Update of high-resolution anorectal manometry interpretation using the London classification
DOI:
https://doi.org/10.22516/25007440.484Keywords:
Anorectal manometry, funtional anorectal disorders, anorectal physiology, London classificationAbstract
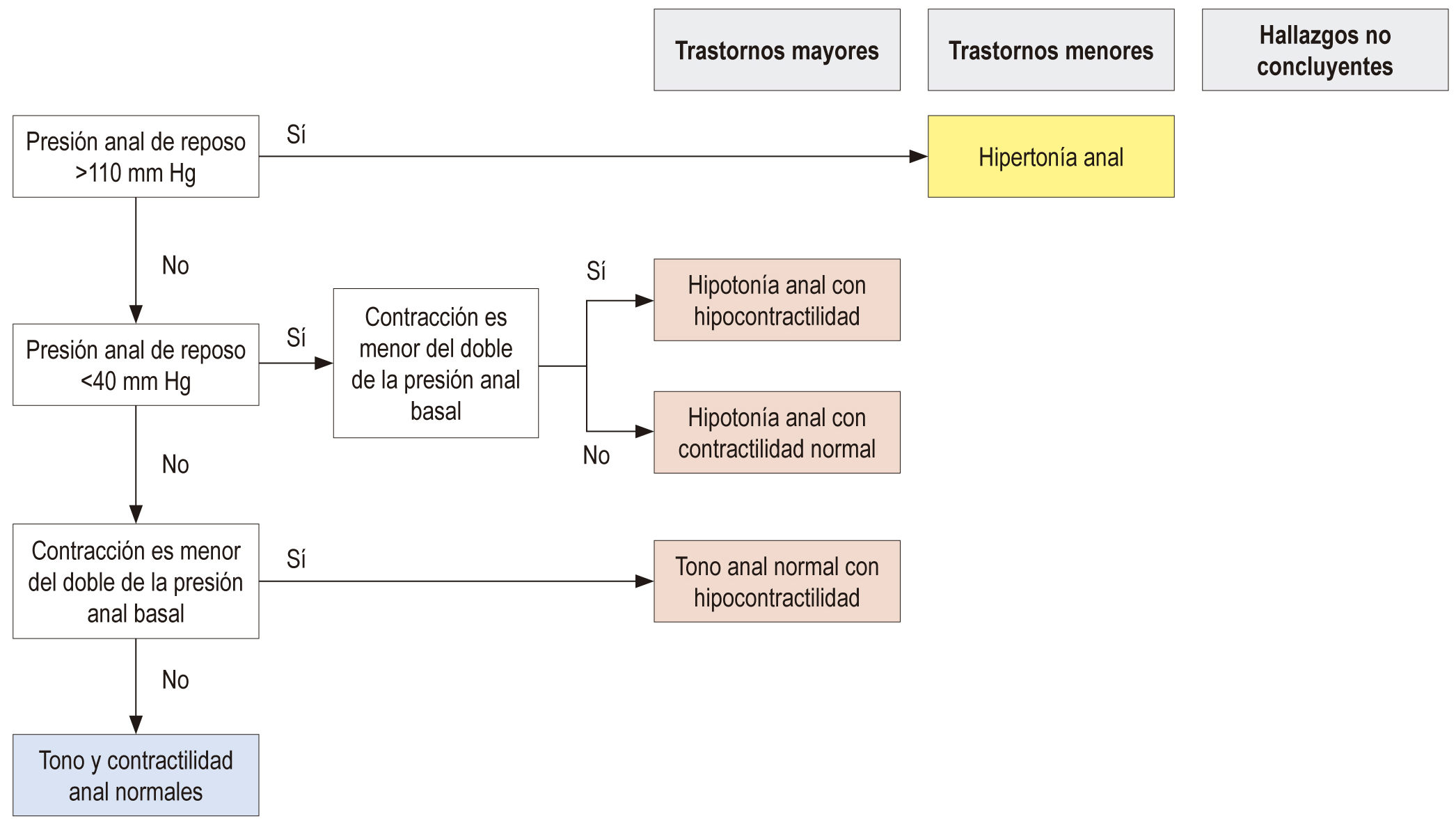
High resolution anorectal manometry is a diagnostic tool, used for anorectal motor and sensory disorders. It consists of a measurement of basal tone and anal contraction, it also performs the push maneuver, rectoanal inhibitory reflex (RAIR) and rectal sensory parameters. The conventional interpretation of anorectal manometry focuses on describing in isolation the dysfunctional anatomical region. However, with the London classification It`s sought to standardize the report of these results, grouping them into major, minor disorders and inconclusive findings, like to the Chicago`s classification for esophageal motor disorders.
Downloads
References
Bharucha AE, Rao SS. An update on anorectal disorders for gastroenterologists. Gastroenterology. 2014;146(1):37-45. doi: https://doi.org/10.1053/j.gastro.2013.10.062.
