Parenteral nutrition: the prison that allows survival in the face of intestinal failure
DOI:
https://doi.org/10.22516/25007440.981Keywords:
Intestinal absorption, intestinal failure, parenteral nutrition, home, qualitative researchAbstract
Objective: Intestinal failure refers to a reduction in intestinal function that necessitates intravenous supplementation of macronutrients, water, or electrolytes due to the intestine’s inability to absorb these substances adequately to maintain health and growth. This study aims to explore the experiences and challenges faced by patients enrolled in the intestinal rehabilitation program at Hospital Pablo Tobón Uribe in Medellín.
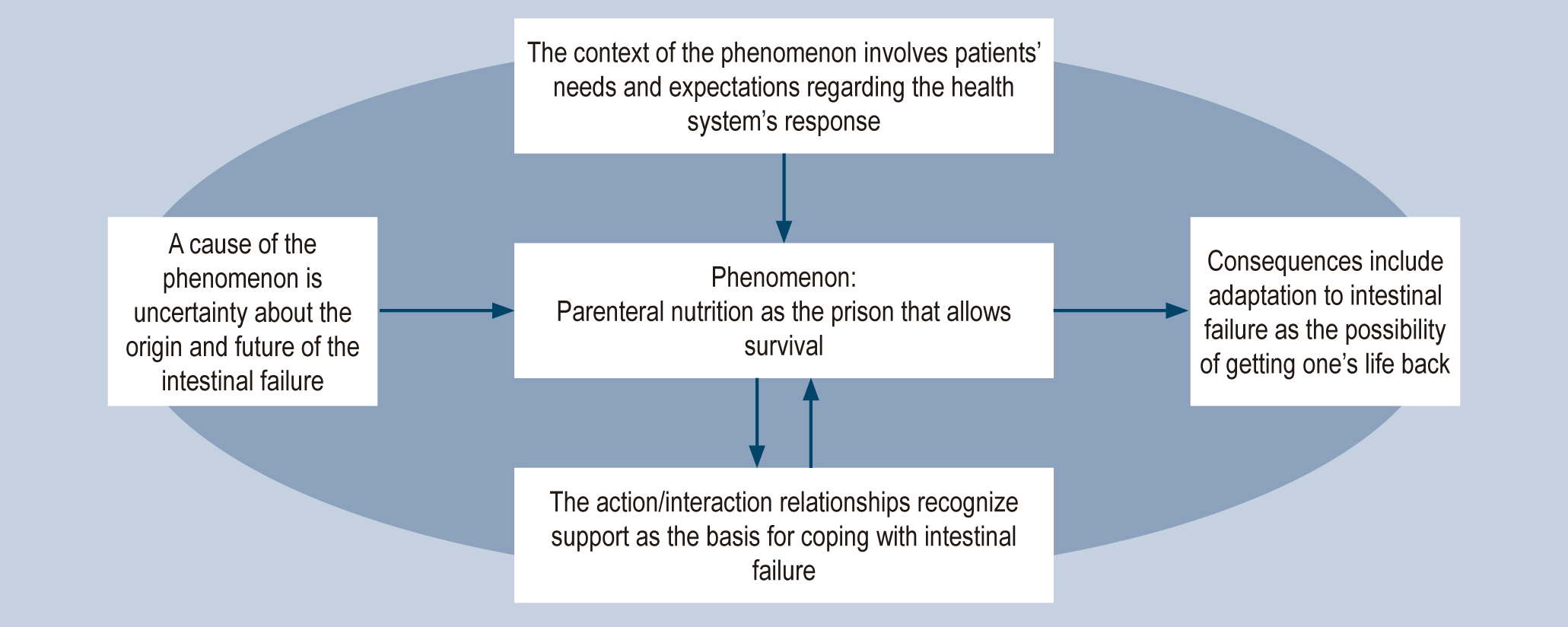
Methodology: This qualitative study adopts a hermeneutic approach and utilizes grounded theory techniques. The sampling process involved both selective and theoretical sampling. A total of 20 semi-structured interviews were conducted, with eight interviews including contributions from family members. The data analysis commenced with open coding, followed by the grouping of codes into descriptive categories. Dimensions and properties were identified within these categories, and analytical categories were subsequently developed through axial and selective coding. This iterative process led to the emergence of the final paradigm matrix.
Results: The study revealed that the healthcare system inadequately addresses the needs and expectations of patients with intestinal failure, leading to increased uncertainty about the disease’s origin and future prognosis. Intestinal failure and its treatment disrupt various aspects of patients’ lives, including personal, family, and work domains. Social stigmatization and rejection are prominent, underscoring the importance of support from family and close individuals in facilitating adaptation and revaluing life.
Conclusions: Coping with the challenges of intestinal failure entails embracing the necessity of relying on parenteral nutrition, which is perceived as a prison that paradoxically enables survival.
Downloads
References
Pironi L, Arends J, Baxter J, Bozzetti F, Peláez RB, Cuerda C, et al. Home Artificial Nutrition & Chronic Intestinal Failure; Acute Intestinal Failure Special Interest Groups of ESPEN. ESPEN endorsed recommendations. Definition and classification of intestinal failure in adults. Clin Nutr. 2015; 34(2):171-80. https://doi.org/10.1016/j.clnu.2014.08.017
Association of Surgeons of Great Britain and Ireland. Guidelines for Implementation of Enhanced Recovery Protocols [Internet]. Londres: Association of Surgeons of Great Britain and Ireland; 2009 [consultado 2022 Mar 31]. Disponible en: chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.asgbi.org.uk/userfiles/file/ipp/_iipp-eras-guidelines-as-gone-to-press.pdf
Solar H, Pedraza A, Gondolesi G. Insuficiencia intestinal Rehabilitacion médica y quirúrgica. En Galindo F. Enciclopedia de Cirugía Digestiva. Buenos Aires: Sociedad Argetina de Cirugía Digestiva; 2014. 1-13.
