Evaluating the Efficacy and Safety of Laparoscopic Heller Myotomy in Treating Achalasia
DOI:
https://doi.org/10.22516/25007440.970Keywords:
Esophageal achalasia, Swallowing disorders, Dysphagia, Esophageal aperistalsis, Heller myotomyAbstract
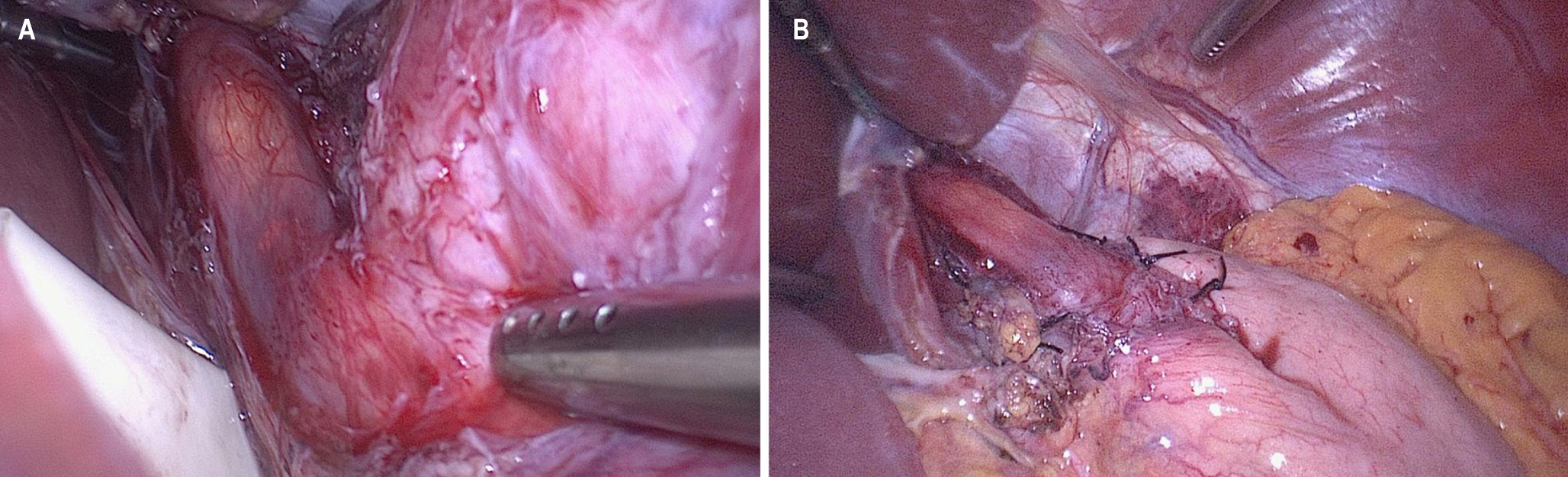
Introduction: Laparoscopic Heller myotomy (LHM) is widely recognized as the standard surgical treatment for esophageal achalasia. However, there is a lack of local data regarding the clinical characteristics of patients and the outcomes of this intervention.
Methodology: This retrospective study analyzed patients who underwent LHM over an eight-year period. Demographic, operative, and postoperative variables were assessed. The Eckardt score was used to compare symptoms before and after the intervention. Continuous variables were presented as means.
Results: Among the 39 patients assessed, 27 met the inclusion criteria. Of these, 51% were male, with an average age of 48 years. The average lower esophageal sphincter pressure was 36 mmHg. The mean operative time and bleeding were 133 minutes and 34 mL, respectively. The average length of the myotomy was 8.3 cm. Partial fundoplication was performed in all cases, and intraoperative endoscopy was conducted in 88% of the cases. Two intraoperative mucosal perforations occurred. The average length of hospital stay was 2.7 days. There was one medical complication but no mortality. Dysphagia significantly improved by 95%, and the mean Eckardt score decreased from 7.7 to 1.2 after surgery (p < 0.001). The average follow-up period was 24 months.
Conclusion: LHM with partial fundoplication proves to be an effective and safe procedure for treating achalasia. It results in the resolution of dysphagia in 95% of cases and carries minimal morbidity. Therefore, LHM should be considered the definitive treatment of choice for achalasia.
