Alergia a la proteína de leche de vaca. Enfoque diagnóstico y terapéutico
DOI:
https://doi.org/10.22516/25007440.379Palabras clave:
alergia a la proteína de la leche de vaca, práctica clínica, guías, diagnóstico, tratamiento, prevención.Resumen
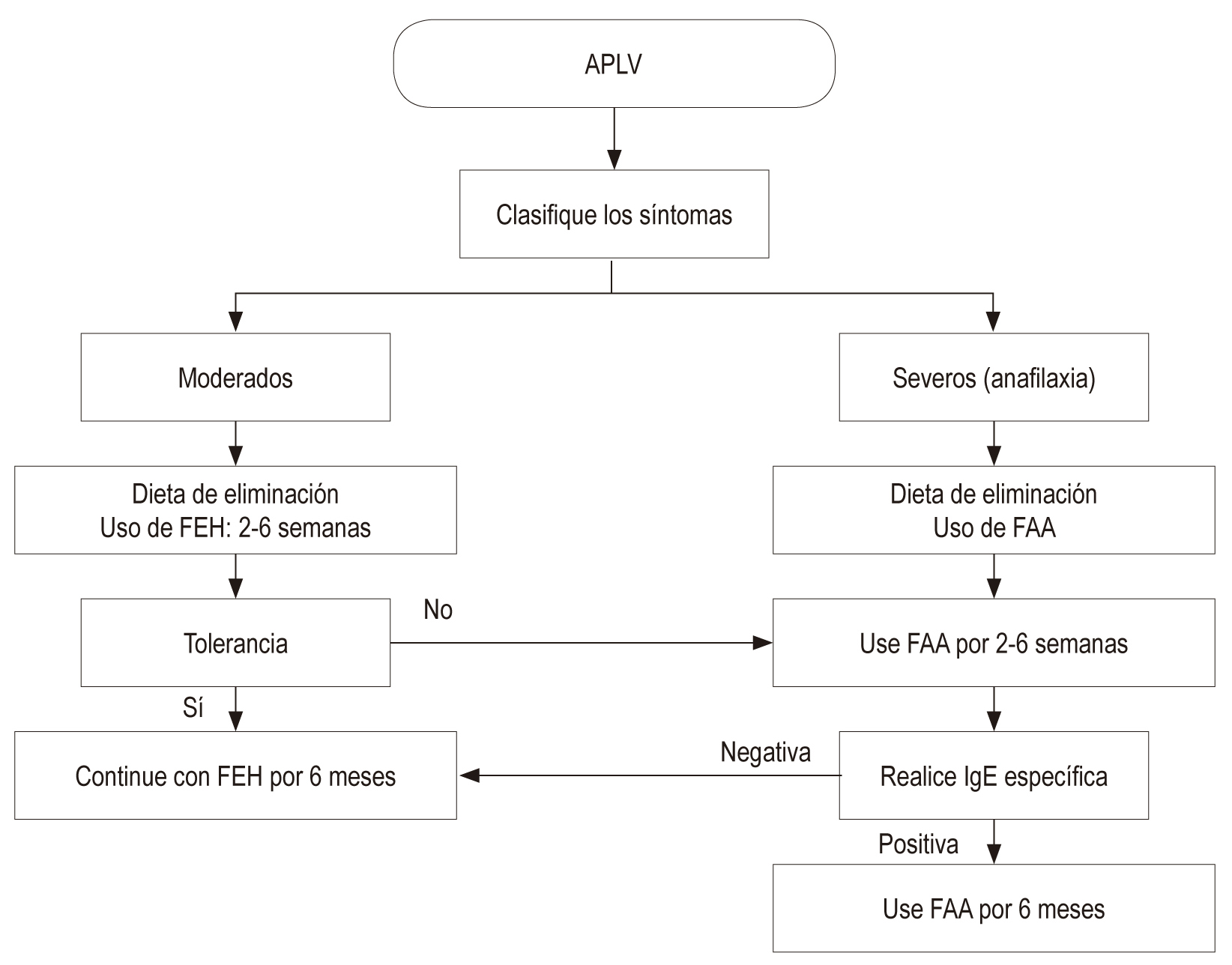
La prevalencia de la alergia a las proteínas de la leche de vaca (APLV) en el ámbito mundial es, aproximadamente, de 1,9 a 4,9 %. En Colombia, esta cifra se desconoce. En un alto porcentaje de los casos, no existe la sospecha por parte del personal de salud, y, por lo tanto, el diagnóstico y el tratamiento se retrasan. Esto acarrea un aumento en el tiempo y en los recursos que emplean los profesionales de la salud y los padres en procura de establecer la etiología del padecimiento de los niños que presentan esta enfermedad. Dentro de este contexto, la historia clínica es fundamental en la sospecha de la APLV, y es especialmente relevante la evaluación de antecedentes, en los cuales se destacan la presencia de la exposición temprana a la proteína, así como la atopia en familiares en primer grado de consanguinidad. La presentación de la APLV puede manifestarse con reacciones inmediatas a nivel digestivo (vómitos, diarrea aguda), cutáneo (urticaria, dermatitis, angioedema) y, con menos frecuencia, a partir de signos respiratorias y sistémicos. Sin embargo, la amplia variedad de manifestaciones clínicas y signos puede ser un reto para el profesional que no se encuentre sensibilizado con la patología, e incluso soslayar este diagnóstico retrasa la suspensión de la proteína de la leche de vaca de la dieta y demora el acceso a un tratamiento eficaz. El tratamiento ideal reconocido es la dieta de exclusión, la cual requiere un estricto cumplimiento. En los niños alimentados con lactancia materna exclusiva, será necesaria la dieta restrictiva de leche y sus derivados en la madre. En quienes no reciben lactancia, se deberá tratar mediante fórmulas de proteínas lácteas extensamente hidrolizadas (FEH) o a base de aminoácidos (FAA). Así bien, el pronóstico es favorable y la mayoría de niños tolerarán las proteínas de la leche de vaca a los 2 años, mientras que en pacientes con polisensibilización el proceso puede prolongarse. En el caso de no alcanzar la tolerancia, la inmunoterapia oral es una opción disponible.
Descargas
Referencias bibliográficas
Koletzko S, Niggemann B, Arato A, Dias JA, Heuschkel R, Husby S, et al. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr. 2012;55(2):221-9. https://doi.org/10.1097/MPG.0b013e31825c9482
Vandenplas Y, Abuabat A, Al-Hammadi S, Aly GS, Miqdady MS, Shaaban SY, et al. Middle East Consensus Statement on the Prevention, Diagnosis, and Management of Cow’s Milk Protein Allergy. Pediatr Gastroenterol Hepatol Nutr. 2014;17(2):61-73. http://dx.doi.org/10.5223/pghn.2014.17.2.61
Boaventura RM, Mendonça RB, Fonseca FA, Mallozi M, Souza FS, Sarni ROS. Nutritional status and food intake of children with cow’s milk allergy. Allergol Immunopathol (Madr). 2019;47(6):544-550. http://dx.doi.org/10.1016/j.aller.2019.03.003
