Recomendaciones sobre diagnóstico y tratamiento de la alergia a la proteína de la leche de vaca en población pediátrica colombiana. Posición de expertos
DOI:
https://doi.org/10.22516/25007440.405Palabras clave:
Alergia a la Proteína de la Leche de Vaca (APLV), atopía, lactancia materna, fórmulas para lactantes, fórmulas hidrolizadas, dermatitis atópica, lactantes.Resumen
Objetivo: generar recomendaciones sobre el diagnóstico y el tratamiento de la alergia a la proteína de la leche de vaca (APLV), que sirvan de referencia y consulta para los médicos pediatras y de cuidado primario.
Materiales y métodos: el presente documento de posición de expertos fue desarrollado por un grupo de médicos, especialistas en diferentes áreas terapéuticas y con experiencia en APLV. Se definieron los temas más relevantes y se realizó una revisión de la literatura científica disponible, a fin de elaborar una propuesta de recomendaciones que fue discutida por los autores.
Resultados: se elaboró un documento de posición que propone un enfoque práctico sobre la definición, el diagnóstico y el tratamiento de la APLV en el paciente pediátrico.
Conclusiones: el diagnóstico temprano y el manejo adecuado de la APLV pueden contribuir a una disminución de la carga de esta enfermedad y sus complicaciones.
Descargas
Referencias bibliográficas
Montijo-Barrios E, López-Ugalde MV, Ramírez-Mayans J, Anaya-Flórez MS, Arredondo-García JL, Azevedo-Tenorio I, et al. [Guía latinoamericana para el diagnóstico y tratamiento de alergia a las proteínas de la leche de vaca (GL-APLV)]. Rev Invest Clin. 2014;66 Suppl 2:S9-S72.
Koletzko S, Niggemann B, Arato A, Dias JA, Heuschkel R, Husby S, et al. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr. 2012;55(2):221-9. https://doi.org/10.1097/MPG.0b013e31825c9482
Schoemaker AA, Sprikkelman AB, Grimshaw KE, Roberts G, Grabenhenrich L, Rosenfeld L, et al. Incidence and natural history of challenge-proven cow’s milk allergy in European children--EuroPrevall birth cohort. Allergy. 2015;70(8):963-72. https://doi.org/10.1111/all.12630
Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. Nutr Res. 2011;31(1):61–75. https://doi.org/10.1016/j.nutres.2011.01.001
Rona RJ, Keil T, Summers C, Gislason D, Zuidmeer L, Sodergren E, et al. The prevalence of food allergy: a meta-analysis. J Allergy Clin Immunol. 2007;120(3):638-46. https://doi.org/10.1016/j.jaci.2007.05.026
Ávila MDL. Pérez J, Del Río BE, Rosas MA, Lerma L, Sienra JJL. Hipersensibilidad por prueba cutánea a alimentos en pacientes alérgicos en el Hospital Infantil de México Federico Gómez. Rev Alergia Mex 2002;49(3):74-79.
Martínez J, Méndez C, Talesnik E, Campos E, Viviani P, Sánchez D. Pruebas cutáneas de hipersensibilidad inmediata en una población pediátrica seleccionada. Rev Med Chile. 2005;133(2):195-201. https://doi.org/10.4067/S0034-98872005000200007
Marrugo J, Hernández L, Villalba V. Prevalence of self-reported food allerg in Cartagena (Colombia) population. Allergol Immunopathol (Madr). 2008;36(6):320-4. https://doi.org/10.1016/S0301-0546(08)75863-4
Acevedo N, Sánchez J, Zakzuk J, Bornacelly A, Quiróz C, Alvarez Á, et al. Particular characteristics of allergic symptoms in tropical environments: follow up to 24 months in the FRAAT birth cohort study. BMC Pulm Med. 2012;12:13. https://doi.org/10.1186/1471-2466-12-13
Solé D, Mallol J, Wandalsen GF, Aguirre V; Latin American ISAAC Phase 3 Study Group. Prevalence of symptoms of eczema in Latin America: results of the International Study of Asthma and Allergies in Childhood (ISAAC) Phase 3. J Investig Allergol Clin Immunol. 2010;20(4):311-23.
Arévalo M, Reyes MA, Victoria L, Villegas A, Badiel M, Herrera S. Asma y rinitis alérgica en pre-escolares en Cali. Colomb Med. 2003;34(1):4-8.
Dennis RJ, Caraballo L, García E, Rojas MX, Rondón MA, Pérez A, et al. Prevalence of asthma and other allergic conditions in Colombia 2009–2010: a cross-sectional study. BMC Pulm Med. 2012;12(17);1-9. https://doi.org/10.1186/1471-2466-12-17
Orsi M, Fernández A, Follett FR, Marchisone S, Saieg G, Busoni VB, et al. Alergia a la proteína de la leche de vaca. Propuesta de Guía para el manejo de los niños con alergia a la proteína de la leche de vaca. Arch Argent Pediatr. 2009;107(5):459-470.
