Mesh migration into the gastroesophageal junction: a rare complication of giant hiatal hernia repair
DOI:
https://doi.org/10.22516/25007440.683Keywords:
Giant hiatal hernia, Hiatal hernia repair, Prosthetic mesh, Esophageal migrationAbstract
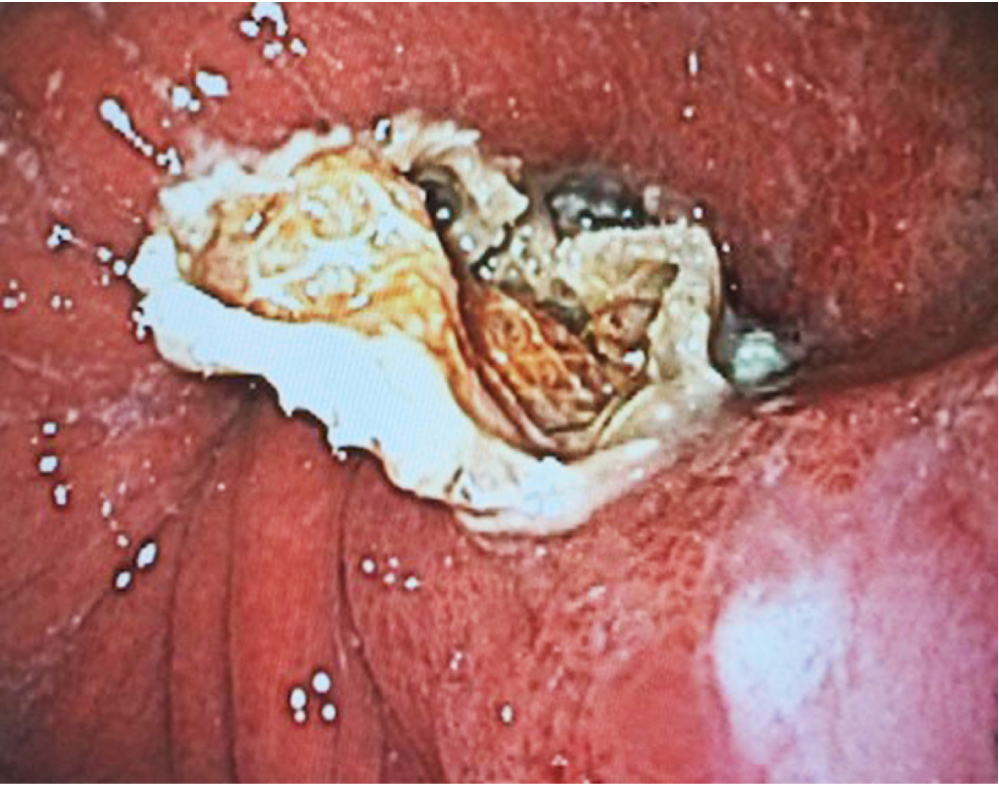
Hiatal hernia repair has been a subject of debate due to the possible associated complications that have changed over the years. The literature reports up to 30% of cases with complications associated with the procedure. Complications other than recurrence and long-term complications are rare and reported in less than 9% of cases. The migration of the prosthetic mesh into the esophagus is a rare complication and only a few cases have been reported. The factors associated with this outcome include prosthetic material, surgical technique, and mesh tension on the intervened tissue. However, it is difficult to establish direct associations of each factor since the current literature has only case reports.
The following is a clinical case of a patient in whom the prosthetic material migrated into the esophagus after a hiatal hernia repair with mesh. The diagnosis and treatment offered are discussed.
Downloads
References
Mittal SK, Shah P. Current Readings: Failed Hiatal Hernia Repair. Semin Thorac Cardiovasc Surg. 2014;26(4):331-4. https://doi.org/10.1053/j.semtcvs.2015.01.002
Kohn GP, Price RR, DeMeester SR, Zehetner J, Muensterer OJ, Awad Z, Mittal SK, Richardson WS, Stefanidis D, Fanelli RD; SAGES Guidelines Committee. Guidelines for the management of hiatal hernia. Surg Endosc. 2013;27(12):4409-28. https://doi.org/10.1007/s00464-013-3173-3.
