Initial experience with endoscopic ultrasound-guided biliary drainage via choledochoduodenostomy (EUS-CDS) in malignant biliary obstruction in a reference hospital in Colombia
DOI:
https://doi.org/10.22516/25007440.723Keywords:
Endosonography, Interventional endoscopy, Drainage, Bile ducts, Obstructive jaundiceAbstract
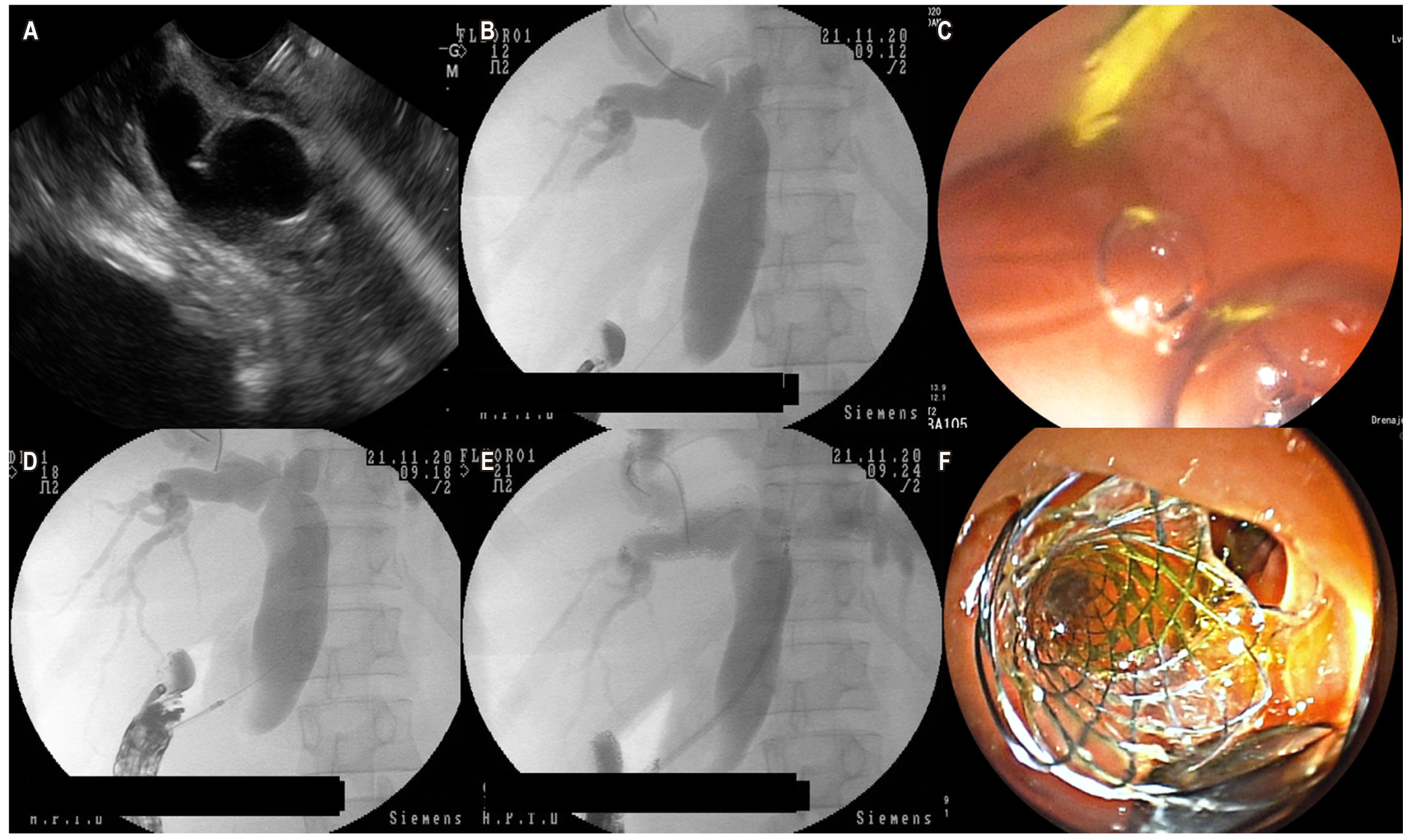
Introduction: Patients with malignant biliary distal obstruction who cannot be treated with endoscopic retrograde cholangiopancreatography (ERCP) or who had a failed ERCP, can find alternative treatment in endoscopic ultrasound-guided biliary drainage via choledochoduodenostomy. EUS-CDS performs with high rates of technical and clinical success and with low rates of morbimortality. Moreover, this method could have the potential to improve the patient’s quality of life, compared with percutaneous or surgical means.
