Experience in endoscopic retrograde cholangiopancreatography management of postcholecystectomy biliary leak in a Colombian referral hospital
DOI:
https://doi.org/10.22516/25007440.905Keywords:
Cholecystectomy, biliary leak, Sphincterotomy, Biliary stent, ERCPAbstract
Introduction: Postcholecystectomy biliary leak is rare. Management is mainly endoscopic, but in the literature, there is no consensus on the first-line technique between sphincterotomy, biliary stent, or combination.
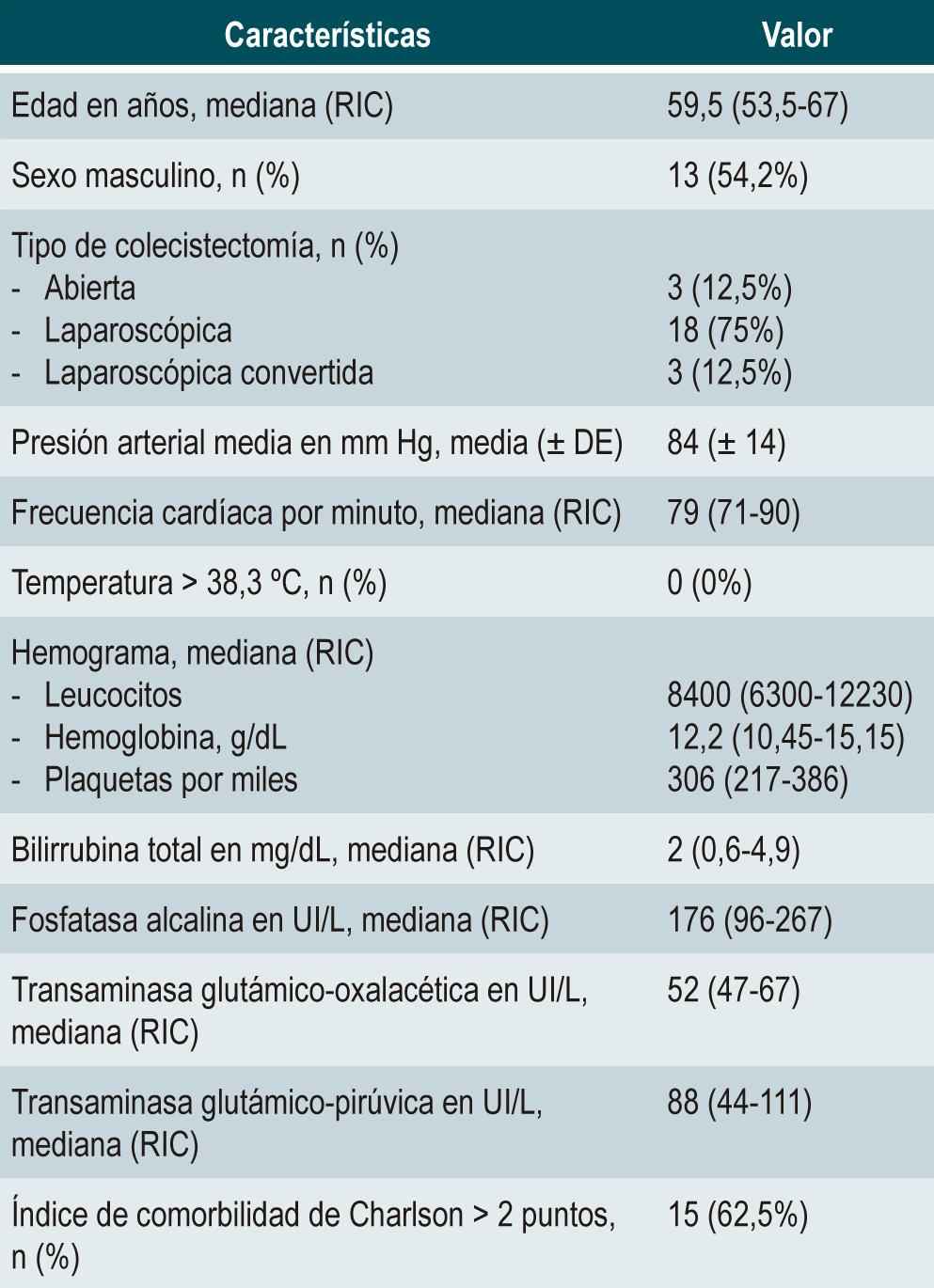
Materials and methods: A case series study was conducted that included all ERCP performed at the San Ignacio University Hospital in Bogotá, Colombia, between January 2010 and March 2021 due to biliary leak after cholecystectomy. Demographic characteristics, clinical manifestations, resolution, adverse events, and hospital length stay were recorded according to the endoscopic technique.