Fiocchi A, Brozek J, Schünemann H, Bahna SL, von Berg A, Beyer K, et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines. Pediatr Allergy Immunol. 2010;21 Suppl 21:1-125. https://doi.org/10.1111/j.1399-3038.2010.01068.x
Björkstén B. Genetic and environmental risk factors for the development of food allergy. Curr Opin Allergy Clin Immunol. 2005;5(3):249-53. https://doi.org/10.1097/01.all.0000168790.82206.17
Eggesbø M, Botten G, Stigum H, Samuelsen SO, Brunekreef B, Magnus P. Cesarean delivery and cow milk allergy/intolerance. Allergy. 2005;60(9):1172-3. https://doi.org/10.1111/j.1398-9995.2005.00857.x
Sánchez-Valverde F, Gil F, Martínez D, Fernández B, Aznal E, Oscoz M, et al. The impact of caesarean delivery and type of feeding on cow’s milk allergy in infants and subsequent development of allergic march in childhood. Allergy. 2009;64(6):884-9. https://doi.org/10.1111/j.1398-9995.2008.01931.x
Vera JF, Ramírez A. Síntomas digestivos y respuesta clínica en lactantes con alergia a la proteína de leche de vaca. Rev Chil Pediatr. 2013;84:(6):641-649. https://doi.org/10.4067/S0370-41062013000600007
Luyt D, Ball H, Makwana N, Green MR, Bravin K, Nasser SM, et al. BSACI guideline for the diagnosis and management of cow’s milk allergy. Clin Exp Allergy. 2014;44(5):642-72. https://doi.org/10.1111/cea.12302
Zuluaga LC, Ramírez R, Mejía LK, Vera JF. Outcomes of treating infants with cow’s milk protein allergies with an extensively hydrolyzed serum-based formula. Rev Colomb Gastroenterol. 2018;33(2):111-115. https://doi.org/10.22516/25007440.253
Ministerio de Salud de Chile. Guía clínica: alergia a proteína de lecha de vaca. Santiago: Ministerio de Salud; 2012.
Pumphrey RS, Gowland MH. Further fatal allergic reactions to food in the United Kingdom, 1999-2006. J Allergy Clin Immunol. 2007;119(4):1018-9. https://doi.org/10.1016/j.jaci.2007.01.021
Simons FE, Ardusso LR, Bilò MB, El-Magal YM, Ledford DK, Ring J, et al. World Allergy Organization anaphylaxis guidelines: summary. J Allergy Clin Immunol. 2011;127(3):587-593. https://doi.org/10.1016/j.jaci.2011.01.038
Skripak JM, Matsui EC, Mudd K, Wood RA. The natural history of IgE-mediated cow’s milk allergy. J Allergy Clin Immunol. 2007;120(5):1172-7. https://doi.org/10.1016/j.jaci.2007.08.023
Muraro A, Roberts G, Clark A, Eigenmann PA, Halken S, Lack G, et al. The management of anaphylaxis in childhood: position paper of the European academy of allergology and clinical immunology. Allergy. 2007;62(8):857-71. https://doi.org/10.1111/j.1398-9995.2007.01421.x
Sampson HA, Muñoz-Furlong A, Campbell RL, Adkinson NF, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report-Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117(2):391-7. https://doi.org/10.1016/j.jaci.2005.12.1303
Braganza SC, Acworth JP, Mckinnon DR, Peake JE, Brown AF. Paediatric emergency department anaphylaxis: different patterns from adults. Arch Dis Child. 2006;91(2):159–163. https://doi.org/10.1136/adc.2004.069914
Latcham F, Merino F, Lang A, Garvey J, Thomson MA, Walker-Smith JA, et al. A consistent pattern of minor immunodeficiency and subtle enteropathy in children with multiple food allergy. J Pediatr. 2003;143(1):39-47. https://doi.org/10.1016/S0022-3476(03)00193-8
Butt AM, Murch SH, Ng CL, Kitching P, Montgomery S, Philips A, et al. Upregulated eotaxin expression and T cell infiltration in the basal and papillary epithelium in cows’ milk associated reflux oesophagitis. Arch Dis Child. 2002;87(2):124–130. https://doi.org/10.1136/adc.87.2.124
Berni Canani R, Nocerino R, Terrin G, Coruzzo A, Cosenza L, Leone L, et al. Effect of Lactobacillus GG on tolerance acquisition in infants with cow’s milk allergy: a randomized trial. J Allergy Clin Immunol. 2012;129(2):580-2,582.e1-5. https://doi.org/10.1016/j.jaci.2011.10.004