Patcharatrakul T, Rao SSC. Update on the pathophysiology and management of anorectal disorders. Gut Liver. 2018;12(4):375-84. doi: https://doi.org/10.5009/gnl17172.
Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, et al. Functional anorectal disorders. Gastroenterology. 2016;S0016-5085(16)00175-X. doi: https://doi.org/10.1053/j.gastro.2016.02.009.
Nuernberg D, Saftoiu A, Barreiros AP, Burmester E, Ivan ET, Clevert DA, et al. EFSUMB recommendations for gastrointestinal ultrasound part 3: endorectal, endoanal and perineal ultrasound. Ultrasound Int Open. 2019;5(1):E34-51. doi: https://doi.org/10.1055/a-0825-6708.
Diamant NE, Kamm MA, Wald A, Whitehead WE. AGA technical review on anorectal testing techniques. Gastroenterology. 1999;116(3):735-60. doi: https://doi.org/10.1016/S0016-5085(99)70195-2.
Heinrich H, Fruehauf H, Sauter M, Steingötter A, Fried M, Schwizer W, et al. The effect of standard compared to enhanced instruction and verbal feedback on anorectal manometry measurements. Neurogastroenterol Motil. 2013;25(3):230-7,e163. doi: https://doi.org/10.1111/nmo.12038.
Basilisco G, Bharucha AE. High-resolution anorectal manometry: an expensive hobby or worth every penny? Neurogastroenterol Motil. 2017;29(8). doi: https://doi.org/10.1111/nmo.13125.
Carrington EV, Heinrich H, Knowles CH, Rao SS, Fox M, Scott SM, et al. Methods of anorectal manometry vary widely in clinical practice: results from an international survey. Neurogastroenterol Motil. 2017;29(8):e13016. doi: https://doi.org/10.1111/nmo.13016.
Carrington EV, Heinrich H, Knowles CH, Fox M, Rao S, Altomare DF, et al. The International Anorectal Physiology Working Group (IAPWG) recommendations: standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil. 2019:e13679. doi: https://doi.org/10.1111/nmo.13679.
Remes-Troche JM, Rao SS. Defecation disorders: neuromuscular aspects and treatment. Curr Gastroenterol Rep. 2006;8:291-9. doi: https://doi.org/10.1007/s11894-006-0049-x.
Demir N, Yuruyen M, Atay K, Yavuzer H, Hatemi I, Doventas A, et al. Prevalence of fecal incontinence and associated risk factors in elderly outpatients: a cross-sectional study. Aging Clin Exp Res. 2017;29(6):1165-71. doi: https://doi.org/10.1007/s40520-017-0723-x.
Vazquez Roque M, Bouras EP. Epidemiology and management of chronic constipation in elderly patients. Clin Interv Aging. 2015;10:919-30. doi: https://doi.org/10.2147/CIA.S54304.
Xu X, Pasricha PJ, Sallam HS, Ma L, Chen JD. Clinical significance of quantitative assessment of rectoanal inhibitory reflex (RAIR) in patients with constipation. J Clin Gastroenterol. 2008;42(6):692-8. doi: https://doi.org/10.1097/MCG.0b013e31814927ba.
Tetangco E, Yan Y, Rao SS. Performing and analyzing high-resolution anorectal manometry. Neuro Gastro Latam Rev. 2018;2:123-32. doi: https://doi.org/10.24875/NGL.19000016.
Carrington EV, Scott SM, Bharucha A, Mion F, Remes-Troche JM, Malcolm A, et al. Expert consensus document: advances in the evaluation of anorectal function. Nat Rev Gastroenterol Hepatol. 2018;15(5):309-23. doi: https://doi.org/10.1038/nrgastro.2018.27.
Lee HJ, Jung KW, Han S, Kim JW, Park SK, Yoon IJ, et al. Normal values for high-resolution anorectal manometry/topography in a healthy Korean population and the effects of gender and body mass index. Neurogastroenterol Motil. 2014;26(4):529-37. doi: https://doi.org/10.1111/nmo.12297.
Carrington EV, Brokjaer A, Craven H, Zarate N, Horrocks EJ, Palit S, et al. Traditional measures of normal anal sphincter function using high-resolution anorectal manometry (HRAM) in 115 healthy volunteers. Neurogastroenterol Motil. 2014;26(5):625-35. doi: https://doi.org/10.1111/nmo.12307.
Noelting J, Ratuapli SK, Bharucha AE, Harvey DM, Ravi K, Zinsmeister AR. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol. 2012;107(10):1530-6. doi: https://doi.org/10.1038/ajg.2012.221.
Oblizajek NR, Gandhi S, Sharma M, Chakraborty S, Muthyala A, Prichard D, et al. Anorectal pressures measured with high-resolution manometry in healthy people-Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterol Motil. 2019;31(7):e13597. doi: https://doi.org/10.1111/nmo.13597.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160-74. doi: https://doi.org/10.1111/nmo.12477.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















