Esophageal and Pulmonary Involvement Caused by Paracoccidioidomycosis in Immunocompromised Patient: Case Report
DOI:
https://doi.org/10.22516/25007440.798Keywords:
Paracoccidioidomycosis, Blastomycosis, Invasive fungal infectionsAbstract
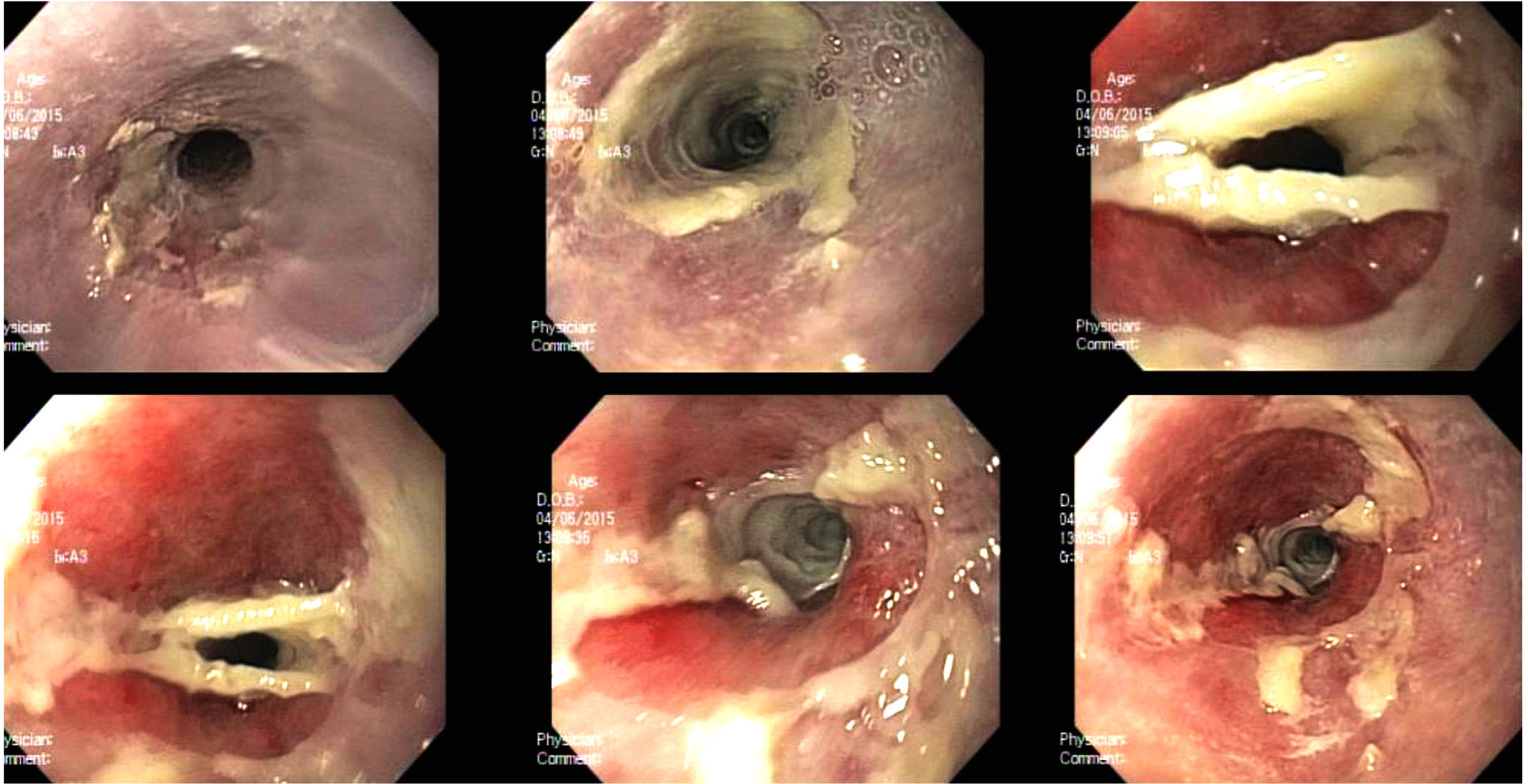
Paracoccidioidomycosis (PCM) is a fungal infection endemic to South America. It predominantly affects men, depending on their work field: farmers and agriculturists. Paracoccidioidomycosis is caused by the aspiration of the fungus in its micellar form and manifests in three conditions: acute, subacute, and chronic; the latter is more frequent in adults, whose treatment will depend on azoles, amphotericin B, and sulfonamides. This case concerns a 57-year-old Colombian man, a farmer with no pathological history who showed dysphagia for solids that progressed to liquids, sialorrhea, and weight loss for two months. He underwent upper GI endoscopy, and whitish lesions were observed; thus, he was biopsied, displaying yeasts in multiple gemmations compatible with paracoccidioidomycosis. In turn, a chest CT scan showed generalized interstitial parenchymal involvement. Subsequently, he was treated with itraconazole, showing improvement and resolution in his clinical picture. Since the pathology described is endemic in South America and can be disseminated in immunocompromised patients. Given the broad infection spectrum, consideration should be given to patients with risk factors, symptomatology, and findings in extension studies suggesting this disease to provide timely and specific treatment.
