Factores de riesgo para fibrosis hepática en pacientes diabéticos con enfermedad renal cronica terminal
Risk Factors for Liver Fibrosis in Diabetic Patients with End-stage Renal Disease
DOI:
https://doi.org/10.22516/25007440.1061Palabras clave:
Cirrosis hepátca, enfermedad renal crónica terminal, Diabetes Mellitus, Diálisis, Diagnóstico por imagen de elasticidadResumen
Introducción: la cirrosis hepática es la cuarta causa de muerte en el mundo. Actualmente, la enfermedad hepática por depósito de grasa es la causa más frecuente de hepatopatía crónica en la mayoría de los países. La identificación de factores de riesgo para la presencia de fibrosis hepática en una población con enfermedad renal crónica terminal puede facilitar el diagnóstico temprano de esta complicación y permitir la activación de protocolos de seguimiento para disminuir la morbimortalidad en estos pacientes.
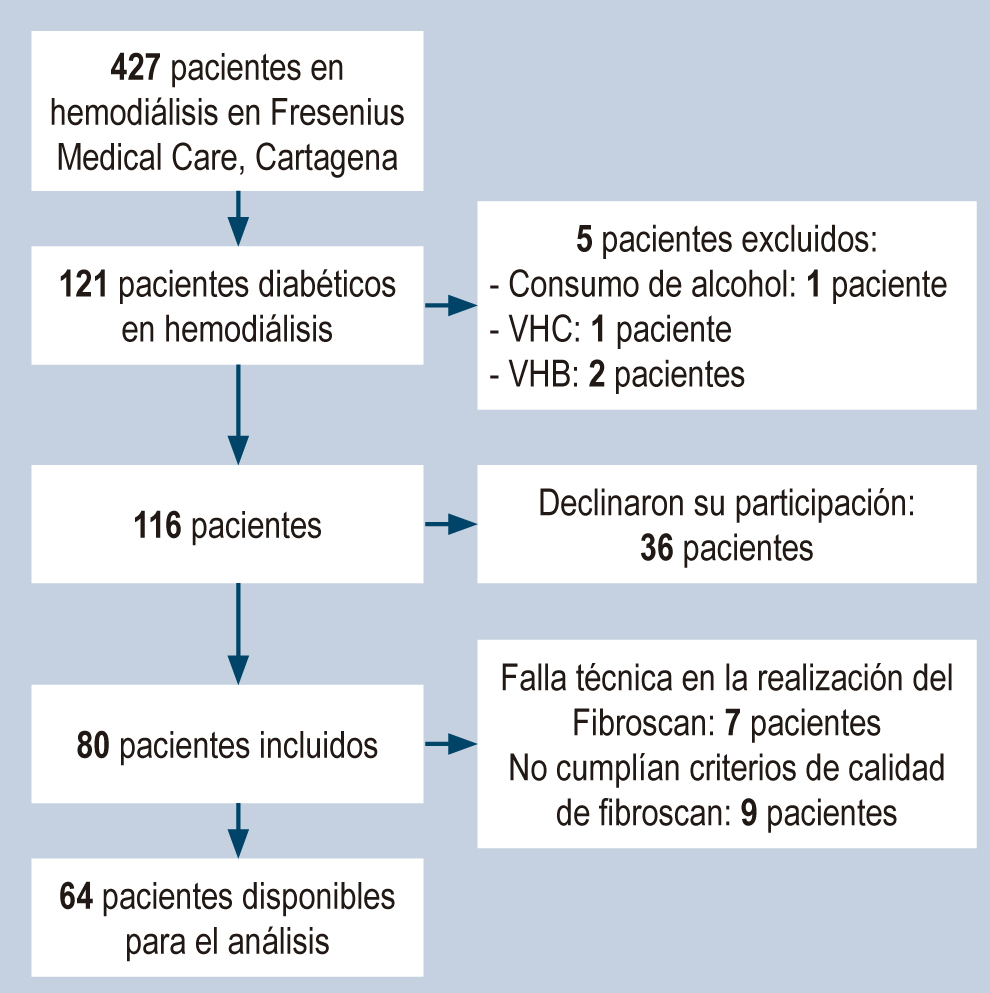
Metodología: se realizó un estudio de corte transversal y analítico. Se incluyeron pacientes en hemodiálisis, mayores de 18 años con diagnóstico de diabetes mellitus y de enfermedad renal crónica terminal. El contraste de hipótesis se realizó a través de la prueba de chi cuadrado y la T de Student, según correspondiera. La significación estadística se estableció con un valor p = 0,05.
