Frequency of Helicobacter pylori Infection in Patients Requiring GI Endoscopy in Seven Units in Three Antioquia Subregions
DOI:
https://doi.org/10.22516/25007440.983Keywords:
Helicobacter pylori, Epidemiology, Gastroduodenal diseases, Diagnostic testsAbstract
Aim: To determine the frequency of Helicobacter pylori and sociodemographic factors, life habits, and personal and family history of gastroduodenal diseases in patients who required and were taken to GI endoscopy (symptomatic or by screening) in seven endoscopy units in three Antioquia subregions.
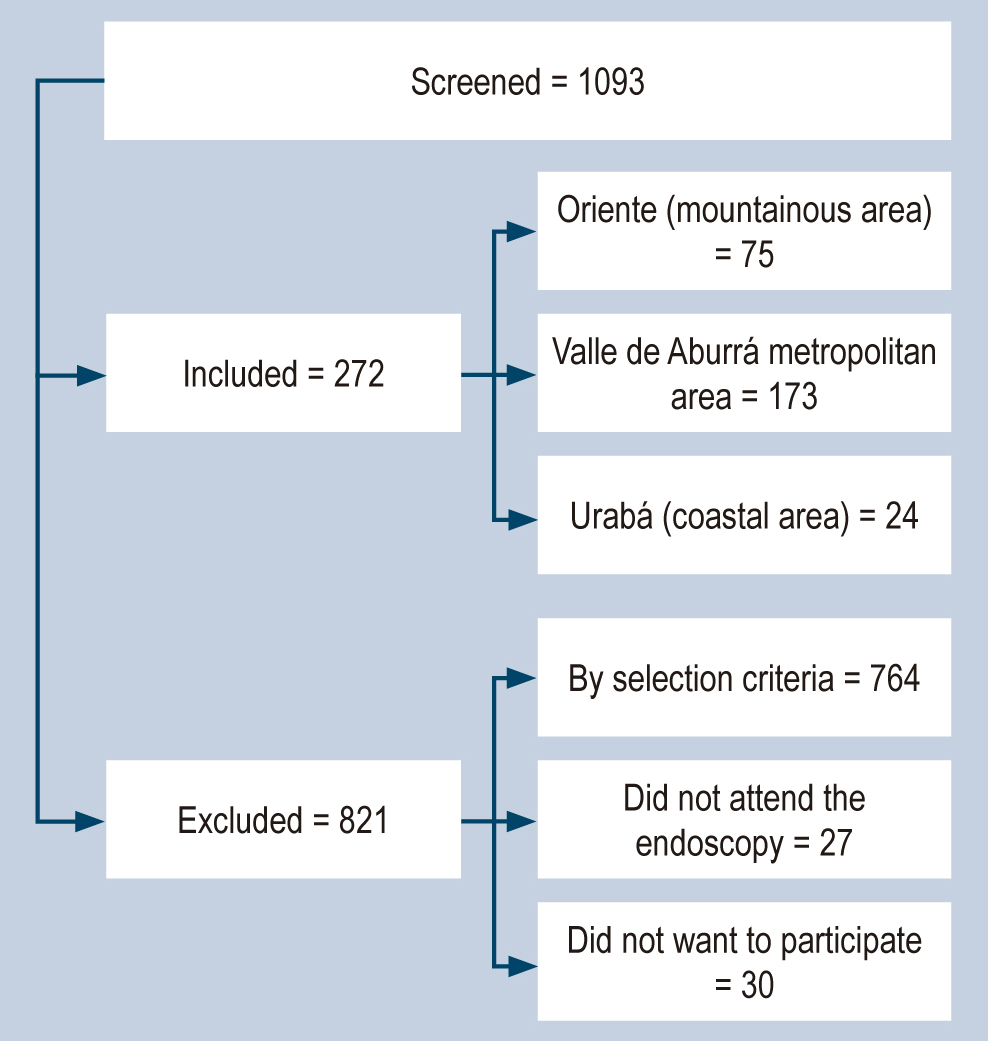
Materials and methods: A cross-sectional study conducted between 2016 and 2018 included 272 participants. Sociodemographic factors, life habits, and personal and family history were related to H. pylori infection. Descriptive statistics and bivariate analysis were performed to establish the association between the variables, and multivariate analysis (binomial regression) was used to adjust the prevalence ratios of the associated factors. A p-value ≤ 0.05 was considered statistically significant.
