biliary and pancreatic diseases. Endoscopic retrograde cholangiopancreatography (ERCP) is one of the most technically demanding procedures with the highest risk of complications when treating hepato-pancreato-biliary disorders.
Objective: To characterize the clinical outcomes of ERCP patients in a cancer patient center. Methodology: Observational, retrospective, descriptive case series study based on clinical data of patients brought to ERCP in a population diagnosed with cancer of different primary origins and in different stages of the disease from January 2010 to January 2017.
Results: A total of 255 procedures were analyzed. The female sex was predominant with 140 cases (54.9%), and the average age was 62.9 years (SD 12.9 years). All procedures were done with therapeutic intent. The most frequent indication was pancreatic cancer (N=47; 18.43%), extrinsic compression of the common bile duct (N=42; 16.47%), biliary prosthesis dysfunction (N=36; 14.12%), cholecystocholedocholithiasis (N=32; 12. 55%), other causes (N=32; 12.55%), gallbladder cancer (N=24; 9.41%), extrahepatic cholangiocarcinoma (N=21; 8.24%), recurrent choledocholithiasis (N=9; 3.53%), residual choledocholithiasis (N=6; 2.35%), and Klatskin tumor (N=6; 2.35%). Successful cannulation was reported in 222 cases (87.06%). During the procedure, 10 patients presented complications (4.3%), with pancreatitis and perforations being the most frequent (N=3; 1.18%), followed by bleeding, cholangitis (N=2; 0.78%), and post-ERCP pain (N=1; 0.39%). Conclusions: In the population studied, the principal reasons for performing the procedure were related to cancer. The frequency of successful cannulation and complications reported here are similar to other results in the general population.
Downloads
References
McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167(5):752-6.
https://doi.org/10.1097/00000658-196805000-00013
NIH state of the science statement on endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and therapy. NIH Consens State Sci Statements. 2002 Jan 14-16;19(1):1-26.
Kutty RS, Westaby D, Martin JP, Vlavianos P, Andreyev HJN. What are the Gastrointestinal Endoscopic Requirements of a Cancer Centre? Clinical Oncology (2007) 19: 330e332.
https://doi.org/10.1016/j.clon.2007.03.008
Freeman ML. Adverse outcomes of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin N Am. 2003;13(4):775-98, xi.
https://doi.org/10.1016/S1052-5157(03)00107-7
Baillie J. Endoscopic therapy in acute recurrent pancreatitis. World J Gastroenterol. 2008;14(7):1034-7.
https://doi.org/10.3748/wjg.14.1034
Donnellan F, Byrne MF. Prevention of Post-ERCP Pancreatitis. Gastroenterol Res Pract. 2012;2012:796751.
https://doi.org/10.1155/2012/796751
Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20(4):148-51.
https://doi.org/10.1016/S0016-5107(74)73914-1
Pineda LF, Arbeláez Méndez V, Gómez Zuleta M, Daza J, Siado Cantillo A, Aponte PN, Brando C, Ortiz C, Saavedra S, González R. Estudio comparativo entre papilotomía endoscópica intraoperatoria y papilotomía endoscópica convencional para el tratamiento de la coledocolitiasis. Rev Col Gastroenterol. 2007;22(4):272-82.
Baillie J. ERCP training: for the few, not for all. Gut. 1999;45(1):9-10
https://doi.org/10.1136/gut.45.1.9
Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP, Jr., Montes H, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56(5):652-6.
https://doi.org/10.1016/S0016-5107(02)70112-0
https://doi.org/10.1067/mge.2002.129086
ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ,
Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc.
;85(1):32-47.
https://doi.org/10.1016/j.gie.2016.06.051
Kochar B, Akshintala VS, Afghani E, Elmunzer BJ, Kim KJ, Lennon AM, Khashab MA, Kalloo AN, Singh VK.
Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastrointest Endosc. 2015;81(1):143-149.e9.
https://doi.org/10.1016/j.gie.2014.06.045
Shanmugarajah I, Solhaug M, Aslam O, Reiertsen O. Efficacy and safety assessment of ERCP in patients with
malignant biliary obstruction. Acta Gastroenterol Belg. 2017;80(4):487-91.
Cohen ME, Slezak L, Wells CK, Andersen DK, Topazian M. Prediction of bile duct stones and complications in
gallstone pancreatitis using early laboratory trends. Am J Gastroenterol. 2001;96(12):3305-11.
https://doi.org/10.1111/j.1572-0241.2001.05330.x
Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232(2):191-8.
https://doi.org/10.1097/00000658-200008000-00007
Penaloza-Ramirez A, Leal-Buitrago C, Rodriguez-Hernandez A. Adverse events of ERCP at San Jose
Hospital of Bogota (Colombia). Rev Esp Enferm Dig. 2009;101(12):837-49.
https://doi.org/10.4321/S1130-01082009001200003
Peng C, Nietert PJ, Cotton PB, Lackland DT, Romagnuolo J. Predicting native papilla biliary cannulation success using a multinational Endoscopic Retrograde Cholangiopancreatography (ERCP) Quality Network.
BMC Gastroenterol. 2013;13:147.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