Sicherer SH, Sampson HA. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018;141(1):41-58. https://doi.org/10.1016/j.jaci.2017.11.003
Kim HP, Vance RB, Shaheen NJ, Dellon ES. The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10(9):988-96.e5. https://doi.org/10.1016/j.cgh.2012.04.019
Pasha SF, DiBaise JK, Kim HJ, De Petris G, Crowell MD, Fleischer DE, et al. Patient characteristics, clinical, endoscopic, and histologic findings in adult eosinophilic esophagitis: a case series and systematic review of the medical literature. Dis Esophagus. 2007;20(4):311-9. https://doi.org/10.1111/j.1442-2050.2007.00721.x
Liacouras CA, Spergel JM, Ruchelli E, Verma R, Mascarenhas M, Semeao E, et al. Eosinophilic esophagitis: a 10-year experience in 381 children. Clin Gastroenterol Hepatol. 2005;3(12):1198-206. https://doi.org/10.1016/S1542-3565(05)00885-2
Lee KM, Lim HC, Kim JH, Yoon YH, Park HJ, Lee SI. Clinical implications of endoscopically suspected eosinophilic esophagitis. Korean J Gastroenterol. 2010;56(5):285-92. https://doi.org/10.4166/kjg.2010.56.5.285
Moawad FJ, Schoepfer AM, Safroneeva E, Ally MR, Chen YJ, Maydonovitch CL, et al. Eosinophilic oesophagitis and proton pump inhibitor-responsive oesophageal eosinophilia have similar clinical, endoscopic and histological findings. Aliment Pharmacol Ther. 2014;39(6):603-8. https://doi.org/10.1111/apt.12636
Uppal V, Kreiger P, Kutsch E. Eosinophilic Gastroenteritis and Colitis: a Comprehensive Review. Clin Rev Allergy Immunol. 2016;50(2):175-88. https://doi.org/10.1007/s12016-015-8489-4
Fleischer DM, Spergel JM, Assa’ad AH, Pongracic JA. Primary prevention of allergic disease through nutritional interventions. J Allergy Clin Immunol Pract. 2013;1(1):29-36. https://doi.org/10.1016/j.jaip.2012.09.003
Giovannini M, D’Auria E, Caffarelli C, Verduci E, Barberi S, Indinnimeo L, et al. Nutritional management and follow up of infants and children with food allergy: Italian Society of Pediatric Nutrition/Italian Society of Pediatric Allergy and Immunology Task Force Position Statement. Ital J Pediatr. 2014;40:1. https://doi.org/10.1186/1824-7288-40-1
Fiocchi A, Dahda L, Dupont C, Campoy C, Fierro V, Nieto A. Cow’s milk allergy: towards an update of DRACMA guidelines. World Allergy Organ J. 2016;9(1):35. https://doi.org/10.1186/s40413-016-0125-0
Fewtrell M, Bronsky J, Campoy C, Domellöf M, Embleton N, Fidler Mis N, et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2017;64(1):119-132. https://doi.org/10.1097/MPG.0000000000001454
Molnár K, Pintér P, Győrffy H, Cseh A, Müller KE, Arató A, et al. Characteristics of allergic colitis in breast-fed infants in the absence of cow’s milk allergy. World J Gastroenterol. 2013;19(24):3824-30. https://doi.org/10.3748/wjg.v19.i24.3824
Yu MC, Tsai CL, Yang YJ, Yang SS, Wang LH, Lee CT, et al. Allergic colitis in infants related to cow’s milk: clinical characteristics, pathologic changes, and immunologic findings. Pediatr Neonatol. 2013;54(1):49-55. https://doi.org/10.1016/j.pedneo.2012.11.006
Kokkonen J, Karttunen TJ. Lymphonodular hyperplasia on the mucosa of the lower gastrointestinal tract in children: an indication of enhanced immune response? J Pediatr Gastroenterol Nutr. 2002;34(1):42-6. https://doi.org/10.1097/00005176-200201000-00010
Hwang JB, Park MH, Kang YN, Kim SP, Suh SI, Kam S. Advanced criteria for clinicopathological diagnosis of food protein-induced proctocolitis. J Korean Med Sci. 2007;22(2):213–217. http://dx.doi.org/10.3346/jkms.2007.22.2.213
Mansueto P, Iacono G, Seidita A, D’Alcamo A, Sprini D, Carroccio A. Review article: intestinal lymphoid nodular hyperplasia in children-the relationship to food hypersensitivity. Aliment Pharmacol Ther. 2012;35(9):1000-9. https://doi.org/10.1111/j.1365-2036.2012.05062.x
European Academy of Allergy and Clinical Immunology (EAACI). Food Allergy and Anaphylaxis Guidelines. Zúrich: EAACI; 2014.
Jones SM, Burks AW. Food Allergy. N Engl J Med. 2017;377(12):1168-1176. https://doi.org/10.1056/NEJMcp1611971
Ebisawa M, Ito K, Fujisawa T; Committee for Japanese Pediatric Guideline for Food Allergy, The Japanese Society of Pediatric Allergy and Clinical Immunology, The Japanese Society of Allergology. Japanese guidelines for food allergy 2017. Allergol Int. 2017;66(2):248-264. https://doi.org/10.1016/j.alit.2017.02.001
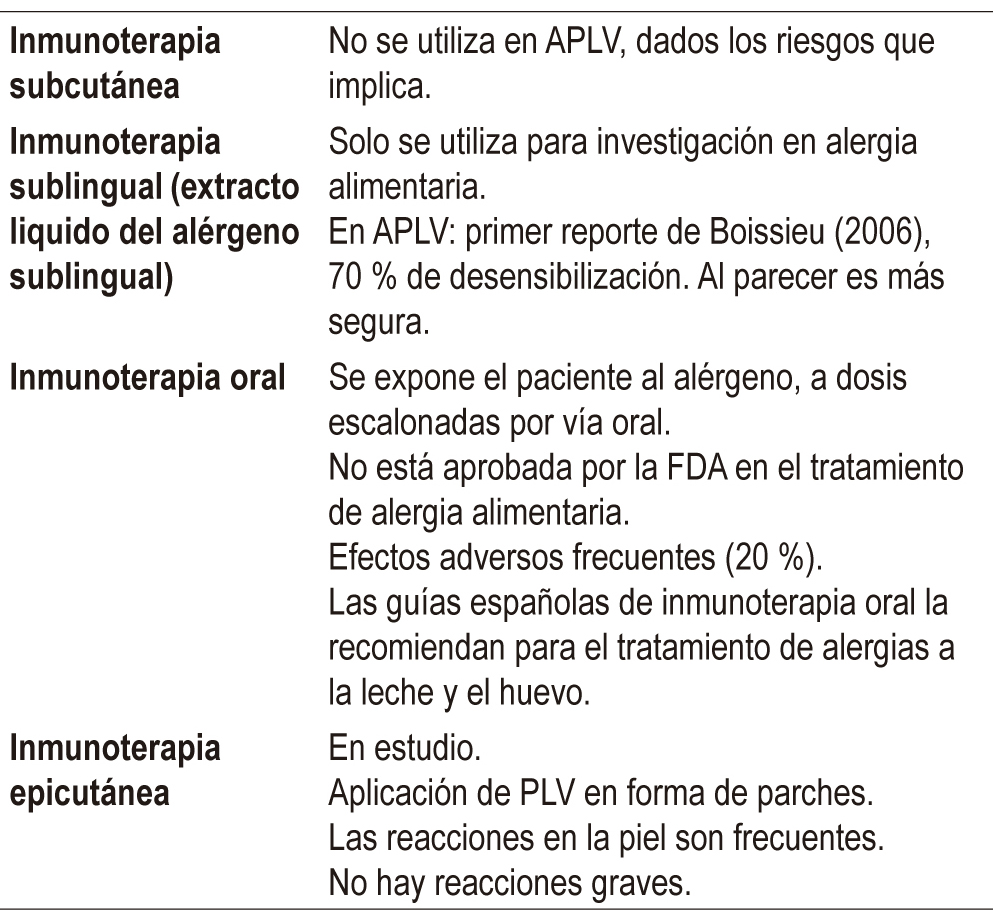
Martorell A, Alonso E, Echeverría L, Escudero C, García-Rodríguez R, Blasco C, et al. Oral Immunotherapy for Food Allergy: A Spanish Guideline. Immunotherapy Egg and Milk Spanish Guide (ITEMS Guide). Part I: Cow Milk and Egg Oral Immunotherapy: Introduction, Methodology, Rationale, Current State, Indications, Contraindications, and Oral Immunotherapy Build-up Phase. J Investig Allergol Clin Immunol. 2017;27(4):225-237. https://doi.org/10.18176/jiaci.0177
Kobernick AK, Burks AW. Active treatment for food allergy. Allergol Int. 2016;65(4):388-395. https://doi.org/10.1016/j.alit.2016.08.002
MacGinnite A. Update on Potential Therapies for IgE-Mediated Food Allergy. Curr Allergy Asthma Rep. 2017;17(1):4. https://doi.org/10.1007/s11882-017-0671-8
Hamad A, Burks WA. Emerging Approaches to Food Desensitization in Children. Curr Allergy Asthma Rep. 2017;17(5):32. https://doi.org/10.1007/s11882-017-0700-7
Vandenplas Y. Prevention and Management of Cow’s Milk Allergy in Non-Exclusively Breastfed Infants. Nutrients. 2017 Jul 10;9(7). pii: E731. https://doi.org/10.3390/nu9070731
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |
