Results: The frequency of H. pylori infection was 55.9%, with differences by subregion (Valle de Aburrá metropolitan area: 54.3%, Oriente: 64%, and Urabá: 79.2%). Factors associated with H. pylori infection were male sex (adjusted prevalence ratio [APR] = 1.26; 95% confidence interval [CI] = 1.04-1.52), age 18-55 years (APR = 1.62; CI 95% = 1.22-2.16), absence of drinking water (APR = 1.40; 95% CI: 1.15-1.72) and educational level below university (APR = 1.73; 95% CI% = 1.26-2.38).
Conclusion: The frequency of H. pylori was higher than in other recent studies because different diagnostic tests were used for its detection, and differences were found in the frequency of infection by region, which is explained by the heterogeneity in the populations analyzed. This study suggests the need to improve the population’s living conditions to reduce H. pylori and direct measures of primary prevention of the infection, especially in family groups, men, individuals between 18 and 55 years old without drinking water, and with an educational level lower than university.
Downloads
References
Kotilea K, Bontems P, Touati E. Epidemiology, Diagnosis and Risk Factors of Helicobacter pylori Infection. Adv Exp Med Biol. 2019;1149:17-33. https://doi.org/10.1007/5584_2019_357
Crowe SE. Helicobacter pylori Infection. N Engl J Med. 2019;380(12):1158-65. https://doi.org/10.1056/NEJMcp1710945
Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology. 2017;153(2):420-9. https://doi.org/10.1053/j.gastro.2017.04.022
Kodaman N, Pazos A, Schneider BG, Piazuelo MB, Mera R, Sobota RS, et al. Human and Helicobacter pylori coevolution shapes the risk of gastric disease. Proc Natl Acad Sci U S A. 2014;111(4):1455-60. https://doi.org/10.1073/pnas.1318093111
Schistosomes, liver flukes and Helicobacter pylori. IARC Monogr Eval Carcinog Risks Hum. 1994;61:1-241.
Abnet C, Asaka M, Choi IJ, Correa P, Ferreccio C, Gisbert J, et al. Helicobacter pylori eradication as a strategy for preventing gastric cancer [Internet]. IARC Working Group Reports; 2014;8 [consultado el 1 de octubre del 2022]. Disponible en: https://rb.gy/9v6qk
International Agency for Research on Cancer. WHO; 2021 [consultado el 12 de septiembre del 2022]. Disponible en: https://gco.iarc.fr/today/data/factsheets/populations/170-colombia-fact-sheets.pdf
Pardo C, De Vries E, Buitrago L, Gamboa Ó. Atlas de mortalidad por cáncer en Colombia [Internet]. 4.a edición. Instituto Nacional de Cancerología; 2017 [consultado el 26 de junio del 2022]. Disponible en: https://rb.gy/x91r5
Departamento Administrativo Nacional de Estadística. Mortalidad por cáncer de estómago según subregión y municipio. DANE; 2021. Disponible en: https://dssa.gov.co/index.php/estadisticas-mortalidad/item/80-mortalidad-por-cancer-por-subregion-municipio-2005-2020
Chaturvedi R, De Sablet T, Asim M, Piazuelo MB, Barry DP, Verriere TG, et al. Increased Helicobacter pylori-associated gastric cancer risk in the Andean region of Colombia is mediated by spermine oxidase. Oncogene. 2015;34(26):3429-40. https://doi.org/10.1038/onc.2014.273
Mera R, Bravo L, Camargo MC, Bravo J, Delgado A, Romero-Gallo J, et al. Dynamics of Helicobacter pylori infection as a determinant of progression of gastric precancerous lesions: 16-year follow- up of an eradication trial. Physiol Behav. 2017;176(5):139-48. https://doi.org/10.1136/gutjnl-2016-311685