Results: 24 patients with postcholecystectomy biliary leak managed with ERCP were included. The median age was 59 years (interquartile range [IQR]: 53.5-67). In 75% the surgery was laparoscopic. The most frequent clinical manifestation was increased biliary drainage > 150 mL/24 hours (50%), followed by abdominal pain (39%). The main fistula’s location was the cystic duct in 40%. Management with sphincterotomy was 25%, with a biliary stent, 8.4%, and combined, 66%; leak resolution occurred in 100%, 50%, and 87%, respectively, with a shorter hospital length stay in the combined management of 3.5 days compared to four days in sphincterotomy. Only one adverse bleeding event occurred in the sphincterotomy group.
Conclusion: Sphincterotomy and combined therapy are options with reasonable resolution rates and low hospital length stay for managing postcholecystectomy biliary leak. Prospective, randomized, and multicenter trials will be required to define the best technique.
Downloads
References
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part III: liver, biliary tract, and pancreas. Gastroenterology. 2009;136(4):1134-1144. https://doi.org/10.1053/j.gastro.2009.02.038
Portincasa P, Di Ciaula A, de Bari O, Garruti G, Palmieri VO, Wang DQ. Management of gallstones and its related complications. Expert Rev Gastroenterol Hepatol. 2016;10(1):93-112. https://doi.org/10.1586/17474124.2016.1109445
Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology. 2019;156(1):254-272.e11. https://doi.org/10.1053/j.gastro.2018.08.063
Lamberts MP. Indications of cholecystectomy in gallstone disease. Curr Opin Gastroenterol. 2018;34(2):97-102. https://doi.org/10.1097/MOG.0000000000000419
Littlefield A, Lenahan C. Cholelithiasis: Presentation and Management. J Midwifery Womens Health. 2019;64(3):289-297. https://doi.org/10.1111/jmwh.12959
Hugh TB, Chen FC, Hugh TJ, Li B. Laparoscopic cholecystectomy. A prospective study of outcome in 100 unselected patients. Med J Aust. 1992;156(5):318-20. https://doi.org/10.5694/j.1326-5377.1992.tb139786.x
Duca S, Bãlã O, Al-Hajjar N, Lancu C, Puia IC, Munteanu D, et al. Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB (Oxford). 2003;5(3):152-8. https://doi.org/10.1080/13651820310015293
Ashfaq A, Ahmadieh K, Shah AA, Chapital AB, Harold KL, Johnson DJ. The difficult gall bladder: Outcomes following laparoscopic cholecystectomy and the need for open conversion. Am J Surg. 2016;212(6):1261-1264. https://doi.org/10.1016/j.amjsurg.2016.09.024
Nuzzo G, Giuliante F, Giovannini I, Ardito F, D’Acapito F, Vellone M, et al. Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg. 2005;140(10):986-92. https://doi.org/10.1001/archsurg.140.10.986
Kholdebarin R, Boetto J, Harnish JL, Urbach DR. Risk factors for bile duct injury during laparoscopic cholecystectomy: a case-control study. Surg Innov. 2008;15(2):114-9. https://doi.org/10.1177/1553350608318144
Kohn JF, Trenk A, Kuchta K, Lapin B, Denham W, Linn JG, et al. Characterization of common bile duct injury after laparoscopic cholecystectomy in a high-volume hospital system. Surg Endosc. 2018;32(3):1184-1191. https://doi.org/10.1007/s00464-017-5790-8
Darnis B, Mohkam K, Cauchy F, Cazauran JB, Bancel B, Rode A, et al. A systematic review of the anatomical findings of multiple gallbladders. HPB (Oxford). 2018;20(11):985-991. https://doi.org/10.1016/j.hpb.2018.04.002
Maddah G, Rajabi Mashhadi MT, Parvizi Mashhadi M, Nooghabi MJ, Hassanpour M, Abdollahi A. Iatrogenic injuries of the extrahepatic biliary system. J Surg Res. 2017;213:215-221. https://doi.org/10.1016/j.jss.2015.11.032
Rio-Tinto R, Canena J. Endoscopic Treatment of Post-Cholecystectomy Biliary Leaks. GE Port J Gastroenterol. 2021;28(4):265-273. https://doi.org/10.1159/000511527
Copelan A, Bahoura L, Tardy F, Kirsch M, Sokhandon F, Kapoor B. Etiology, Diagnosis, and Management of Bilomas: A Current Update. Tech Vasc Interv Radiol. 2015;18(4):236-43. https://doi.org/10.1053/j.tvir.2015.07.007
Sandha GS, Bourke MJ, Haber GB, Kortan PP. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc. 2004;60(4):567-74. https://doi.org/10.1016/S0016-5107(04)01892-9
Adler DG, Papachristou GI, Taylor LJ, McVay T, Birch M, Francis G, et al. Clinical outcomes in patients with bile leaks treated via ERCP with regard to the timing of ERCP: a large multicenter study. Gastrointest Endosc. 2017;85(4):766-772. https://doi.org/10.1016/j.gie.2016.08.018
Hajjar NA, Tomuş C, Mocan L, Mocan T, Graur F, Iancu C, et al. Management of bile duct injuries following laparoscopic cholecystectomy: long-term outcome and risk factors influencing biliary reconstruction. Chirurgia (Bucur). 2014;109(4):493-9.