Downloads
References
Restrepo A, Gómez BL, Tobón A. Paracoccidioidomycosis: Latin America’s Own Fungal Disorder. Curr Fungal Infect Rep. 2012;6(4):303-11. https://doi.org/10.1007/s12281-012-0114-x
Sifuentes-Osornio J, Corzo-León DE, Ponce-de-León LA. Epidemiology of Invasive Fungal Infections in Latin America. Curr Fungal Infect Rep. 2012;6(1):23-34. https://doi.org/10.1007/s12281-011-0081-7
Mendes RP, Cavalcante RS, Marques SA, Marques MEA, Venturini J, Sylvestre TF, et al. Paracoccidioidomycosis: Current Perspectives from Brazil. Open Microbiol J. 2017;11:224-282. https://doi.org/10.2174/1874285801711010224
Teixeira MM, Theodoro RC, Nino-Vega G, Bagagli E, Felipe MSS. Paracoccidioides species complex: ecology, phylogeny, sexual reproduction, and virulence. PLoS Pathog. 2014;10(10):e1004397. https://doi.org/10.1371/journal.ppat.1004397
Teixeira M de M, Theodoro RC, Oliveira FFM de, Machado GC, Hahn RC, Bagagli E, et al. Paracoccidioides lutzii sp. nov.: biological and clinical implications. Med Mycol. Oxford University Press; 2014;52(1):19-28.
Da Costa MM, Marques da Silva SH. Epidemiology, Clinical, and Therapeutic Aspects of Paracoccidioidomycosis. Curr Trop Med Reports. 2014;1:138-44. https://doi.org/10.1007/s40475-014-0013-z
Costa AN, Benard G, Albuquerque ALP, Fujita CL, Magri ASK, Salge JM, et al. The lung in paracoccidioidomycosis: new insights into old problems. Clinics (Sao Paulo). 2013;68(4):441-8. https://doi.org/10.6061/clinics/2013(04)02
Bocca AL, Amaral AC, Teixeira MM, Sato PK, Sato P, Shikanai-Yasuda MA, et al. Paracoccidioidomycosis: eco-epidemiology, taxonomy and clinical and therapeutic issues. Future Microbiol. Future Microbiol. 2013;8(9):1177-91. https://doi.org/10.2217/fmb.13.68
Bicalho RN, Santo MF, de Aguiar MC, Santos VR. Oral paracoccidioidomycosis: a retrospective study of 62 Brazilian patients. Oral Dis. 2001;7(1):56-60. https://doi.org/10.1034/j.1601-0825.2001.70111.x
Silva CO, Almeida AS, Pereira AA, Sallum AW, Hanemann JA, Tatakis DN. Gingival involvement in oral paracoccidioidomycosis. J Periodontol. 2007;78(7):1229-34. https://doi.org/10.1902/jop.2007.060490
Godoy H, Reichart PA. Oral manifestations of paracoccidioidomycosis. Report of 21 cases from Argentina. Mycoses. 2003;46(9-10):412-7. https://doi.org/10.1046/j.0933-7407.2003.00917.x
Sant’Anna GD, Mauri M, Arrarte JL, Camargo H Jr. Laryngeal manifestations of paracoccidioidomycosis (South American blastomycosis). Arch Otolaryngol Head Neck Surg. 1999;125(12):1375-8. https://doi.org/10.1001/archotol.125.12.1375
Borges SR, Silva GM, Chambela Mda C, Oliveira Rde V, Costa RL, Wanke B, et al. Itraconazole vs. trimethoprim-sulfamethoxazole: A comparative cohort study of 200 patients with paracoccidioidomycosis. Med Mycol. 2014;52(3):303-10. https://doi.org/10.1093/mmy/myt012
Blotta MH, Mamoni RL, Oliveira SJ, Nouér SA, Papaiordanou PM, Goveia A, et al. Endemic regions of paracoccidioidomycosis in Brazil: a clinical and epidemiologic study of 584 cases in the southeast region. Am J Trop Med Hyg. 1999;61(3):390-4. https://doi.org/10.4269/ajtmh.1999.61.390
Brunaldi MO, Rezende RE, Zucoloto S, Garcia SB, Módena JL, Machado AA. Co-infection with paracoccidioidomycosis and human immunodeficiency virus: report of a case with esophageal involvement. Am J Trop Med Hyg. 2010;82(6):1099-101. https://doi.org/10.4269/ajtmh.2010.09-0751
Moreto TC, Marques ME, de Oliveira ML, Moris DV, de Carvalho LR, Mendes RP. Accuracy of routine diagnostic tests used in paracoccidioidomycosis patients at a university hospital. Trans R Soc Trop Med Hyg. 2011;105(8):473-8. https://doi.org/10.1016/j.trstmh.2011.03.001
Negroni R. Paracoccidiodes brasiliensis (Paracoccidiomycosis) [Internet]. Antimicrobe.org. 2021 [consultado el 12 de octubre de 2021]. Disponible en: http://www.antimicrobe.org/f09.asp
Shikanai-Yasuda MA, Conceição YM, Kono A, Rivitti E, Campos AF, Campos SV. Neoplasia and paracoccidioidomycosis. Mycopathologia. 2008;165(4-5):303-12. https://doi.org/10.1007/s11046-007-9047-2
Tobón AM, Agudelo CA, Osorio ML, Alvarez DL, Arango M, Cano LE, et al. Residual pulmonary abnormalities in adult patients with chronic paracoccidioidomycosis: prolonged follow-up after itraconazole therapy. Clin Infect Dis. 2003;37(7):898-904. https://doi.org/10.1086/377538
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