Downloads
References
Pandolfino JE, Gawron AJ. Achalasia. JAMA. 2015;313(18):1841. https://doi.org/10.1001/jama.2015.2996
Pandolfino JE, Kahrilas PJ. Presentation, Diagnosis, and Management of Achalasia. Clinical Gastroenterology and Hepatology. 2013;11(8):887-97. https://doi.org/10.1016/j.cgh.2013.01.032
Vaezi M, Krill J, Naik R. Clinical management of achalasia: current state of the art. Clin Exp Gastroenterol. 2016;9:71-82. https://doi.org/10.2147/CEG.S84019
Tuason J, Inoue H. Current status of achalasia management: a review on diagnosis and treatment. J Gastroenterol. 2017;52(4):401-6. https://doi.org/10.1007/s00535-017-1314-5
Rondón-Carvajal J, Ardila Hani C, Hani de Ardila AC, Vargas Rubio RD, Leguízamo Naranjo AM, Cañadas Garrido RA, et al. Megaesófago como complicación de acalasia: Reporte de caso y revisión narrativa de la literatura. Rev Colomb Gastroenterol. 2020;35(4):551-7. https://doi.org/10.22516/25007440.460
Spechler SJ, Talley N, Robson K. Achalasia: Pathogenesis, clinical manifestations, and diagnosis [Internet]. UpToDate; 2019 [consultado el 15 de enero de 2020]. Disponible en: https://www.uptodate.com/contents/achalasia-pathogenesis-clinical-manifestations-and-diagnosis
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: A New Clinically Relevant Classification by High-Resolution Manometry. Gastroenterology. 2008;135(5):1526-33. https://doi.org/10.1053/j.gastro.2008.07.022
Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, et al. Esophageal motility disorders on high‐resolution manometry: Chicago classification version 4.0? Neurogastroenterol Motil. 2021;33(1):e14053. https://doi.org/10.1111/nmo.14053
Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. Classifying Esophageal Motility by Pressure Topography Characteristics: A Study of 400 Patients and 75 Controls. Am J Gastroenterol. 2008;103(1):27-37. https://doi.org/10.1111/j.1572-0241.2007.01532.x
Schlottmann F, Herbella F, Allaix ME, Patti MG. Modern management of esophageal achalasia: From pathophysiology to treatment. Curr Probl Surg. 2018;55(1):10-37. https://doi.org/10.1067/j.cpsurg.2018.01.001
Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. American Journal of Gastroenterology. 2020;115(9):1393-411. https://doi.org/10.14309/ajg.0000000000000731
Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol. 2011;8(6):311-9. https://doi.org/10.1038/nrgastro.2011.68
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, et al. Pneumatic Dilation versus Laparoscopic Heller’s Myotomy for Idiopathic Achalasia. N Engl J Med. 2011;364(19):1807-16. https://doi.org/10.1056/NEJMoa1010502
Zaninotto G, Bennett C, Boeckxstaens G, Costantini M, Ferguson MK, Pandolfino JE, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus. 2018;31(9). https://doi.org/10.1093/dote/doy071
Wang L, Li YM, Li L. Meta-Analysis of Randomized and Controlled Treatment Trials for Achalasia. Dig Dis Sci. 2009;54(11):2303-11. https://doi.org/10.1007/s10620-008-0637-8
Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103(6):1732-8. https://doi.org/10.1016/0016-5085(92)91428-7
Taft TH, Carlson DA, Triggs J, Craft J, Starkey K, Yadlapati R, et al. Evaluating the reliability and construct validity of the Eckardt symptom score as a measure of achalasia severity. Neurogastroenterol Motil. 2018;30(6):e13287. https://doi.org/10.1111/nmo.13287
Prieto RG, Prieto JE, Casas F, Ballén H. Acalasia, una visión actual. Rev Colomb Cir. 2019;34(2):171-8. https://doi.org/10.30944/20117582.111
Borráez B, Patti M. Miotomía de Heller por vía laparoscópica: un procedimiento seguro. Rev Colomb Cir. 2014;29(3):182-7.