Zamani M, Ebrahimtabar F, Zamani V, Miller WH, Alizadeh-Navaei R, Shokri-Shirvani J, et al. Systematic review with meta-analysis: the worldwide prevalence of Helicobacter pylori infection. Aliment Pharmacol Ther. 2018;47(7):868-76. https://doi.org/10.1111/apt.14561
Ford AC, Yuan Y, Forman D, Hunt R, Moayyedi P. Helicobacter pylori eradication for the prevention of gastric neoplasia. Cochrane Database Syst Rev. 2020;84(6):525. https://doi.org/10.1002/14651858.CD005583.pub3
Piazuelo MB, Bravo LE, Mera RM, Camargo MC, Bravo JC, Delgado AG, et al. The Colombian Chemoprevention Trial: 20-Year Follow-Up of a Cohort of Patients With Gastric Precancerous Lesions. Gastroenterology. 2021;160(4):1106-1117.e3. https://doi.org/10.1053/j.gastro.2020.11.017
Liou J-M, Malfertheiner P, Lee Y-C, Sheu B-S, Sugano K, Cheng H-C, et al. Screening and eradication of Helicobacter pylori for gastric cancer prevention: the Taipei global consensus. Gut. 2020;69(12):2093-112. https://doi.org/10.1136/gutjnl-2020-322368
Chiang TH, Chang WJ, Chen SLS, Yen AMF, Fann JCY, Chiu SYH, et al. Mass eradication of Helicobacter pylori to reduce gastric cancer incidence and mortality: A long-term cohort study on Matsu Islands. Gut. 2021;70(2):243-50. https://doi.org/10.1136/gutjnl-2020-322200
Pardo C, de Vries E. Supervivencia global de pacientes con cáncer en el Instituto Nacional de Cancerología (INC). Rev Colomb Cancerol. 2017;21(1):12-8. https://doi.org/10.1016/j.rccan.2017.01.003
Arias-Ortiz NE, de Vries E. Health inequities and cancer survival in Manizales, Colombia: a population-based study. Colomb Medica. 2018;49(1):63-72. https://doi.org/10.25100/cm.v49i1.3629
Salazar BE, Pérez-Cala T, Gomez-Villegas SI, Cardona-Zapata L, Pazos-Bastidas S, Cardona-Estepa A, et al. The OLGA-OLGIM staging and the interobserver agreement for gastritis and preneoplastic lesion screening: a cross-sectional study. Virchows Arch. 2022;(0123456789). https://doi.org/10.1007/s00428-022-03286-8
Atherton JC, Cao P, Peek RM, Tummuru MKR, Blaser MJ, Cover TL. Mosaicism in vacuolating cytotoxin alleles of helicobacter pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem. 1995;270(30):17771-7. https://doi.org/10.1074/jbc.270.30.17771
Van Doorn LJ, Figueiredo C, Sanna R, Pena S, Midolo P, Ng EKW, et al. Expanding allelic diversity of Helicobacter pylori vacA. J Clin Microbiol. 1998;36(9):2597-603. https://doi.org/10.1128/JCM.36.9.2597-2603.1998
Peek RM, Miller GG, Tham KT, Perez-Perez GI, Cover TL, Atherton JC, et al. Detection of Helicobacter pylori gene expression in human gastric mucosa. J Clin Microbiol. 1995;33(1):28-32. https://doi.org/10.1128/jcm.33.1.28-32.1995
Organización Mundial de la Salud (OMS). Tabaquismo [Internet]. Who.int. [consultado el 13 de octubre del 2022]. Disponible en: https://www.who.int/es/health-topics/tobacco
Correa GS, Cardona AAF, Correa GT, Correa LLA, García GHI, Estrada MS. Prevalencia de Helicobacter pylori y características histopatológicas en biopsias gástricas de pacientes con síntomas dispépticos en un centro de referencia de Medellín. Rev Colomb Gastroenterol. 2016;31(1):9-15. https://doi.org/10.22516/25007440.67
Roldán IJ, Castaño R, Navas MC. Mutaciones del gen ARN ribosómico 23S de Helicobacter pylori asociadas con resistencia a claritromicina en pacientes atendidos en una unidad de endoscopia de Medellín, Colombia. Biomedica. 2019;39(2):117-29. https://doi.org/10.7705/biomedica.v39i4.4377
Sánchez Londoño S, Guevara Casallas G, Niño S, Arteta Cueto A, Marcelo Escobar R, Camilo Ricaurte J, et al. Patrones de detección de Helicobacter pylori y lesiones relacionadas mediante protocolo Sydney en una población de Antioquia, Colombia. Rev Gastroenterol del Perú. 2022;42(2):86-91. https://doi.org/10.47892/rgp.2022.422.1377
Cámara de Comercio de Medellín. Perfiles socioeconómicos de las subregiones de Antioquia 2021. Cámara de Comercio de Medellín. Medellín; 2021. [consultado el 10 de octubre del 2022]. Disponible en: https://rb.gy/frwwg
Gobernación de Antioquia. Anuario estadístico de Antioquia. Perfiles socioeconómicos de las subregiones de Antioquia 2021. Cámara de Comercio de Medellín. Medellín; 2019 [consultado el 25 de febrero de 2022]. Disponible en: https://www.antioquiadatos.gov.co/index.php/geoportal/indicadores/
Gobernación de Antioquia. Necesidades básicas insatisfechas [Internet]. Observatorio Metropolitano; 2017 [consultado el 25 de febrero de 2022]. Disponible en: https://antioquia.gov.co/necesidades-basicas-insatisfechas-nbi-vf
Gobernación de Antioquia. Anuario Estadístico de Antioquia 2018 – Portal [Internet]. AntioquiaDatos.gov.co; 2018 [consultado el 30 de enero de 2022]. Disponible en: https://www.antioquiadatos.gov.co/index.php/biblioteca-estadistica/anuario-estadistico-de-antioquia/anuario-estadistico-de-antioquia-2018/
Kayali S, Manfredi M, Gaiani F, Bianchi L, Bizzarri B, Leandro G, et al. Helicobacter pylori, transmission routes and recurrence of infection: state of the art. Acta Biomed. 2018;89(8-S):72-6. https://doi.org/10.23750/abm.v89i8-S.7947
Vesga F-J, Moreno Y, Ferrús MA, Campos C, Trespalacios AA. Detection of Helicobacter pylori in drinking water treatment plants in Bogotá, Colombia, using cultural and molecular techniques. Int J Hyg Environ Health. 2018;221(4):595-601. https://doi.org/10.1016/j.ijheh.2018.04.010
Oliveros R, Pinilla Morales RE, Facundo Navia H, Sánchez Pedraza R. Cáncer gástrico: una enfermedad prevenible. Estrategias para intervención en la historia natural. Rev Colomb Gastroenterol. 2019;34(2):177-89. https://doi.org/10.22516/25007440.394
Wang W, Jiang W, Zhu S, Sun X, Li P, Liu K, et al. Assessment of prevalence and risk factors of helicobacter pylori infection in an oilfield Community in Hebei, China. BMC Gastroenterol. 2019;19(1):186. https://doi.org/10.1186/s12876-019-1108-8
Razuka-Ebela D, Polaka I, Parshutin S, Santare D, Ebela I, Murillo R, et al. Sociodemographic, Lifestyle and Medical Factors Associated with Helicobacter Pylori Infection. J Gastrointest Liver Dis. 2020;29(3):319-27. https://doi.org/10.15403/jgld-870
Nagy P, Johansson S, Molloy-Bland M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog. 2016;8(1). https://doi.org/10.1186/s13099-016-0091-7
Ferrari F, Cantú E, Dutra G, Zanardi HC, Scolaro BL, Ferrari OM. ORIGINAL Time trends of Helicobacter pylori prevalence in Itajaí - SC : a retrospective study of 25 years based on endoscopic database. Arq Gastroenterol. 2019;56(1):10-14. https://doi.org/10.1590/s0004-2803.201900000-13
Yu X, Yang X, Yang T, Dong Q, Wang L, Feng L. Decreasing prevalence of Helicobacter pylori according to birth cohorts in urban China. Turkish J Gastroenterol. 2017;28(2):94-7. https://doi.org/10.5152/tjg.2017.16557
