Evaluation of sustained responses to infiltration of local anesthetic in patients with chronic abdominal wall pain
DOI:
https://doi.org/10.22516/25007440.364Keywords:
Pain, infiltration, sustained response, Carnett’s signAbstract
Introduction: Chronic abdominal pain is frequently encountered at outpatient clinics where the traditional approach is to investigate visceral pathologies. Fifty percent of these patients are finally found to have abdominal wall pain which is generally secondary to entrapment of the anterior cutaneous nerve. This entity is identified by Carnett’s sign. The treatment of choice is to infiltrate the painful points with lidocaine following which there is significant improvement in 85% to 90% of these patients. The duration of post-infiltration improvement is unknown. The objective of this work is to determine sustained response in one and two-year follow-up examinations.
Materials and Methods: This is a retrospective cohort study conducted in the gastroenterology unit of the Clínica Fundadores. We included adult patients over 18 years of age who had received local injection treatment with 2% lidocaine without epinephrine and who had answered a telephone survey to assess the intensity of pain on an analogous scale.
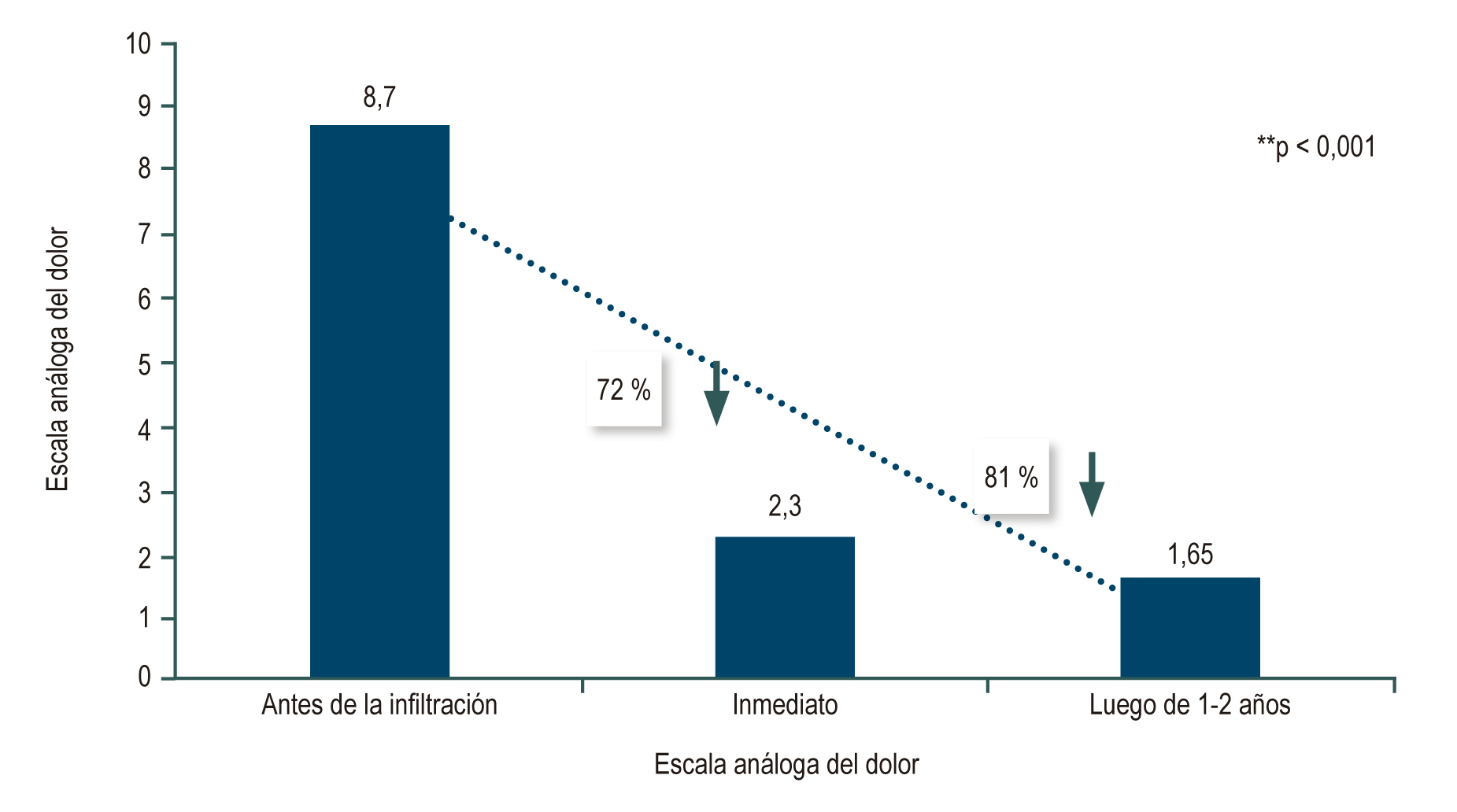
Results: Of the 360 eligible patients identified, 324 patients (90%) were interviewed by telephone. The average age of those interviewed was 57 years, and 87% were women. The average pain level prior to infiltration was 8.7 points. Following infiltration, the average intensity was 2.38 points (p <0.05). In 71% of patients, average pain intensity at a two year follow-up examination was 1.65 points (p <0.05), an 81% improvement in intensity (p = 0.001). Fibromyalgia had a positive association with sustained improvement in pain (p = 0.008).
Conclusions: Infiltration of the abdominal wall with a local anesthetic produces a sustained response for up to two years in patients with chronic abdominal wall pain.
Downloads
References
Otero W, Ruiz X, Otero E, Gómez M, Pineda LF. Dolor crónico de la pared abdominal: una entidad poco reconocida con gran impacto en la práctica médica. Rev Col Gastroenterol. 2007;22(4):261-71.
