Crohn’s disease with extensive involvement and rare extraintestinal manifestations: A case report
DOI:
https://doi.org/10.22516/25007440.605Keywords:
Crohn´s disease, sclerosing colangitis, enteritisAbstract
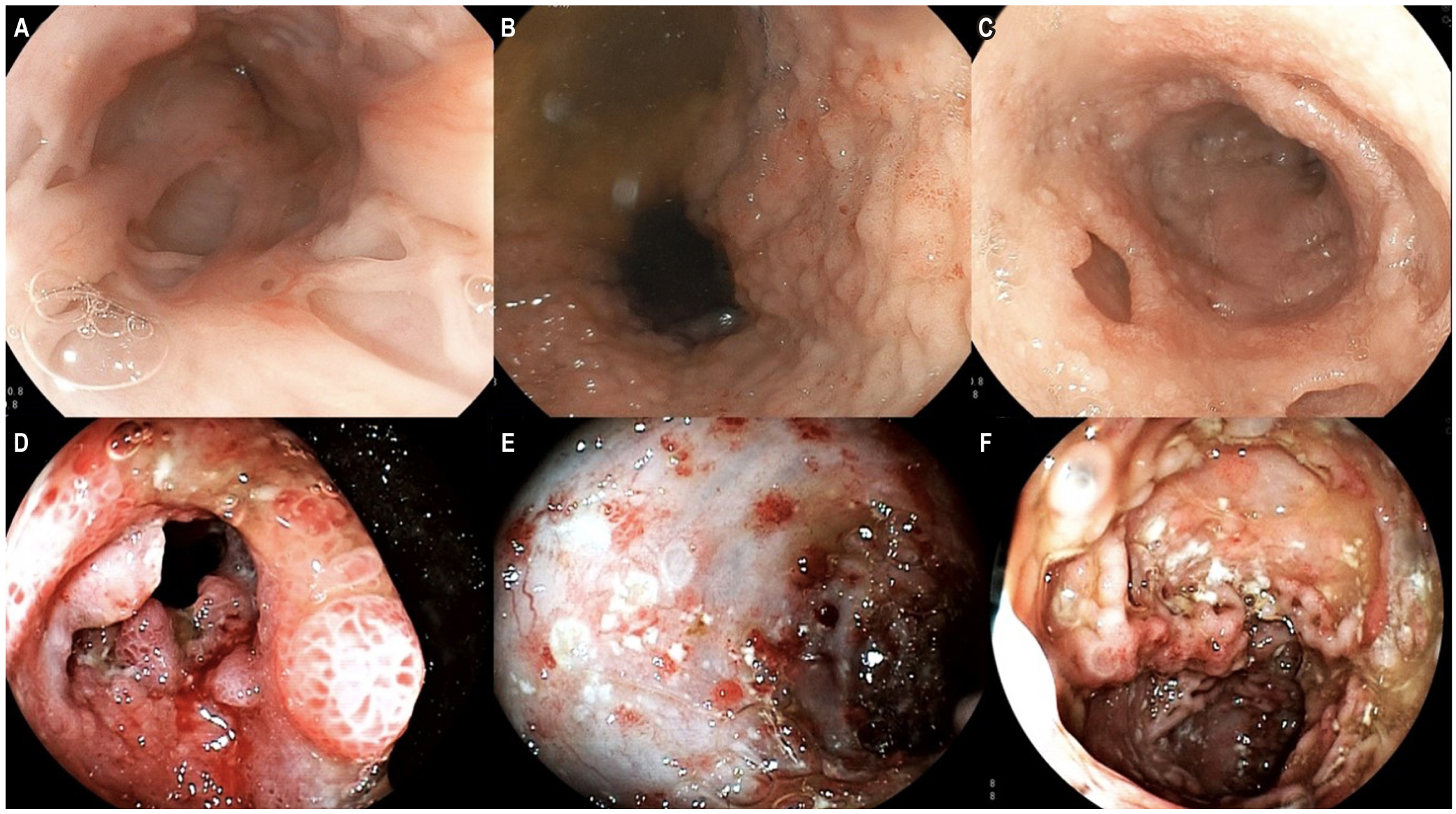
Crohn’s disease (CD) is considered an immunologically mediated entity that involves the digestive tract. It is characterized by transmural inflammation and can affect any part of the digestive tract, from the oral cavity to the anus. Although it is recognized that its severity varies, extensive and multiple organ failure is unusual. We present the case of a young patient, who initially presented with pulmonary symptoms associated with CD. Years later, digestive and bile duct symptoms appeared. Treatment was based on anti-tumor necrosis factor-alpha antibody therapy, resulting in a satisfactory clinical response. The clinical relevance of this case is its full-blown presentation, which includes extensive gastrointestinal involvement and rare extraintestinal manifestations.
Downloads
References
Marín-Jiménez I, Menchén-Viso L, Gomollón-García F. Diagnóstico diferencial de la enfermedad inflamatoria intestinal. 1.a edición. Elsevier; 2012.
Rieder F, Zimmermann EM, Remzi FH, Sandborn WJ. Crohn’s disease complicated by strictures: a systematic review. Gut. 2013;62(7):1072-84. https://doi.org/10.1136/gutjnl-2012-304353
Molnár T, Tiszlavicz L, Gyulai C, Nagy F, Lonovics J. Clinical significance of granuloma in Crohn’s disease. World J Gastroenterol. 2005;11(20):3118-21. https://doi.org/10.3748/wjg.v11.i20.3118
Laube R, Liu K, Schifter M, Yang JL, Suen MK, Leong RW. Oral and upper gastrointestinal Crohn’s disease. J Gastroenterol Hepatol. 2018;33(2):355-364. https://doi.org/10.1111/jgh.13866
Ingle SB, Hinge CR, Dakhure S, Bhosale SS. Isolated gastric Crohn’s disease. World J Clin Cases. 2013;1(2):71-3. https://doi.org/10.12998/wjcc.v1.i2.71
Griffiths AM, Alemayehu E, Sherman P. Clinical features of gastroduodenal Crohn’s disease in adolescents. J Pediatr Gastroenterol Nutr. 1989;8(2):166-71. https://doi.org/10.1097/00005176-198902000-00008
Annunziata ML, Caviglia R, Papparella LG, Cicala M. Upper gastrointestinal involvement of Crohn’s disease: a prospective study on the role of upper endoscopy in the diagnostic work-up. Dig Dis Sci. 2012;57(6):1618-23. https://doi.org/10.1007/s10620-012-2072-0
Gomollón F, Dignass A, Annese V, Tilg H, Van Assche G, Lindsay JO, Peyrin-Biroulet L, Cullen GJ, Daperno M, Kucharzik T, Rieder F, Almer S, Armuzzi A, Harbord M, Langhorst J, Sans M, Chowers Y, Fiorino G, Juillerat P, Mantzaris GJ, Rizzello F, Vavricka S, Gionchetti P; ECCO. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 1: Diagnosis and Medical Management. J Crohns Colitis. 2017;11(1):3-25. https://doi.org/10.1093/ecco-jcc/jjw168
Vennera M, Picado C. Manifestaciones pulmonares de las enfermedades inflamatorias intestinales. Arch Bronconeumol. 2005;41(2):93-8. https://doi.org/10.1157/13070806
Storch I, Sachar D, Katz S. Pulmonary manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2003;9(2):104-15. https://doi.org/10.1097/00054725-200303000-00004
Lunder AK, Hov JR, Borthne A, Gleditsch J, Johannesen G, Tveit K, Viktil E, Henriksen M, Hovde Ø, Huppertz-Hauss G, Høie O, Høivik ML, Monstad I, Solberg IC, Jahnsen J, Karlsen TH, Moum B, Vatn M, Negård A. Prevalence of Sclerosing Cholangitis Detected by Magnetic Resonance Cholangiography in Patients With Long-term Inflammatory Bowel Disease. Gastroenterology. 2016;151(4):660-669.e4. https://doi.org/10.1053/j.gastro.2016.06.021
Kraft SC, Earle RH, Roesler M, Esterly JR. Unexplained bronchopulmonary disease with inflammatory bowel disease. Arch Intern Med. 1976;136(4):454-9.
Massart A, Hunt DP. Pulmonary Manifestations of Inflammatory Bowel Disease. Am J Med. 2020;133(1):39-43. https://doi.org/10.1016/j.amjmed.2019.07.007
Tulic MK, Piche T, Verhasselt V. Lung-gut cross-talk: evidence, mechanisms and implications for the mucosal inflammatory diseases. Clin Exp Allergy. 2016;46(4):519-28. https://doi.org/10.1111/cea.12723
Fung BM, Lindor KD, Tabibian JH. Cancer risk in primary sclerosing cholangitis: Epidemiology, prevention, and surveillance strategies. World J Gastroenterol. 2019;25(6):659-671. https://doi.org/10.3748/wjg.v25.i6.659
Zheng HH, Jiang XL. Increased risk of colorectal neoplasia in patients with primary sclerosing cholangitis and inflammatory bowel disease: a meta-analysis of 16 observational studies. Eur J Gastroenterol Hepatol. 2016;28(4):383-90. https://doi.org/10.1097/MEG.0000000000000576
Colombel JF, Sands BE, Rutgeerts P, Sandborn W, Danese S, D’Haens G, Panaccione R, Loftus EV Jr, Sankoh S, Fox I, Parikh A, Milch C, Abhyankar B, Feagan BG. The safety of vedolizumab for ulcerative colitis and Crohn’s disease. Gut. 2017;66(5):839-851. https://doi.org/10.1136/gutjnl-2015-311079
Lynch KD, Chapman RW, Keshav S, Montano-Loza AJ, Mason AL, Kremer AE, Vetter M, de Krijger M, Ponsioen CY, Trivedi P, Hirschfield G, Schramm C, Liu CH, Bowlus CL, Estes DJ, Pratt D, Hedin C, Bergquist A, de Vries AC, van der Woude CJ, Yu L, Assis DN, Boyer J, Ytting H, Hallibasic E, Trauner M, Marschall HU, Daretti LM, Marzioni M, Yimam KK, Perin N, Floreani A, Beretta-Piccoli BT, Rogers JK; International Primary Sclerosing Cholangitis Study Group (IPSCSG), Levy C. Effects of Vedolizumab in Patients With Primary Sclerosing Cholangitis and Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2020;18(1):179-187.e6. https://doi.org/10.1016/j.cgh.2019.05.013
Tremaine WJ. Gastroduodenal Crohn’s disease: medical management. Inflamm Bowel Dis. 2003;9(2):127-8; discussion 131. https://doi.org/10.1097/00054725-200303000-00008
Nugent FW, Roy MA. Duodenal Crohn’s disease: an analysis of 89 cases. Am J Gastroenterol. 1989;84(3):249-54.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














