Percutaneous transgastric approach in pancreatic ductal disruption: Case series
DOI:
https://doi.org/10.22516/25007440.725Keywords:
Acute necrotizing Pancreatitis, Minimally invasive surgical procedures, pancreatic duct, pancreatic pseudocyst, pancreatic fistulaAbstract
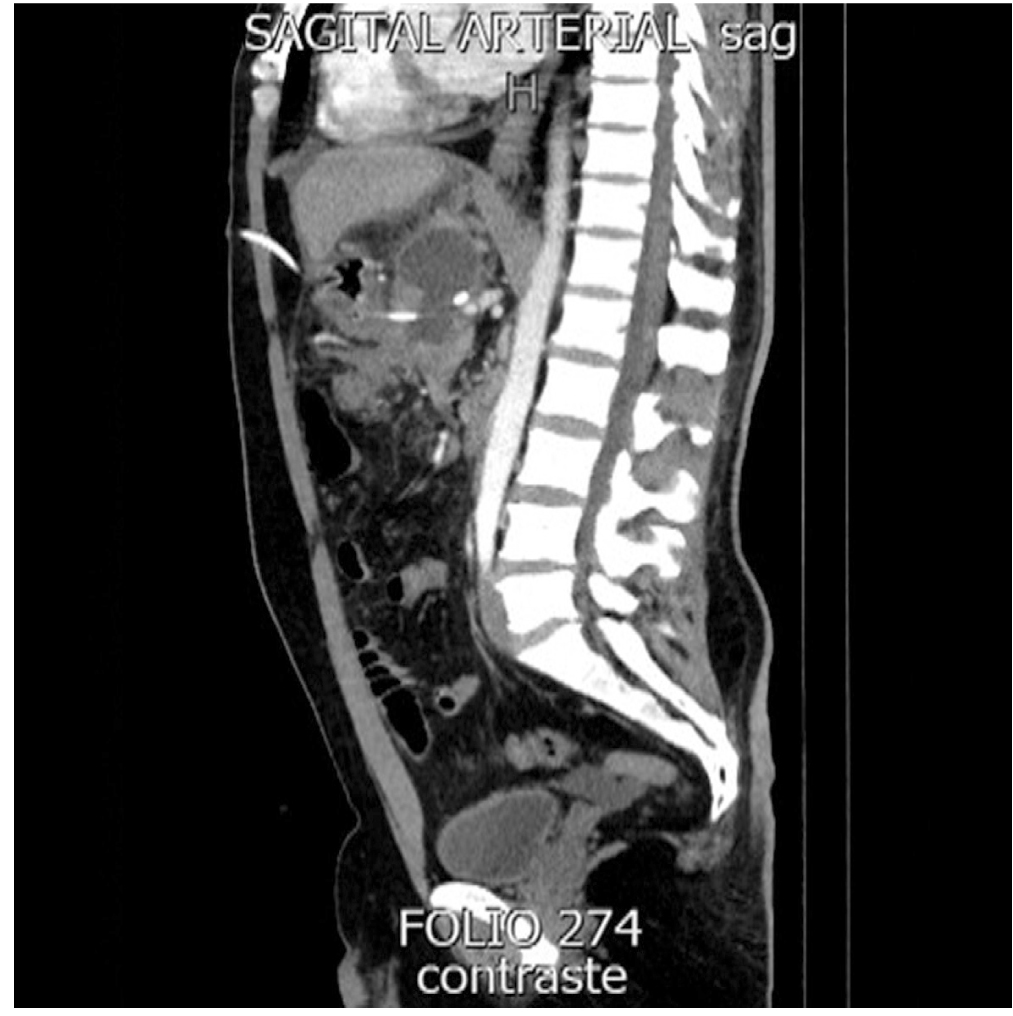
A total of six patients with pancreatic ductal disruption (PDD), treated with image-guided endoscopy percutaneous drainage were enrolled. Initially, patients had infected pancreatic necrosis, treated with transgastric percutaneous drainage, and after the infection was controlled, they developed PDD. In the imaging study process, four patients were diagnosed with partial duct disruption and two patients with complete duct disruption. In both cases the placement of a percutaneous transgastric prosthesis to drain the pancreatic fluids to the stomach was indicated. The prosthesis remained 183 days on average and there were no mortality cases. This therapeutic minimally invasive alternative has low rates of morbimortality and thus, the endoscopy percutaneous transgastric approach is considered as a viable treatment in PPD.