Abbas A, Sethi S, Brady P, Taunk P. Endoscopic management of postcholecystectomy biliary leak: When and how? A nationwide study. Gastrointest Endosc. 2019;90(2):233-241.e1. https://doi.org/10.1016/j.gie.2019.03.1173
Chathadi KV, Chandrasekhara V, Acosta RD, Decker GA, Early DS, Eloubeidi MA, et al. The role of ERCP in benign diseases of the biliary tract. Gastrointest Endosc. 2015;81(4):795-803. https://doi.org/10.1016/j.gie.2014.11.019
Dumonceau JM, Tringali A, Blero D, Devière J, Laugiers R, Heresbach D, et al. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012;44(3):277-98. https://doi.org/10.1055/s-0031-1291633
Ahmad DS, Faulx A. Management of Postcholecystectomy Biliary Complications: A Narrative Review. Am J Gastroenterol. 2020;115(8):1191-1198. https://doi.org/10.14309/ajg.0000000000000704
Tarantino I, Baron TH, Ligresti D. Biliary surgery adverse events, including liver transplantation. En: Baron TH, Kozarek RA, Carr-Locke DL, (editores). ERCP. 3.a edición. Filadelfia: Elsevier; 2019. p. 422-31. https://doi.org/10.1016/B978-0-323-48109-0.00044-4
Shabanzadeh DM. Incidence of gallstone disease and complications. Curr Opin Gastroenterol. 2018;34(2):81-89. https://doi.org/10.1097/MOG.0000000000000418
Festi D, Reggiani ML, Attili AF, Loria P, Pazzi P, Scaioli E, et al. Natural history of gallstone disease: Expectant management or active treatment? Results from a population-based cohort study. J Gastroenterol Hepatol. 2010;25(4):719-24. https://doi.org/10.1111/j.1440-1746.2009.06146.x
Pandit N, Yadav TN, Awale L, Deo KB, Dhakal Y, Adhikary S. Current Scenario of Postcholecystectomy Bile Leak and Bile Duct Injury at a Tertiary Care Referral Centre of Nepal. Minim Invasive Surg. 2020;2020:4382307. https://doi.org/10.1155/2020/4382307
Rainio M, Lindström O, Udd M, Haapamäki C, Nordin A, Kylänpää L. Endoscopic Therapy of Biliary Injury After Cholecystectomy. Dig Dis Sci. 2018;63(2):474-480. https://doi.org/10.1007/s10620-017-4768-7
Angileri SA, Rodà GM, Savoldi AP, Meglio LD, Signorelli G, Ierardi AM, et al. Imaging findings and available percutaneous techniques for the treatment of bile leaks after hepatobiliary surgery. Ann Gastroenterol. 2020;33(6):675-679. https://doi.org/10.20524/aog.2020.0532
Haidar H, Manasa E, Yassin K, Suissa A, Kluger Y, Khamaysi I. Endoscopic treatment of post-cholecystectomy bile leaks: a tertiary center experience. Surg Endosc 2021;35(3):1088-1092. https://doi.org/10.1007/s00464-020-07472-0
Mavrogiannis C, Liatsos C, Papanikolaou IS, Karagiannis S, Galanis P, Romanos A. Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy biliary leaks: a prospective randomized study. Eur J Gastroenterol Hepatol. 2006;18(4):405-409. https://doi.org/10.1097/00042737-200604000-00014
Chandra S, Murali AR, Masadeh M, Silverman WB, Johlin FC. Comparison of Biliary Stent versus Biliary Sphincterotomy Alone in the Treatment of Bile Leak. Dig Dis. 2020;38(1):32-37. https://doi.org/10.1159/000499872
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |