Severe Manifestation of Peritoneal Tuberculosis: Clinical Case Report
DOI:
https://doi.org/10.22516/25007440.961Keywords:
Peritoneal tuberculosis, Ascites, Laparoscopy, Histology, DiagnosisAbstract
Aim: To describe the clinical manifestation and the diagnostic process of a patient with peritoneal tuberculosis as a clinical challenge in a tertiary referral center in a Latin American country.
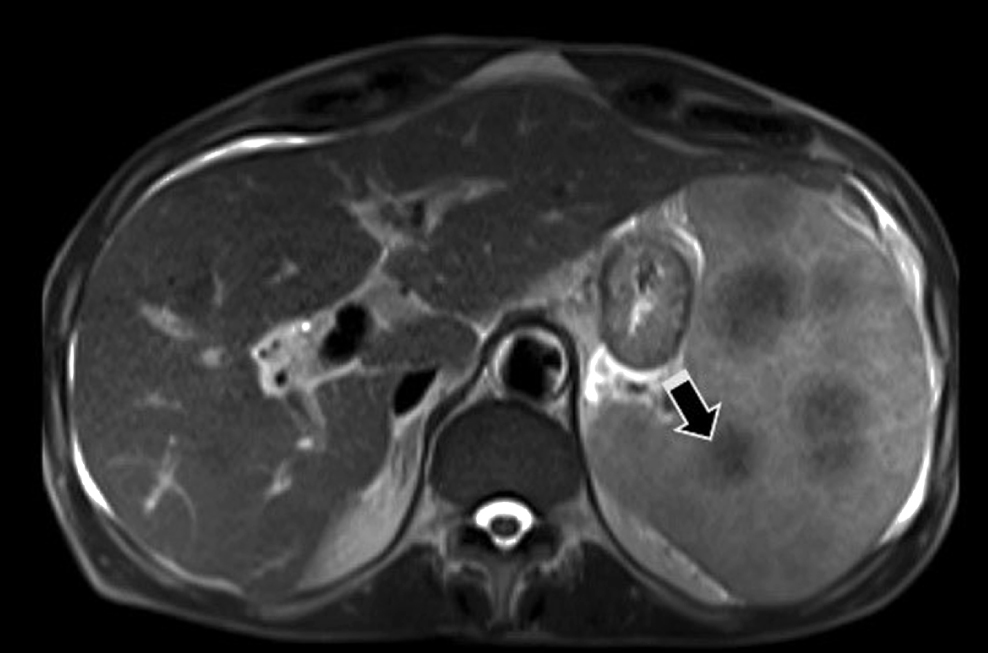
Case description: A 61-year-old male patient from the urban area of Cali consulted for edema in the lower limbs, ascites, hyporexia, weight loss, cachexia, thrombocytopenia, elevated transaminases, imaging of splenomegaly and pulmonary, hepatic, and peritoneum nodules. Initially, neoplasia was suspected, but the adenosine deaminase report and histopathology were consistent with the diagnosis of peritoneal tuberculosis.
Conclusion: Peritoneal tuberculosis represents the sixth cause of extrapulmonary tuberculosis, after lymphatic, pleural, osteoarticular, genitourinary, and meningeal manifestations. Despite having surveillance systems, peritoneal tuberculosis is still considered the most challenging infectious disease to reach a definitive diagnosis. We present a case of disseminated tuberculosis in which invasion of the peritoneum was verified, for which tetraconjugate treatment was started; however, the patient showed an adverse hepatic reaction and died due to multisystem involvement of a pulmonary infectious complication.
Downloads
References
Dineen P, Homan W, Grafe W. Tuberculous Peritonitis. Ann Surg. 1976;184(6):717-722. https://doi.org/10.1097/00000658-197612000-00010
Peto H, Pratt R, Harrington T, LoBue P, Armstrong L. Epidemiology of Extrapulmonary Tuberculosis in the United States, 1993-2006. Clinical Infectious Diseases. 2009;49(9):1350-7. https://doi.org/10.1086/605559
Uygur-Bayramiçli O. A clinical dilemma: abdominal tuberculosis. World J Gastroenterol. 2003;9(5):1098-101. https://doi.org/10.3748/wjg.v9.i5.1098
Guirat A, Koubaa M, Mzali R, Abid B, Ellouz S, Affes N, et al. Peritoneal tuberculosis. Clin Res Hepatol Gastroenterol. 2011;35(1):60-69. https://doi.org/10.1016/j.gcb.2010.07.023
Koff A, Azar M. Diagnosing peritoneal tuberculosis. BMJ Case Reports. 2020;13(2):e233131. https://doi.org/10.1136/bcr-2019-233131
Norbis L, Alagna R, Tortoli E, Codecasa L, Migliori G, Cirillo D. Challenges and perspectives in the diagnosis of extrapulmonary tuberculosis. Expert Rev Anti Infect Ther. 2014;12(5):633-47. https://doi.org/10.1586/14787210.2014.899900
Marshall J. Tuberculosis of the gastrointestinal tract and peritoneum. Pediatr Infect Dis J. 1994;13(4):341. https://doi.org/10.1097/00006454-199404000-00031
Manohar A, Simjee A, Haffejee A, Pettengell K. Symptoms and investigative findings in 145 patients with tuberculous peritonitis diagnosed by peritoneoscopy and biopsy over a five year period. Gut. 1990;31(10):1130-1132. https://doi.org/10.1136/gut.31.10.1130
Sanai F, Bzeizi K. Systematic review: tuberculous peritonitis - presenting features, diagnostic strategies and treatment. Aliment Pharmacol Ther. 2005;22(8):685-700. https://doi.org/10.1111/j.1365-2036.2005.02645.x
Norbis L, Alagna R, Tortoli E, Codecasa L, Migliori G, Cirillo D. Challenges and perspectives in the diagnosis of extrapulmonary tuberculosis. Expert Review of Anti-infective Therapy. 2014;12(5):633-47. https://doi.org/10.1586/14787210.2014.899900
Obaid Shakil A, Korula J, Kanel G, Murray N, Reynolds T. Diagnostic features of tuberculous peritonitis in the absence and presence of chronic liver disease: A case control study. Am J Med. 1996;100(2):179-85. https://doi.org/10.1016/S0002-9343(97)89456-9
Sharma S, Kohli M, Chaubey J, Yadav R, Sharma R, Singh B, et al. Evaluation of Xpert MTB/RIF assay performance in diagnosing extrapulmonary tuberculosis among adults in a tertiary care centre in India. Eur Respir J. 2014;44(4):1090-3. https://doi.org/10.1183/09031936.00059014
Shen Y, Wang T, Chen L, Yang T, Wan C, Hu Q, et al. Systematic review/Meta-analysis Diagnostic accuracy of adenosine deaminase for tuberculous peritonitis: a meta-analysis. Arch Med Sci. 2013;4(4):601-7. https://doi.org/10.5114/aoms.2013.36904
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |
