Vaezi MF, Richter JE. Diagnosis and Management of Achalasia. Am J Gastroenterol. 1999;94(12):3406-12. https://doi.org/10.1111/j.1572-0241.1999.01639.x
Fisichella PM, Raz D, Palazzo F, Niponmick I, Patti MG. Clinical, Radiological, and Manometric Profile in 145 Patients with Untreated Achalasia. World J Surg. 2008;32(9):1974-9. https://doi.org/10.1007/s00268-008-9656-z
Vaezi MF. The American College of Gastroenterology’s New Guidelines on Achalasia: What Clinicians Need to Know. Curr Gastroenterol Rep. 2013;15(12):358. https://doi.org/10.1007/s11894-013-0358-9
Vela MF, RJE. Management of achalasia at a tertiary center-a complicated disease. Gastroenterology. 2003;4(124):p.A236. https://doi.org/10.1016/S0016-5085(03)81186-1
Tsuboi K, Hoshino M, Srinivasan A, Yano F, Hinder RA, DeMeester TR, et al. Insights Gained from Symptom Evaluation of Esophageal Motility Disorders: A Review of 4,215 Patients. Digestion. 2012;85(3):236-42. https://doi.org/10.1159/000336072
Nau P, Rattner D. Laparoscopic Heller Myotomy as the Gold Standard for Treatment of Achalasia. J Gastrointest Surg. 2014;18(12):2201-7. https://doi.org/10.1007/s11605-014-2655-5
Ursut B, Alecu L, Tulin A, Enciu O. Laparoscopic treatment in achalasia of the cardia. Chirurgia (Bucur). 2014;109(5):604-7.
Agrusa A, Romano G, Bonventre S, Salamone G, Cocorullo G, Gulotta G. Laparoscopic treatment for esophageal achalasia: experience at a single center. G Chir. 2013;34(7-8):220-3. https://doi.org/10.11138/gchir/2013.34.7.220
Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F, et al. Endoscopic and Surgical Treatments for Achalasia. Ann Surg. 2009;249(1):45-57. https://doi.org/10.1097/SLA.0b013e31818e43ab
Illés A, Farkas N, Hegyi P, Garami A, Szabó I, Solymár M, et al. Is Heller Myotomy Better than Balloon Dilation? A Meta-Analysis. Journal of Gastrointestinal and Liver Diseases. 2017;26(2):121-7. https://doi.org/10.15403/jgld.2014.1121.262.myo
Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD. SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc. 2012;26(2):296-311. https://doi.org/10.1007/s00464-011-2017-2
Zonca P, Cambal M, Labas P, Hrbaty B, Jacobi CA. The role of laparoscopic Heller myotomy in the treatment of achalasia. Bratisl Lek Listy. 2014;115(3):156-60. https://doi.org/10.4149/BLL_2014_033
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, et al. Heller Myotomy Versus Heller Myotomy With Dor Fundoplication for Achalasia. Ann Surg. 2004;240(3):405-15. https://doi.org/10.1097/01.sla.0000136940.32255.51
Rawlings A, Soper NJ, Oelschlager B, Swanstrom L, Matthews BD, Pellegrini C, et al. Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc. 2012;26(1):18-26. https://doi.org/10.1007/s00464-011-1822-y
Wang L, Li YM, Li L, Yu CH. A systematic review and meta-analysis of the Chinese literature for the treatment of achalasia. World J Gastroenterol. 2008;14(38):5900. https://doi.org/10.3748/wjg.14.5900
Yaghoobi M, Mayrand S, Martel M, Roshan-Afshar I, Bijarchi R, Barkun A. Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc. 2013;78(3):468-75. https://doi.org/10.1016/j.gie.2013.03.1335
Moonen AJ, Boeckxstaens GE. Management of Achalasia. Gastroenterol Clin North Am. 2013;42(1):45-55. https://doi.org/10.1016/j.gtc.2012.11.009
Rodríguez-Fajardo JA, Mantilla-Gaviria HJ, Pineda-Ovalle LF, Jalal-Espitia AA, Escobar-Cruz HJ, Arbelaez-Méndez VH, et al. Miotomía endoscópica por vía oral (POEM) para el tratamiento de Acalasia: nuestras primeras experiencias. Rev Colomb Gastroenterol. 2018;33(3):228. https://doi.org/10.22516/25007440.197
Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, et al. Comparison of Perioperative Outcomes Between Peroral Esophageal Myotomy (POEM) and Laparoscopic Heller Myotomy. Journal of Gastrointestinal Surgery. 2013;17(2):228-35. https://doi.org/10.1007/s11605-012-2030-3
Krieger‐Grübel C, Tutuian R, Borovicka J. Correlation of esophageal clearance and dysphagia symptom assessment after treatment for achalasia. United European Gastroenterol J. 2016;4(1):55-61. https://doi.org/10.1177/2050640615584732
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |
