Resultados: se observó una prevalencia de fibrosis hepática significativa y cirrosis del 17%. Los factores asociados a la presencia de fibrosis hepática fueron los antecedentes de enfermedad cerebrovascular, la enfermedad vascular periférica, el índice de masa corporal (IMC), el colesterol total, la hemoglobina glicosilada, el sodio y el aspartato-aminotransferasa (AST). No se observó relación entre el puntaje de NAFLD (enfermedad del hígado graso no alcohólico), el índice APRI (AST to Platelet Ratio Index) y la presencia de fibrosis.
Conclusión: la prevalencia de fibrosis hepática significativa en pacientes con diabetes y ERCT es similar a la reportada en otras poblaciones de pacientes con diabetes. Sin embargo, algunos factores, como el IMC, podrían comportarse de forma diferente y favorecer la aparición de lesión hepática con grados menores de obesidad a los reportados previamente en la literatura.
Descargas
Referencias bibliográficas
Byass P. The global burden of liver disease: A challenge for methods and for public health. BMC Med. 2014;12(1):159. https://doi.org/10.1186/s12916-014-0159-5
Pappachan JM, Babu S, Krishnan B, Ravindran NC. Non-alcoholic Fatty Liver Disease: A Clinical Update. J Clin Transl Hepatol. 2017;5(4):384-393. https://doi.org/10.14218/JCTH.2017.00013
European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388-402. https://doi.org/10.1016/j.jhep.2015.11.004
Önnerhag K, Dreja K, Nilsson PM, Lindgren S. Increased mortality in non-alcoholic fatty liver disease with chronic kidney disease is explained by metabolic comorbidities. Clin Res Hepatol Gastroenterol. 2019;43(5):542-50. https://doi.org/10.1016/j.clinre.2019.02.004
Silvariño R, Gadola L, Ríos P. Obesidad y Enfermedad Renal Crónica. Rev Urug Med Int. 2(3):3-23. https://doi.org/10.26445/rmu.2.3.1
Lee YJ, Wang CP, Hung WC, Tang WH, Chang YH, Hu DW, et al. Common and unique factors and the bidirectional relationship between chronic kidney disease and nonalcoholic fatty liver in type 2 diabetes patients. Diabetes, Metab Syndr Obes Targets Ther. 2020;13:1203-14. https://doi.org/10.2147/DMSO.S237700
Chinnadurai R, Ritchie J, Green D, Kalra PA. Non-alcoholic fatty liver disease and clinical outcomes in chronic kidney disease. Nephrol Dial Transplant. 2019;34(3):449-57. https://doi.org/10.1093/ndt/gfx381
Wong F, Reddy KR, O›Leary JG, Tandon P, Biggins SW, Garcia-Tsao G, et al. Impact of Chronic Kidney Disease on Outcomes in Cirrhosis. Liver Transplant. 2019;25(6):870-80. https://doi.org/10.1002/lt.25454
Vanegas CM, Restrepo C, Vargas N, Marín AE. Caracterización de pacientes con enfermedad del hígado graso no alcohólica en un hospital de alta complejidad en 2013. Rev Colomb Gastroenterol. 2014;29(4):342-6. https://doi.org/10.22516/25007440.421
Rafael J, Ángel M, Salcedo Ó, Wady D, Felipe J, Quijano CA, et al. Hígado graso no alcohólico en consulta de gastroenterología. Repertorio de Medicina y Cirugía. 2016;5(4):210-8.
Sandrin L, Fourquet B, Hasquenoph JM, Yon S, Fournier C, Mal F, et al. Transient elastography: A new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29(12):1705-13. https://doi.org/10.1016/j.ultrasmedbio.2003.07.001
Castéra L, Foucher J, Bernard PH, Carvalho F, Allaix D, Merrouche W, et al. Pitfalls of liver stiffness measurement: A 5-year prospective study of 13,369 examinations. Hepatology. 2010;51(3):828-35. https://doi.org/10.1002/hep.23425
Eddowes PJ, Sasso M, Allison M, Tsochatzis E, Anstee QM, Sheridan D, et al. Accuracy of FibroScan Controlled Attenuation Parameter and Liver Stiffness Measurement in Assessing Steatosis and Fibrosis in Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2019;156(6):1717-30. https://doi.org/10.1053/j.gastro.2019.01.042
Siddiqui MS, Vuppalanchi R, Van Natta ML, Hallinan E, et al. Vibration-controlled Transient Elastography to Assess Fibrosis and Steatosis in Patients With Nonalcoholic Fatty Liver Disease. Clin Gastroenterol Hepatol. 2019;17(1):156-163.e2. https://doi.org/10.1016/j.cgh.2018.04.043