Hill DJ, Firer MA, Shelton MJ, Hosking CS. Manifestations of milk allergy in infancy: clinical and immunologic findings. J Pediatr. 1986;109(2):270-6. https://doi.org/10.1016/S0022-3476(86)80384-5
Mehaudy R, Parisi C, Petriz N, Eymann A, Jauregui MB, Orsi M. Prevalence of cow’s milk protein allergy among children in a university community hospital. Arch Argent Pediatr. 2018;116(3):219-223. https://doi.org/10.5546/aap.2018.219
Høst A, Halken S. A prospective study of cow milk allergy in Danish infants during the first 3 years of life. Clinical course in relation to clinical and immunological type of hypersensitivity reaction. Allergy. 1990;45(8):587-96. https://doi.org/10.1111/j.1398-9995.1990.tb00944.x
Jakobsson I, Lindberg T. A prospective study of cow’s milk protein intolerance in Swedish infants. Acta Paediatr Scand. 1979;68(6):853-9. https://doi.org/10.1111/j.1651-2227.1979.tb08223.x
Santos A, Dias A, Pinheiro JA. Predictive factors for the persistence of cow’s milk allergy. Pediatr Allergy Immunol. 2010;21(8):1127-34. https://doi.org/10.1111/j.1399-3038.2010.01040.x
Kvenshagen B, Halvorsen R, Jacobsen M. Adverse reactions to milk in infants. Acta Paediatr. 2008;97(2):196–200. https://doi.org/10.1111/j.1651-2227.2007.00599.x
Bishop JM, Hill DJ, Hosking CS. Natural history of cow milk allergy: clinical outcome. J Pediatr. 1990;116(6):862-7. https://doi.org/10.1016/S0022-3476(05)80641-9
Høst A, Halken S, Jacobsen HP, Christensen AE, Herskind AM, Plesner K. Clinical course of cow’s milk protein allergy/intolerance and atopic diseases in childhood. Pediatr Allergy Immunol. 2002;13(s15):23-8. https://doi.org/10.1034/j.1399-3038.13.s.15.7.x
Vanto T, Helppilä S, Juntunen-Backman K, Kalimo K, Klemola T, Korpela R, Koskinen P. Prediction of the development of tolerance to milk in children withcow’s milk hypersensitivity. J Pediatr. 2004;144(2):218-22. https://doi.org/10.1016/j.jpeds.2003.10.063
Høst A. Frequency of cow’s milk allergy in childhood. Ann Allergy Asthma Immunol. 2002;89(6 Suppl 1):33-7. https://doi.org/10.1016/S1081-1206(10)62120-5
De Greef E, Hauser B, Devreker T, Veereman-Wauters G, Vandenplas Y. Diagnosis and management of cow’s milk protein allergy in infants. World J Pediatr. 2012;8(1):19-24. https://doi.org/10.1007/s12519-012-0332-x
Wal JM. Cow’s milk proteins/allergens. Ann Allergy Asthma Immunol. 2002;89(6 Suppl 1):3-10. https://doi.org/10.1016/S1081-1206(10)62115-1
Nowak-Wegrzyn A, Fiocchi A. Rare, medium, or well done? The effect of heating and food matrix on food protein allergenicity. Curr Opin Allergy Clin Immunol. 2009;9(3):234-7. https://doi.org/10.1097/ACI.0b013e32832b88e7
Karlsson MR, Rugtveil J, Brandtzaeg P. Allergen-responsive CD41CD251 regulatory cells in children who have outgrown cow’s milk allergy. J. Exp. Med. 2004; 199: 1679–1688. https://doi.org/10.1084/jem.20032121
Salvatore S, Vandenplas Y. Gastroesophageal reflux and cow milk allergy: is there a link? Pediatrics. 2002;110(5):972-84. https://doi.org/10.1542/peds.110.5.972
Daza W, Dadán S, Rojas AM. Alergia alimentaria en la infancia. Programa de Educación Continuada (Precop), Soc Col de Pediat. 2014;13(3):49-58.