Konno M, Yokota S, Suga T, Takahashi M, Sato K, Fujii N. Predominance of mother-to-child transmission of Helicobacter pylori infection detected by random amplified polymorphic DNA fingerprinting analysis in Japanese families. Pediatr Infect Dis J. 2008;27(11):999-1003. https://doi.org/10.1097/INF.0b013e31817d756e
Yücel O, Sayan A, Yildiz M. The factors associated with asymptomatic carriage of Helicobacter pylori in children and their mothers living in three socio-economic settings. Jpn J Infect Dis. 2009;62(2):120-4. https://doi.org/10.7883/yoken.JJID.2009.120
Kivi M, Johansson ALV, Reilly M, Tindberg Y. Helicobacter pylori status in family members as risk factors for infection in children. Epidemiol Infect. 2005;133(4):645-52. https://doi.org/10.1017/S0950268805003900
Yilmaz E, Doğan Y, Gürgöze MK, Unal S. Seroprevalence of Helicobacter pylori infection among children and their parents in eastern Turkey. J Paediatr Child Health. 2002;38(2):183-6. https://doi.org/10.1046/j.1440-1754.2002.00735.x
Weyermann M, Rothenbacher D, Brenner H. Acquisition of helicobacter pylori infection in early childhood: Independent contributions of infected mothers, fathers, and siblings. Am J Gastroenterol. 2009;104(1):182-9. https://doi.org/10.1038/ajg.2008.61
Urita Y, Watanabe T, Kawagoe N, Takemoto I, Tanaka H, Kijima S, et al. Role of infected grandmothers in transmission of Helicobacter pylori to children in a Japanese rural town. J Paediatr Child Health. 2013;49(5):394-8. https://doi.org/10.1111/jpc.12191
Ertem D. Clinical Practice: Helicobacter pylori infection in childhood. Eur J Pediatr. 2013;172(11):1427-34. https://doi.org/10.1007/s00431-012-1823-4
Yucel O. Prevention of Helicobacter pylori infection in childhood. World J Gastroenterol. 2014;20(30):10348-54. https://doi.org/10.3748/wjg.v20.i30.10348
Hu J, Wang X, Chua EG, He Y, Shu Q, Zeng L, et al. Prevalence and risk factors of Helicobacter pylori infection among children in Kuichong Subdistrict of Shenzhen City, China. PeerJ. 2020;8:e8878. https://doi.org/10.7717/peerj.8878
Bogiel T, Mikucka A, Szaflarska-Popławska A, Grzanka D. Usefulness of Molecular Methods for Helicobacter pylori Detection in Pediatric Patients and Their Correlation with Histopathological Sydney Classification. Int J Mol Sci. 2022;24(1):179. https://doi.org/10.3390/ijms24010179
Sabbagh P, Javanian M, Koppolu V, Vasigala VR, Ebrahimpour S. Helicobacter pylori infection in children: an overview of diagnostic methods. Eur J Clin Microbiol Infect Dis. 2019;38(6):1035-45. https://doi.org/10.1007/s10096-019-03502-5
Yang I, Woltemate S, Piazuelo MB, Bravo LE, Yepez MC, Romero-Gallo J, et al. Different gastric microbiota compositions in two human populations with high and low gastric cancer risk in Colombia. Sci Rep. 2016;6(1):18594. https://doi.org/10.1038/srep18594
Whary MT, Avenia JMR, Bravo LE, Lofgren JL, Lertpiriyapong K, Mera-Giler R, et al. Contrasting serum biomarker profiles in two Colombian populations with different risks for progression of premalignant gastric lesions during chronic Helicobacter pylori infection. Cancer Epidemiol. 2020;67:101726. https://doi.org/10.1016/j.canep.2020.101726
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

Funding data
-
Universidad de Antioquia
Grant numbers proyecto 2014-1062 -
Departamento Administrativo de Ciencia, Tecnología e Innovación (COLCIENCIAS)
Grant numbers Proyecto 111577757202 contrato 644-2018;Convocatoria Doctorados Nacionales 617-2013

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