Chilintseva N, Brigand C, Meyer C, Rohr S. Chirurgie laparoscopique des hernies hiatales de grande taille avec renforcement prothétique de l’hiatus œsophagien. J Chir Viscerale. 2012;149(3):235-40. https://doi.org/10.1016/j.jchirv.2011.12.008
Braghetto I, Csendes A, Korn O, Musleh M, Lanzarini E, Saure A, Hananias B, Valladares H. Hernias hiatales: ¿cuándo y por qué deben ser operadas? [Hiatal hernias: why and how should they be surgically treated]. Cir Esp. 2013;91(7):438-43. https://doi.org/10.1016/j.cireng.2012.07.004
Prassas D, Rolfs TM, Schumacher FJ. Laparoscopic repair of giant hiatal hernia. A single center experience. Int J Surg. 2015;20:149-52. https://doi.org/10.1016/j.ijsu.2015.06.067
Sathasivam R, Bussa G, Viswanath Y, Obuobi RB, Gill T, Reddy A, Shanmugam V, Gilliam A, Thambi P. ‹Mesh hiatal hernioplasty› versus ‹suture cruroplasty› in laparoscopic para-oesophageal hernia surgery; a systematic review and meta-analysis. Asian J Surg. 2019;42(1):53-60. https://doi.org/10.1016/j.asjsur.2018.05.001
Tam V, Winger DG, Nason KS. A systematic review and meta-analysis of mesh vs suture cruroplasty in laparoscopic large hiatal hernia repair. Am J Surg. 2016;211(1):226-38. https://doi.org/10.1016/j.amjsurg.2015.07.007
Petersen LF, McChesney SL, Daly SC, Millikan KW, Myers JA, Luu MB. Permanent mesh results in long-term symptom improvement and patient satisfaction without increasing adverse outcomes in hiatal hernia repair. Am J Surg. 2014;207(3):445-8. https://doi.org/10.1016/j.amjsurg.2013.09.014
Oleynikov D, Jolley JM. Paraesophageal hernia. Surg Clin North Am. 2015;95(3):555-65. https://doi.org/10.1016/j.suc.2015.02.008
Rochefort M, Wee JO. Management of the Difficult Hiatal Hernia. Thorac Surg Clin. 2018;28(4):533-539. https://doi.org/10.1016/j.thorsurg.2018.07.001
Priego-Jiménez P, Salvador-Sanchís JL, Ángel V, Escrig-Sos J. Short-term results for laparoscopic repair of large paraesophageal hiatal hernias with Gore Bio A® mesh. Int J Surg. 2014;12(8):794-7. https://doi.org/10.1016/j.ijsu.2014.06.001
Jiménez AEP, Aguirre MEP, Campos AR, Eguizabal PT, Torres AJ, Serrano ID, Sánchez-Pernaute A. 658 - Management of Erosion of Hiatal Mesh into the Gastroesophageal Lumen. Gastroenterology. 2018;154(6):S-1274.
https://doi.org/10.1016/S0016-5085(18)34186-6
Müller-Stich BP, Köninger J, Müller-Stich BH, Schäfer F, Warschkow R, Mehrabi A, Gutt CN. Laparoscopic mesh-augmented hiatoplasty as a method to treat gastroesophageal reflux without fundoplication: single-center experience with 306 consecutive patients. Am J Surg. 2009;198(1):17-24. https://doi.org/10.1016/j.amjsurg.2008.07.050
Coluccio G, Ponzio S, Ambu V, Tramontano R, Cuomo G. Dislocazione nel lume cardiale di protesi in PTFE utilizzata per il trattamento di voluminosa ernia jatale da scivolamento. Descrizione di un caso clinico [Dislocation into the cardial lumen of a PTFE prosthesis used in the treatment of voluminous hiatal sliding hernia, A case report]. Minerva Chir. 2000;55(5):341-345.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