Magazzù G, Scoglio R. Gastrointestinal manifestations of cow’s milk allergy.Ann Allergy Asthma Immunol. 2002;89(6 Suppl 1):65-8. https://doi.org/10.1016/S1081-1206(10)62126-6
Sicherer SH. Determinants of systemic manifestations of food allergy. J Allergy Clin Immunol. 2000;106(5 Suppl):S251-7. https://doi.org/10.1067/mai.2000.110158
Walker-Smith J. Cow’s milk allergy: a new understanding from immunology. Ann Allergy Asthma Immunol. 2003;90(6 Suppl 3):81-3. https://doi.org/10.1016/S1081-1206(10)61666-3
Huang J, Walker WA. Food allergic enteropathy. En: Huang J, Walker WA. Review of pediatric gastroenterology disease and nutrition. Hamilton: BC Decker Inc; 2005. p. 145-146.
Nosan G, Jakic M, Jager M, Paro-Panjan D. Prognostic accuracy of clinical signs and diagnostic tests in cow’s milk allergy in newborns. Pediatr Neonatol. 2017;58(5):449-454. https://doi.org/10.1016/j.pedneo.2016.09.009
Bahna SL. Clinical expressions of food allergy. Ann Allergy Asthma Immunol. 2003;90(6 Suppl 3):41-4. https://doi.org/10.1016/S1081-1206(10)61659-6
Fiocchi A, Schünemann HJ, Brozek J, Restani P, Beyer K, Troncone R, et al. Diagnosis and Rationale for Action Against Cow’s Milk Allergy (DRACMA): a summary report. J Allergy Clin Immunol. 2010;126(6):1119-28.e12. https://doi.org/10.1016/j.jaci.2010.10.011
Kelly E, DunnGalvin G, Murphy BP, O’B Hourihane J. Formula supplementation remains a risk for cow’s milk allergy in breast-fed infants. Pediatr Allergy Immunol. 2019;30(8):810-816. https://doi.org/10.1111/pai.13108
Vanto T, Juntunen-Backman K, Kalimo K, Klemola T, Koivikko A, Koskinen P, et al. The patch test, skin prick test, and serum milk-specific IgE as diagnostic tools in cow’s milk allergy in infants. Allergy. 1999;54(8):837-42. https://doi.org/10.1034/j.1398-9995.1999.00134.x
Costa AJ, Sarinho ES, Motta ME, Gomes PN, de Oliveira de Melo SM, da Silva GA. Allergy to cow’s milk proteins: what contribution does hypersensitivity in skin tests have to this diagnosis? Pediatr Allergy Immunol. 2011;22(1 Pt 2):e133-8. https://doi.org/10.1111/j.1399-3038.2010.00988.x
García-Ara MC, Boyano-Martínez MT, Díaz-Pena JM, Martín-Muñoz MF, Martín-Esteban M. Cow’s milk-specific immunoglobulin E levels as predictors of clinical reactivity in the follow-up of the cow’s milk allergy infants. Clin Exp Allergy. 2004;34(6):866-70. https://doi.org/10.1111/j.1365-2222.2004.01976.x
Vandenplas Y, Koletzko S, Isolauri E, Hill D, Oranje AP, Brueton M, et al. Guidelines for the diagnosis and management of cow’s milk protein allergy in infants. Arch Dis Child. 2007;92(10):902-8. https://doi.org/10.1136/adc.2006.110999
Venter C, Pereira B, Voigt K, Grundy J, Clayton CB, Gant C, et al. Comparison of open and double-blind placebo-controlled food challenges in diagnosis of food hypersensitivity amongst children. J Hum Nutr Diet. 2007;20(6):565-79. https://doi.org/10.1111/j.1365-277X.2007.00828.x
Sampson HA. Utility of food-specific IgE concentrations in predicting symptomatic food allergy. J Allergy Clin Immunol. 2001;107(5):891-6. https://doi.org/10.1067/mai.2001.114708