Björkström K, Franzén S, Eliasson B, Miftaraj M, Gudbjörnsdottir S, Trolle-Lagerros Y, et al. Risk Factors for Severe Liver Disease in Patients With Type 2 Diabetes. Clin Gastroenterol Hepatol. 2019;17(13):2769-2775.e4. https://doi.org/10.1016/j.cgh.2019.04.038
Pimpin L, Cortez-Pinto H, Negro F, Corbould E, Lazarus JV, Webber L, et al. Burden of liver disease in Europe: Epidemiology and analysis of risk factors to identify prevention policies. J Hepatol. 2018;69(3):718-35. https://doi.org/10.1016/j.jhep.2018.05.011
Ekstedt M, Hagström H, Nasr P, Fredrikson M, Stål P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61(5):1547-54. https://doi.org/10.1002/hep.27368
Li X, Jiao Y, Xing Y, Gao P. Diabetes Mellitus and Risk of Hepatic Fibrosis/Cirrhosis. Biomed Res Int. 2019;2019: 5308308. https://doi.org/10.1155/2019/5308308
Moreno-del Castillo MC, Sánchez-Rodriguez A, Hernández-Buen Abad JJ, Aguirre-Valadez J, Ruiz I, Garcia-Buen Abad R, et al. Importance of Evaluating Cardiovascular Risk and Hepatic Fibrosis in Patients With Newly Diagnosed Nonalcoholic Fatty Liver Disease. Clin Gastroenterol Hepatol. 2019;17(5):997-9. https://doi.org/10.1016/j.cgh.2018.07.039
Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846-854. https://doi.org/10.1002/hep.21496
Wong VWS, Adams LA, de Lédinghen V, Wong GLH, Sookoian S. Noninvasive biomarkers in NAFLD and NASH - current progress and future promise. Nat Rev Gastroenterol Hepatol. 2018;15(8):461-78. https://doi.org/10.1038/s41575-018-0014-9
Alvero-Cruz JR, Correas L, Ronconi M, Férnandez R, Porta J. La bioimpedanciometría eléctrica como método de estimación de la composición corporal, normas prácticas de utilización. Rev Andal Med Deporte. 2011;4(4):167-74.
Tuong TTK, Tran DK, Phu PQT, Hong TND, Dinh TC, Chu DT. Non-alcoholic fatty liver disease in patients with type 2 diabetes: Evaluation of hepatic fibrosis and steatosis using fibroscan. Diagnostics. 2020;10(3):159. https://doi.org/10.3390/diagnostics10030159
Lai LL, Wan Yusoff WNI, Vethakkan SR, Nik Mustapha NR, Mahadeva S, Chan WK. Screening for non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus using transient elastography. J Gastroenterol Hepatol. 2019;34(8):1396-403. https://doi.org/10.1111/jgh.14577
George ES, Roberts SK, Nicoll AJ, Reddy A, Paris T, Itsiopoulos C, et al. Non alcoholic fatty liver disease patients attending two metropolitan hospitals in Melbourne, Australia; high risk status and low prevalence. Intern Med J. 2018;48(11):1369-1376. https://doi.org/10.1111/imj.13973
de Marco R, Locatelli F, Zoppini G, Verlato G, Bonora E, Muggeo M. Cause-specific mortality in type 2 diabetes. The Verona Diabetes Study. Diabetes Care. 1999;22(5):756‐761. https://doi.org/10.2337/diacare.22.5.756
Vora JP, Leese GP, Peters JR, Owens DR. Longitudinal evaluation of renal function in non-insulin-dependent diabetic patients with early nephropathy: effects of angiotensin-converting enzyme inhibition. J Diabetes Complications. 1996;10(2):88-93. https://doi.org/10.1016/1056-8727(95)00003-8
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol 1984;102(4):527-532. https://doi.org/10.1001/archopht.1984.01040030405011
Tsalamandris C, Allen TJ, Gilbert RE, Sinha A, Panagiotopoulos S, Cooper ME, et al. Progressive decline in renal function in diabetic patients with and without albuminuria. Diabetes. 1994;43(5):649-55. https://doi.org/10.2337/diabetes.43.5.649
American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S66-S76. https://doi.org/10.2337/dc20-S006
Caldwell SH, Lee VD, Kleiner DE, Al-Osaimi AMS, Argo CK, Northup PG, et al. NASH and cryptogenic cirrhosis: A histological analysis. Ann Hepatol. 2009;8(4):346-52. https://doi.org/10.1016/S1665-2681(19)31748-X
Hamed AE, Elsahar M, Elwan NM, El-Nakeep S, Naguib M, Soliman HH, et al. Managing diabetes and liver disease association. Arab J Gastroenterol. 2018;19(4):166-79. https://doi.org/10.1016/j.ajg.2018.08.003
Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, et al. The epidemiology of cirrhosis in the United States a population-based study. J Clin Gastroenterol. 2015;49(8):690-6. https://doi.org/10.1097/MCG.0000000000000208