Objective: This study aims to describe the initial experience with endoscopic ultrasound-guided biliary drainage in patients with malignant biliary distal obstruction in a reference center.
Methods: Retrospective case review of six patients with malignant biliary obstruction and prior ERCP-placed and failed. Endoscopic ultrasound-guided biliary drainage via choledochoduodenostomy was performed as an alternative method. Technical and clinical success rates, adverse event rates, dysfunction rates, and patient survival time were described.
Results: 6 cases were analyzed with a higher proportion of female patients, with a mean age of 71,8 ± 19,8 years. The symptoms were related to pancreas adenocarcinoma, periampullary tumor, and distal cholangiocarcinoma. The procedure was technically successful in 100% of cases and clinically successful in 83% of cases. Serious adverse events were nor reported. After 30 days, a survival rate of 66,7 % was observed.
Conclusion: Choledochoduodenostomy is a viable, safe, and effective method in patients with malignant biliary obstruction who had a failed ERCP, and it has high rates of technical and clinical success.
Downloads
References
Pu LZ, Singh R, Loong CK, de Moura EG. Malignant Biliary Obstruction: Evidence for Best Practice. Gastroenterol Res Pract. 2016;2016:3296801. https://doi.org/10.1155/2016/3296801
Forero EA, Galasso D, Bories E, Giovannini M. Derivaciones biliopancreáticas guiadas por ultrasonido endoscópico: descripción de caso y revisión de la literatura. Rev Colomb Gastroenterol. 2013;28(4):339-351.
Minaga K, Takenaka M, Yamao K, Kamata K, Omoto S, Nakai A, Yamazaki T, Okamoto A, Ishikawa R, Yoshikawa T, Chiba Y, Watanabe T, Kudo M. Clinical utility of treatment method conversion during single-session endoscopic ultrasound-guided biliary drainage. World J Gastroenterol. 2020;26(9):947-959. https://doi.org/10.3748/wjg.v26.i9.947
Mora Soler AM, Álvarez Delgado A, Piñero Pérez MC, Velasco-Guardado A, Marcos Prieto H, Rodríguez Pérez A. Endoscopic ultrasound-guided choledochoduodenostomy after a failed or impossible ERCP. Rev Esp Enferm Dig. 2018;110(5):299-305. https://doi.org/10.17235/reed.2018.5040/2017
Artifon EL, Marson FP, Gaidhane M, Kahaleh M, Otoch JP. Hepaticogastrostomy or choledochoduodenostomy for distal malignant biliary obstruction after failed ERCP: is there any difference? Gastrointest Endosc. 2015;81(4):950-9. https://doi.org/10.1016/j.gie.2014.09.047
Perez-Miranda M, de la Serna C, Diez-Redondo P, Vila JJ. Endosonography-guided cholangiopancreatography as a salvage drainage procedure for obstructed biliary and pancreatic ducts. World J Gastrointest Endosc. 2010;2(6):212-22. https://doi.org/10.4253/wjge.v2.i6.212
de Benito Sanz M, Nájera-Muñoz R, de la Serna-Higuera C, Fuentes-Valenzuela E, Fanjul I, Chavarría C, García-Alonso FJ, Sanchez-Ocana R, Carbajo AY, Bazaga S, Perez-Miranda M. Lumen apposing metal stents versus tubular self-expandable metal stents for endoscopic ultrasound-guided choledochoduodenostomy in malignant biliary obstruction. Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-08179-y
Cazacu IM, Singh BS, Saftoiu A, Bhutani MS. Recent developments in hepatopancreatobiliary EUS. Endosc Ultrasound. 2019;8(3):146-150. https://doi.org/10.4103/eus.eus_20_19
Park JK, Woo YS, Noh DH, Yang JI, Bae SY, Yun HS, Lee JK, Lee KT, Lee KH. Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: prospective randomized controlled study. Gastrointest Endosc. 2018;88(2):277-282. https://doi.org/10.1016/j.gie.2018.03.015
Nussbaum JS, Kumta NA. Endoscopic Ultrasound-Guided Biliary Drainage. Gastrointest Endosc Clin N Am. 2019;29(2):277-291. https://doi.org/10.1016/j.giec.2018.11.005
Artifon EL, Aparicio D, Paione JB, Lo SK, Bordini A, Rabello C, Otoch JP, Gupta K. Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol. 2012;46(9):768-74. https://doi.org/10.1097/MCG.0b013e31825f264c
Beissert M, Wittenberg G, Sandstede J, Beer M, Tschammler A, Burghardt W, Jahns R, Hahn D. Metallic stents and plastic endoprostheses in percutaneous treatment of biliary obstruction. Z Gastroenterol. 2002;40(7):503-10. https://doi.org/10.1055/s-2002-32806
Speer AG, Cotton PB, Russell RC, Mason RR, Hatfield AR, Leung JW, MacRae KD, Houghton J, Lennon CA. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet. 1987;2(8550):57-62. https://doi.org/10.1016/s0140-6736(87)92733-4
Piñol V, Castells A, Bordas JM, Real MI, Llach J, Montañà X, Feu F, Navarro S. Percutaneous self-expanding metal stents versus endoscopic polyethylene endoprostheses for treating malignant biliary obstruction: randomized clinical trial. Radiology. 2002;225(1):27-34. https://doi.org/10.1148/radiol.2243011517
Artifon ELA, Ferreira FC, Otoch JP. Coledocoduodenostomía guiada por ultrasonido endoscópico para la paliación de la obstrucción biliar distal maligna. Rev Gastroenterol Mex. 2012;77(1):31-37.
Dhir V, Isayama H, Itoi T, Almadi M, Siripun A, Teoh AYB, Ho KY. Endoscopic ultrasonography-guided biliary and pancreatic duct interventions. Dig Endosc. 2017;29(4):472-485. https://doi.org/10.1111/den.12818
Rimbaş M, Larghi A. Endoscopic Ultrasonography-Guided Techniques for Accessing and Draining the Biliary System and the Pancreatic Duct. Gastrointest Endosc Clin N Am. 2017;27(4):681-705. https://doi.org/10.1016/j.giec.2017.06.006
Logiudice FP, Bernardo WM, Galetti F, Sagae VM, Matsubayashi CO, Madruga Neto AC, Brunaldi VO, de Moura DTH, Franzini T, Cheng S, Matuguma SE, de Moura EGH. Endoscopic ultrasound-guided vs endoscopic retrograde cholangiopancreatography biliary drainage for obstructed distal malignant biliary strictures: A systematic review and meta-analysis. World J Gastrointest Endosc. 2019;11(4):281-291. https://doi.org/10.4253/wjge.v11.i4.281
Itoi T, Isayama H, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Tsuji S, Ishii K, Ikeuchi N, Tanaka R, Umeda J, Moriyasu F, Kawakami H. Stent selection and tips on placement technique of EUS-guided biliary drainage: transduodenal and transgastric stenting. J Hepatobiliary Pancreat Sci. 2011;18(5):664-72. https://doi.org/10.1007/s00534-011-0410-9
Villaverde A, Pizzala JE, Oria IC, Manazzoni D, Abecia V, Mahler MA, Urgiles D, Marcolongo M. Drenaje biliar guiado por ultrasonografía endoscópica en la obstrucción biliar maligna, experiencia inicial en un centro de Argentina. Serie de casos. Acta Gastroenterol Latinoam. 2020;50(3):279-84.
Siddiqui AA, Sreenarasimhaiah J, Lara LF, Harford W, Lee C, Eloubeidi MA. Endoscopic ultrasound-guided transduodenal placement of a fully covered metal stent for palliative biliary drainage in patients with malignant biliary obstruction. Surg Endosc. 2011;25(2):549-55. https://doi.org/10.1007/s00464-010-1216-6
Anderloni A, Fugazza A, Troncone E, Auriemma F, Carrara S, Semeraro R, Maselli R, Di Leo M, D’Amico F, Sethi A, Repici A. Single-stage EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction. Gastrointest Endosc. 2019;89(1):69-76. https://doi.org/10.1016/j.gie.2018.08.047
Tonozuka R, Itoi T, Sofuni A, Itokawa F, Moriyasu F. Endoscopic double stenting for the treatment of malignant biliary and duodenal obstruction due to pancreatic cancer. Dig Endosc. 2013;25 Suppl 2:100-8.
https://doi.org/10.1111/den.12063
Yoon WJ, Park DH, Choi JH, Jang S, Samarasena J, Lee TH, Paik WH, Oh D, Song TJ, Choi JH, Hara K, Iwashita T, Perez-Miranda M, Lee JG, Vazquez-Sequeiros E, Naitoh I, Vila JJ, Brugge WR, Takenaka M, Lee SS, Seo DW, Lee SK, Kim MH. The underutilization of EUS-guided biliary drainage: Perception of endoscopists in the East and West. Endosc Ultrasound. 2019;8(3):188-193. https://doi.org/10.4103/eus.eus_57_18
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