Downloads
References
Timmerhuis H, Boxhoorn L, Besselink M, Bollen T, Bruno M, Joseph Elmunzer B, Fockens P, Horvath KD, Verdonk RC, van Santvoort HC, Voermans RP . Diagnosis and Treatment of Pancreatic Duct Disruption or Disconnection: an International Expert Survey and Case Vignette Study. Endoscopy. 2020;52(S 01):S124. https://doi.org/10.1055/s-0040-1704381
Ramia JM, Fabregat J, Pérez-Miranda M, Figueras J. Síndrome del ducto pancreático desconectado [Disconnected panreatic duct syndrome]. Cir Esp. 2014;92(1):4-10. https://doi.org/10.1016/j.ciresp.2013.02.024
Murage KP, Ball CG, Zyromski NJ, Nakeeb A, Ocampo C, Sandrasegaran K, Howard TJ. Clinical framework to guide operative decision making in disconnected left pancreatic remnant (DLPR) following acute or chronic pancreatitis. Surgery. 2010;148(4):847-56; discussion 856-7. https://doi.org/10.1016/j.surg.2010.07.039
Varadarajulu S, Wilcox CM. Endoscopic placement of permanent indwelling transmural stents in disconnected pancreatic duct syndrome: does benefit outweigh the risks? Gastrointest Endosc. 2011;74(6):1408-12. doi: 10.1016/j.gie.2011.07.049. https://doi.org/10.1016/j.gie.2011.07.049
Veillette G, Dominguez I, Ferrone C, Thayer SP, McGrath D, Warshaw AL, Fernández-del Castillo C. Implications and management of pancreatic fistulas following pancreaticoduodenectomy: the Massachusetts General Hospital experience. Arch Surg. 2008;143(5):476-81. https://doi.org/10.1001/archsurg.143.5.476
Rana SS, Sharma R, Sharma V, Chhabra P, Gupta R, Bhasin DK. Prevention of recurrence of fluid collections in walled off pancreatic necrosis and disconnected pancreatic duct syndrome: Comparative study of one versus two long term transmural stents. Pancreatology. 2016;16(4):687-8. https://doi.org/10.1016/j.pan.2016.05.009
Irani S, Gluck M, Ross A, Gan SI, Crane R, Brandabur JJ, Hauptmann E, Fotoohi M, Kozarek RA. Resolving external pancreatic fistulas in patients with disconnected pancreatic duct syndrome: using rendezvous techniques to avoid surgery (with video). Gastrointest Endosc. 2012;76(3):586-93.e1-3. https://doi.org/10.1016/j.gie.2012.05.006
Bang JY, Wilcox CM, Navaneethan U, Hasan MK, Peter S, Christein J, Hawes R, Varadarajulu S. Impact of Disconnected Pancreatic Duct Syndrome on the Endoscopic Management of Pancreatic Fluid Collections. Ann Surg. 2018;267(3):561-568. https://doi.org/10.1097/SLA.0000000000002082
Mouli VP, Sreenivas V, Garg PK. Efficacy of conservative treatment, without necrosectomy, for infected pancreatic necrosis: a systematic review and meta-analysis. Gastroenterology. 2013;144(2):333-340.e2. https://doi.org/10.1053/j.gastro.2012.10.004
van Baal MC, van Santvoort HC, Bollen TL, Bakker OJ, Besselink MG, Gooszen HG; Dutch Pancreatitis Study Group. Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis. Br J Surg. 2011;98(1):18-27. https://doi.org/10.1002/bjs.7304
van Brunschot S, Fockens P, Bakker OJ, Besselink MG, Voermans RP, Poley JW, Gooszen HG, Bruno M, van Santvoort HC. Endoscopic transluminal necrosectomy in necrotising pancreatitis: a systematic review. Surg Endosc. 2014;28(5):1425-38. https://doi.org/10.1007/s00464-013-3382-9
van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, van Goor H, Schaapherder AF, van Eijck CH, Bollen TL, van Ramshorst B, Nieuwenhuijs VB, Timmer R, Laméris JS, Kruyt PM, Manusama ER, van der Harst E, van der Schelling GP, Karsten T, Hesselink EJ, van Laarhoven CJ, Rosman C, Bosscha K, de Wit RJ, Houdijk AP, van Leeuwen MS, Buskens E, Gooszen HG; Dutch Pancreatitis Study Group. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med. 2010;362(16):1491-502. https://doi.org/10.1056/NEJMoa0908821
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