Carlsson E, Persson E. Living With Intestinal Failure Caused by Crohn Disease. Gastroenterol Nurs. 2015; 38(1):12-20. https://doi.org/10.1097/SGA.0000000000000085
Pubmed [base de datos en Internet]. Bethesda: National Library of Medicine; [consultado el 22 de junio del 2022]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/?term=intestinal%20failure
Alberti G, Le Roy C, Cofré C, Pattillo J, Domínguez P, Guerra J. Actualización en el manejo de pacientes con insuficiencia intestinal. Rev Chil pediatr. 2014 [citado 2022 Jun 22]; 85(2):148-156. https://doi.org/10.4067/S0370-41062014000200003
Carlson GL, Maguire G, Williams N, Bradley a, Shaffer JL, Irving MH. Quality of life on home parenteral nutrition: a single centre study of 37 patients. Clin Nutr. 1995; 14(4):219-28. https://doi.org/10.1016/S0261-5614(95)80003-4
Strauss AL, Corbin J. Basics of Qualitative Research Grounded Theory Procedures and Techniques. 1st ed. Sage Publications; 1990.
Charmaz K. Constructing grounded theory. A practical guide through qualitative analysis. Thousand Oaks: SAGE publications; 2006.
Glaser BG. Emergence vs Forcing: Basics of Grounded Theory: Strategies for Qualitative Research. First. Mill Valley: Sociology Press; 1992.
Yeasmin S, Rahman KF. "'Triangulation' Research Method as the Tool of Social Science Research." Bup Journal. 2012; 1(1): p.154-163
Resolución 8430 de 1993. Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Resolución numero 8430 (4 de octubre de 1993).
Wong C, Lucas B, Wood D. Patients' experiences with home parenteral nutrition: A grounded theory study. Clin Nutr ESPEN. 2018; 24:100-108. https://doi.org/10.1016/j.clnesp.2018.01.005
Heaney A, McKenna SP, Wilburn J, Rouse M, Taylor M, Burden S, et al. The impact of Home Parenteral Nutrition on the lives of adults with Type 3 Intestinal Failure. Clin Nutr ESPEN. 2018; 24:35-40. https://doi.org/10.1016/j.clnesp.2018.02.003
Sowerbutts AM, Panter C, Dickie G, Bennett B, Ablett J, Burden S, et al. Short bowel syndrome and the impact on patients and their families: a qualitative study. J Hum Nutr Diet. 2020; 33(6):767-774. https://doi.org/10.1111/jhn.12803
Blüthner E, Bednarsch J, Stockmann M, Karber M, Pevny S, Maasberg S, et al. Determinants of Quality of Life in Patients With Intestinal Failure Receiving Long-Term Parenteral Nutrition Using the SF-36 Questionnaire: A German Single-Center Prospective Observational Study. JPEN J Parenter Enteral Nutr. 2020; 44(2):291-300. https://doi.org/10.1002/jpen.1531
Avitzur Y, Miserachs M. Quality of life on long-term parenteral nutrition: can it be an indication for intestinal transplantation? Curr Opin Organ Transplant. 2018; 23(2):199-206. https://doi.org/10.1097/MOT.0000000000000503
Ambrose T, Holdaway L, Smith A, Howe H, Vokes L, Vrakas G, et al. The impact of intestinal transplantation on quality of life. Clin Nutr. 2020; 39(6):1958-1967. https://doi.org/10.1016/j.clnu.2019.08.023
Smith CE, Yadrich D, Wright S, Ridder L, Werkowitch M, Bruce A, et al. Themes of Stressors, Emotional Fatigue, and Communication Challenges Found in Mobile Care Discussion Sessions With Patients Requiring Lifelong Home Parenteral Nutrition Infusions. JPEN J Parenter Enteral Nutr. 2021; 45(3):499-506. https://doi.org/10.1002/jpen.1854
Ablett J, Vasant DH, Taylor M, Cawley C, Lal S. Poor Social Support and Unemployment Are Associated With Negative Affect in Home Parenteral Nutrition-Dependent Patients With Chronic Intestinal Failure. JPEN J Parenter Enteral Nutr. 2019; 43(4):534-539. https://doi.org/10.1002/jpen.1457
Kumpf VJ. Challenges and Obstacles of Long-Term Home Parenteral Nutrition. Nutr Clin Pract. 2019; 34(2):196-203. https://doi.org/10.1002/ncp.10258
Burden ST, Jones DJ, Gittins M, Ablett J, Taylor M, Mountford C, et al. Needs-based quality of life in adults dependent on home parenteral nutrition. Clin Nutr. 2019; 38(3):1433-1438. https://doi.org/10.1016/j.clnu.2018.06.964
Cloutier A, Deutsch L, Miller B, Leahy G, Ablett J, Healey A, et al. Factors affecting antidepressant use by patients requiring home parenteral nutrition. JPEN J Parenter Enteral Nutr. 2022; 46(1):153-159. https://doi.org/10.1002/jpen.2090
French C, Lal S, Jones D, Sowerbutts AM, Brundrett D, Burch N, et al. Impact of home parenteral nutrition on family members: A national multi-centre cross-sectional study. Clin Nutr. 2022; 41(2):500-507. https://doi.org/10.1016/j.clnu.2021.12.030
Samuel M, Adaba F, Askari A, Maeda Y, Duffus J, Small M, et al. Home parenteral nutrition and employment in patients with intestinal failure: Factors associated with return to employment. Clin Nutr. 2019; 38(3):1211-1214. https://doi.org/10.1016/j.clnu.2018.04.021
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |
