Calès P, Boursier J, Oberti F, Hubert I, Gallois Y, Rousselet MC, et al. FibroMeters: a family of blood tests for liver fibrosis. Gastroenterol Clin Biol. 2008;32(6 Suppl 1):40-51. https://doi.org/10.1016/S0399-8320(08)73992-7
Wai Ch, Greenson J, Fontana R, Kalbfleisch J, Marrero J, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38(2):518-526. https://doi.org/10.1053/jhep.2003.50346
Harrison SA, Oliver D, Arnold HL, Gogia S, Neuschwander-Tetri BA. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008;57(10):1441‐1447. https://doi.org/10.1136/gut.2007.146019
Henry ZH, Argo CK. How to Identify the Patient with Nonalcoholic Steatohepatitis Who Will Progress to Cirrhosis. Gastroenterol Clin North Am. 2020;49(1):45-62. https://doi.org/10.1016/j.gtc.2019.09.002
Leise M, Cárdenas A. Hyponatremia in Cirrhosis: Implications for Liver Transplantation. Liver Transplant. 2018;24(11):1612-21. https://doi.org/10.1002/lt.25327
Patel K, Sebastiani G. Limitations of non-invasive tests for assessment of liver fibrosis. JHEP Reports. 2020;2(2):100067. https://doi.org/10.1016/j.jhepr.2020.100067
Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286-92. https://doi.org/10.1053/jhep.2003.50229
Pais R, Charlotte F, Fedchuk L, Bedossa P, Lebray P, Poynard T, et al. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol. 2013;59(3):550-6. https://doi.org/10.1016/j.jhep.2013.04.027
Vuppalanchi R, Siddiqui MS, Van Natta ML, Hallinan E, Brandman D, Kowdley K, et al. Performance characteristics of vibration-controlled transient elastography for evaluation of nonalcoholic fatty liver disease. Hepatology. 2018;67(1):134-44. https://doi.org/10.1002/hep.29489
Sporea I, Mare R, Popescu A, Nistorescu S, Baldea V, Sirli R, et al. Screening for Liver Fibrosis and Steatosis in a Large Cohort of Patients with Type 2 Diabetes Using Vibration Controlled Transient Elastography and Controlled Attenuation Parameter in a Single-Center Real-Life Experience. J Clin Med. 2020;9(4):1032. https://doi.org/10.3390/jcm9041032
Chen PC, Kao WY, Cheng YL, Wang YJ, Hou MC, Wu JC, et al. The correlation between fatty liver disease and chronic kidney disease. J Formos Med Assoc. 2020;119(1P1):42-50. https://doi.org/10.1016/j.jfma.2019.02.010
Han E, Lee Y. Non-Alcoholic Fatty Liver Disease: The Emerging Burden in Cardiometabolic and Renal Diseases. 2017;41(6):430-7. https://doi.org/10.4093/dmj.2017.41.6.430
Mikolasevic I, Racki S, Bubic I, Jelic I, Stimac D, Orlic L. Chronic kidney disease and nonalcoholic fatty liver disease proven by transient elastography. Kidney Blood Press Res. 2013;37(4-5):305-10. https://doi.org/10.1159/000350158
Targher G, Byrne CD. Non-alcoholic fatty liver disease: An emerging driving force in chronic kidney disease. Nat Rev Nephrol. 2017;13(5):297-310. https://doi.org/10.1038/nrneph.2017.16
Kiapidou S, Liava C, Kalogirou M, Akriviadis E, Sinakos E. Chronic kidney disease in patients with non-alcoholic fatty liver disease: What the Hepatologist should know? Ann Hepatol. 2020;19(2):134-44. https://doi.org/10.1016/j.aohep.2019.07.013
Bassegoda O, Huelin P, Ariza X, Solé C, Juanola A, Gratacós-Ginès J, et al. Development of chronic kidney disease after acute kidney injury in patients with cirrhosis is common and impairs clinical outcomes. J Hepatol. 2020 Jun;72(6):1132-1139. https://doi.org/10.1016/j.jhep.2019.12.020
Ekser B, Contreras AG, Andraus W, Taner T. Current status of combined liver-kidney transplantation. Int J Surg. 2020;82S:149-154. https://doi.org/10.1016/j.ijsu.2020.02.008
Zhou JH, She ZG, Li HL, Cai JJ. Noninvasive evaluation of nonalcoholic fatty liver disease: Current evidence and practice. World J Gastroenterol. 2019;25(11):1307-26. https://doi.org/10.3748/wjg.v25.i11.1307
Vilar-Gomez E, Chalasani N. Non-invasive assessment of non-alcoholic fatty liver disease: Clinical prediction rules and blood-based biomarkers. J Hepatol. 2018;68(2):305-15. https://doi.org/10.1016/j.jhep.2017.11.013
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2023 Revista colombiana de Gastroenterología

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |















