Macroamylasemia at the Hospital Víctor Lazarte Echegaray in Trujillo (Peru): Case report
DOI:
https://doi.org/10.22516/25007440.620Keywords:
Macroamylasemia, Hyperamylasemia, Acute pancreatitisAbstract
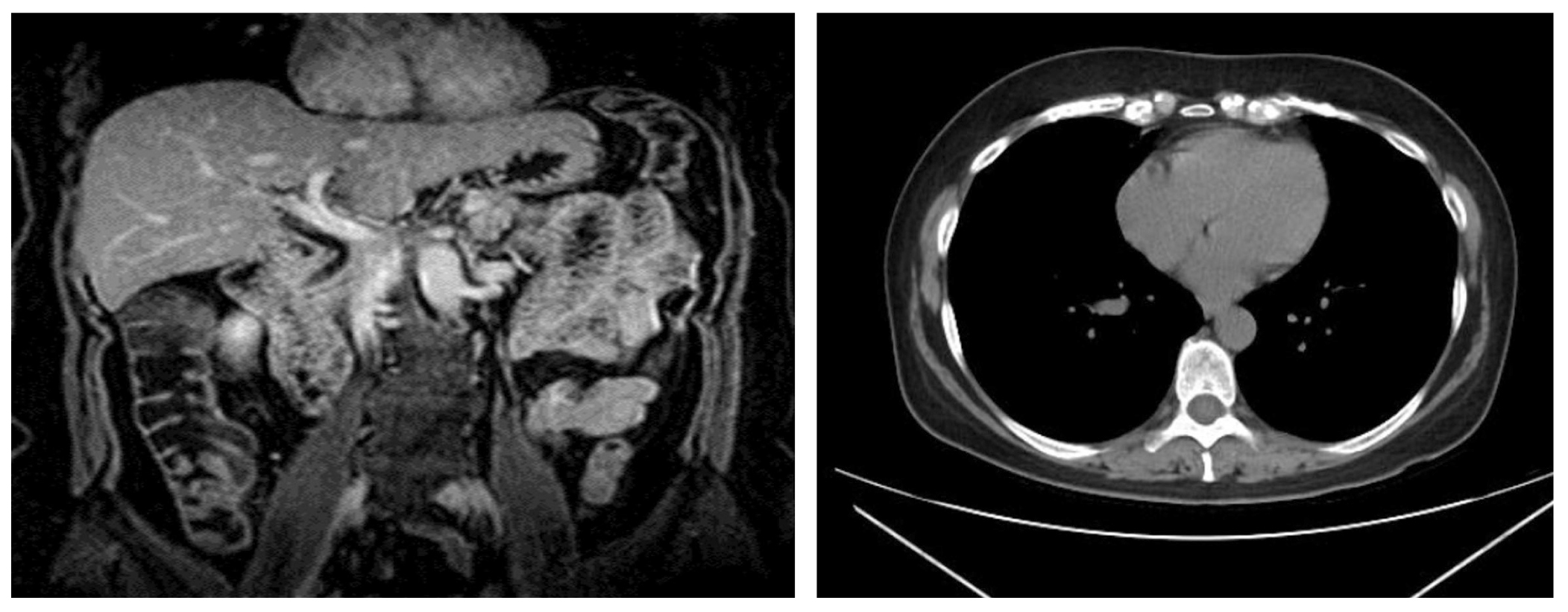
Macroamylasemia should be suspected in any patient with a persistent catalytic increase of plasma α-amylase but no other clinical signs of abdominal pain after ruling out other causes of pancreatic and extra-pancreatic disease. The binding of α-amylase complexes with immunoglobulin, most commonly immunoglobulin A, characterizes this condition. Macroamylasemia is classified into three kinds. To prevent unnecessary procedures, it is critical to make a differential diagnosis of other conditions that can cause amylase increase. The present article reports the case of a 53-year-old female patient who was admitted to the emergency room with abdominal pain and hyperamylasemia, who was initially diagnosed with acute pancreatitis.
Downloads
References
Banks PA, Bollen TL, Dervenis Ch, Gooszeng G, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis-2012: Revision of Atlanta clasification and definitions by international consensus. Gut. 2013;62:102-11. https://doi.org/10.1136/gutjnl-2012-302779
Yokoe M, Takada T, Mayumi T, Yoshida M, Isaji S, Wada K, et al. Japanese guidelines for the management of acute pancreatitis: Japanese Guidelines 2015. J Hepatobiliary Pancreat Sci. 2015;22:405-32. https://doi.org/10.1002/jhbp.259
Crockett SD, Wani S, Gardner T, Falck-Ytter Y, Barkun A, et al. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018;154(4):1096-101. https://doi.org/10.1053/j.gastro.2018.01.032
Greenberg JA, Hsu J, Bawazeer M, Marshall J, Friedrich J, Nathens A, et al. Clinical practice guideline: management of acute pancreatitis. Can J Surg. 2016;59(2):128-40. https://doi.org/10.1503/cjs.015015
Wiederkehr JC, Wiederkehr B, Wiederkehr E, Carvalho C. Nonspecific Hyperamylasemia: A Case Report. JOP. 2013;14(1):74-6. https://doi.org/10.6092/1590-8577/1216
Sánchez-Molina Acosta MI, Chueca MP, Quílez D, Vergara E. ¿Macroamilasemia o hiperamilasemia en un paciente con dolor abdominal? Rev Lab Clin. 2016;9(1):13-6. https://doi.org/10.1016/j.labcli.2015.08.003
Pezzilli R, Andreone P, Morselli-Labate AM, Sama C, Billi P, Cursaro C, et al. Serum pancreatic enzyme concentrations in chronic viral liver diseases. Dig Dis Sci. 1999;44:350-5. https://doi.org/10.1023/A:1026662719514
Antonini F, Pezzilli R, Angelelli L, Macarri G. Pancreatic disorders in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2016;7(3):276-82. https://doi.org/10.4291/wjgp.v7.i3.276
Berk JE, Kizu H, Wilding P, Searcy RL. Macroamylasemia: a newly recognized cause for elevated serum amylase activity. N Engl J Med. 1967;277:941-6. https://doi.org/10.1056/NEJM196711022771801
Šimac V, Špelić M, Devčić B, Rački S. Diagnosing macroamylasemia in unexplained hyperamylasemia. Acta Med Croatica. 2017;71(1)63-7.
Oette M. Macroamylasemia. En: Lang F (editor). Encyclopedia of Molecular Mechanisms of Disease. Berlín, Springer: 2009. p. 1241-1242.
Vahedi A, Mehramouz B, Maroufi P, Pourlak T, Rezvanpour R, Shokouhi B, et al. Determining the Frequency of Macroamylasemia in Patients with Hyperamylasemia using PEG Precipitation Method. J Clin Diag Res. 2018;12(5):EC10-EC13. https://doi.org/10.7860/JCDR/2018/34148.11466
Levitt MD, Ellis C. A rapid and simple assay to determine if macroamylase is the cause of hyperamylasemia. Gastroenterol. 1982;83(2):378-82. https://doi.org/10.1016/S0016-5085(82)80331-4
Forsman RW. Macroamylase: Prevalence, distribution of age, sex, amylase activity, and electrophoretic mobility. Clin Biochem. 1986;19(4):250-3. https://doi.org/10.1016/S0009-9120(86)80036-4
Warshaw AL, Hawboldt MM. Puzzling persistent hyperamylasemia, probably neither pancreatic nor pathologic. Am J Surg. 1988;155(3):453-6. https://doi.org/10.1016/S0002-9610(88)80112-0
Rabsztyn A, Green P, Berti I, Fasano A, Perman J, Karoly H. Macroamylasemia in Patients With Celiac Disease. Am J Gastroenterol. 2001;96(4):1096-100. https://doi.org/10.1111/j.1572-0241.2001.03746.x
Yoshida E, Tsuruoka T, Suzuki M, Asahara M, Okazaki T, Kadohno N, et al. [Sex and age distribution of patients with macroamylasemia found in the daily isoenzyme analysis]. Rinsho Byori. 1998;46(5):473-8.
Masuda H, Tsukada T, Nakayama M, Kitamura M. A study on 41-cases of macroamylasemia detected in a period of 15 months. Chemistry. 1983;27:201-7.
Cutolo M, Sulli A, Barone A, Picciotto A, Mangravtti S, Seriolo B, et al. Macroamylasemia: a possible cause of unexplained hyperamylasemia in rheumatoid arthritis. Br J Rheumatol. 1995;34(3):290-2. https://doi.org/10.1093/rheumatology/34.3.290
Goto H, Wakui H, Komatsuda A, Imai H, Miura A, Fujita K, et al. Simultaneous Macroamylasemia and Macrolipasemia in a Patient with Systemic Lupus Erythematosus in Remission. Intern Med. 2000;39(12):1115-8. https://doi.org/10.2169/internalmedicine.39.1115
Okada S, Komatsu N, Osaka A, Yoshida M, Sakamoto S, Miura Y, et al. IgG (kappa type) binding macroamylasemia complicated with immunoblastic lymphadenopathy-like T cell lymphoma. Nippon Naika Gakkai Zasshi. 1989;78(4):519-22. https://doi.org/10.2169/naika.78.519
Fujimura Y, Nishishita C, Uchida J, Iida M. Macroamylasemia associated with ulcerative colitis. J Mol Med. 1995;73:95-7. https://doi.org/10.1007/BF00270584
Eleccion C, Hathaway A. Macroamylasemia in HIV infection. Tex Med. 1998;94(12):77-9.
Levitt MD, Goetzl EJ, Cooperbani SR. Two forms of macroamylasemia. Lancet. 1968;291(7549):95758. https://doi.org/10.1016/S0140-6736(68)90907-0
Fridhandler, Berk E. Macroamylasemia. Advances Clin Chem. 1978;20:267-86. https://doi.org/10.1016/S0065-2423(08)60024-4
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