Rivero M, Moreira V, Riesco JM, Rodríguez MA, Garrido E, Milicua JM. Dolor originado en la pared abdominal: una alternativa diagnóstica olvidada. Gastroenterol Hepatol. 2007;30(4):244-50.
https://doi.org/10.1157/13100598
Paajanen H. Does laparoscopy used in open exploration alleviate pain associated with chronic intractable abdominal wall neuralgia? Surg Endosc. 2006;20(12):1835-8.
https://doi.org/10.1007/s00464-005-0744-y
Otero W, Martínez E, Lúquez A. El costo de ignorar el signo de Carnett, reporte de caso y revisión de literatura. Rev Col Gastroenterol. 2017;32(1):75-81.
Constanza CD, Longstreth GF, Liu AL. Chronic abdominal wall pain: clinical feature, health care costs and long term outcome. Clin Gastroenterol Hepatol. 2004;2(5):395-9. https://doi.org/10.1016/S1542-3565(04)00124-7
Sparkes V, Prevost T, Hunter JO. Derivation and identification of questions that act as predictors of abdominal pain of musculoskeletal origin. Eur J Gastroenterol Hepatol. 2003;15(9):1021-7.
https://doi.org/10.1097/00042737-200309000-00013
Keefer L, Drossman DA, Guthrie E, Simrén M, Tillisch K, Olden K, Whorwell PJ. Centrally Mediated Disorders of Gastrointestinal Pain. Gastroenterology. 2016;150(6):1408-19.
https://doi.org/10.1053/j.gastro.2016.02.034
Thomson C, Goodman R, Rowe WA. Abdominal wall syndrome: a costly diagnosis of exclusion. Gastroenterology. 2001;120(5):637A.
https://doi.org/10.1016/S0016-5085(08)83167-8
Carnett JB. Intercostal neuralgia as a cause of abdominal pain and tenderness. Surg Gynecol Obstet. 1926;42:625-32.
Carnett JB, Bates W. The treatment of intercostal neuralgia of the abdominal wall. 1933;98(5):820-9.
https://doi.org/10.1097/00000658-193311000-00002
Abdominal wall pain easily differentiated from visceral origin. Gastroenterology Observer. 1990;9(6):1-8.
Koop H, Koprdova S, Schürmann C. Chronic abdominal wall pain-a poorly recognized clinical problem. Dtsch Arztebl Int. 2016;113(4):51-7.
https://doi.org/10.3238/arztebl.2016.0051
Akhnikh S, de Korte N, de Winter P. Anterior cutaneous nerve entrapment syndrome: the forgotten diagnosis. Eur J Pediatr. 2014;173(4):445-9.
https://doi.org/10.1007/s00431-013-2140-2
Takada T, Ikusaka M, Ohira Y, Noda K, Tsukamoto T. Diagnostic usefulness of Carnett’s test in psychogenic abdominal pain. Intern Med. 2011;50(3):213-7.
https://doi.org/10.2169/internalmedicine.50.4179
Boelens OBA, Scheltinga MF, Houterman S, Roumen RM. Randomized clinical trials on trigger point infiltration with lidocaine to diagnose anterior cutaneous nerve entrapment syndrome. Br J Surg. 2013;100(2):217-21.
https://doi.org/10.1002/bjs.8958
Clarke S, Kanakarajan S. Abdominal cutaneous nerve entrapment syndrome. Contin Educ Anaesth Crit Care Pain. 2015;15(2):60-3.
https://doi.org/10.1093/bjaceaccp/mku016
Peleg R, Gohar J, Koretz M, Peleg A. Abdominal wall pain in pregnant women caused by thoracic lateral cutaneous nerve entrapment. Eur J Obstet Gynecol Reprod Biol. 1997;74(2):169-71.
https://doi.org/10.1016/S0301-2115(97)00114-0
Simons DG, Hong CZ, Simons LS. Endplate potentials are common to midfiber myofascial trigger points. Am J Phys Med Rehabil. 2002;81(3):212-22.
https://doi.org/10.1097/00002060-200203000-00010
van Assen T, Boelens OB, van Eerten PV, Perquin C, Scheltinga MR, Roumen RM. Long-term success rates after an anterior neurectomy in patients with an abdominal cutaneous nerve entrapment syndrome. Surgery. 2015:157(1):137-43.
https://doi.org/10.1016/j.surg.2014.05.022
Kuan LC, Li YT, Chen FM, Tseng CJ, Wu SF, Kuo TC. Efficacy of treating abdominal wall pain by local injection. Taiwanese J Obstet Gynecol. 2006;45(3):239-43.
https://doi.org/10.1016/S1028-4559(09)60232-1
Boelens OB, Scheltinga MR, Houterman S, Roumen RM. Management of anterior cutaneous nerve entrapment syndrome in a cohort of 139 patients. Ann Surg. 2011;254(6):1054‐1058.
https://doi.org/10.1097/SLA.0b013e31822d78b8
Nazareno J, Ponich T, Gregor J. Long-term follow-up of trigger point injections for abdominal wall pain. Can J Gastroenterol. 2005;19(9):561-5.
https://doi.org/10.1155/2005/274181
Kamboj AK, Hoversten P, Oxentenko AS. Chronic abdominal wall pain: a common yet overlooked etiology of chronic abdominal pain. Mayo Clin Proc. 2019;94(1):139-44.
https://doi.org/10.1016/j.mayocp.2018.09.018
Álvarez D, Rockwell PAG. Trigger points: diagnosis and management. Am Acad Fam Phys. 2002; 65: 653-60.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