Nowak-Wegrzyn A, Bloom KA, Sicherer SH, Shreffler WG, Noone S, Wanich N, et al. Tolerance to extensively heated milk in children with cow’s milk allergy. J Allergy Clin Immunol. 2008;122(2):342-7, 347.e1-2. https://doi.org/10.1016/j.jaci.2008.05.043
Lifschitz C, Szajewska H. Cow’s milk allergy: evidence-based diagnosis and management for the practitioner. Eur J Pediatr. 2015;174(2):141–150. https://doi.org/10.1007/s00431-014-2422-3
Cuomo B, Indirli GC, Bianchi A, Arasi S, Caimmi D, Dondi A, et al. Specific IgE and skin prick tests to diagnose allergy to fresh and baked cow’s milk according to age: a systematic review. Ital J Pediatr. 2017;43(1):93. https://doi.org/10.1186/s13052-017-0410-8
Čelakovská J, Krcmova I, Bukac J, Vaneckova J. Sensitivity and specificity of specific IgE, skin prick test and atopy patch test in examination of food allergy. 2016;28(2):238-247. http://dx.doi.org/10.1080/09540105.2016.1258548
Vandenplas Y, Dupont C, Eigenmann P, Host A, Kuitunen M, Ribes-Koninckx C, et al. A workshop report on the development of the Cow›s Milk-related Symptom Score awareness tool for young children. Acta Paediatr. 2015;104(4):334-9. https://doi.org/10.1111/apa.12902
Zeng Y, Zhang J, Dong G, Liu P, Xiao F, Li W, et al. Assessment of Cow›s milk-related symptom scores in early identification of cow›s milk protein allergy in Chinese infants. BMC Pediatr. 2019;19(1):191. https://doi.org/10.1186/s12887-019-1563-y
Vandenplas Y, Mukherjee R, Dupont C, Eigenmann P, Høst A, Kuitunen M, et al. Protocol for the validation of sensitivity and specificity of the Cow›s Milk-related Symptom Score (CoMiSS) against open food challenge in a single-blinded, prospective, multicentre trial in infants. BMJ Open. 2018;8(5):e019968. https://doi.org/10.1136/bmjopen-2017-019968
Xanthakos SA, Schwimmer JB, Melin-Aldana H, Rothenberg ME, Witte DP, Cohen MB. Prevalence and outcome of allergic colitis in healthy infants with rectal bleeding: a prospective cohort study. J Pediatr Gastroenterol Nutr. 2005;41(1):16-22. https://doi.org/10.1097/01.MPG.0000161039.96200.F1
Hill DJ, Heine RG, Cameron DJ, Catto-Smith AG, Chow CW, Francis DE, et al. Role of food protein intolerance in infants with persistent distress attributed to reflux esophagitis. J Pediatr. 2000;136(5):641-7. https://doi.org/10.1067/mpd.2000.104774
Jakobsson I, Lindberg T. Cow›s milk proteins cause infantile colic in breast-fed infants: a double-blind crossover study. Pediatrics. 1983;71(2):268-71.
Isolauri E, Tahvanainen A, Peltola T, Arvola T. Breast-feeding of allergic infants. J Pediatr. 1999;134(1):27-32. https://doi.org/10.1016/S0022-3476(99)70368-9
Saarinen UM, Kajosaari M. Breastfeeding as prophylaxis against atopic disease: prospective follow-up study until 17 years old. Lancet. 1995;346(8982):1065-9. https://doi.org/10.1016/S0140-6736(95)91742-X
American Academy of Pediatrics. Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106(2 Pt 1):346-9. https://doi.org/10.1542/peds.106.2.346
Giampietro PG, Kjellman NI, Oldaeus G, Wouters-Wesseling W, Businco L. Hypoallergenicity of an extensively hydrolyzed whey formula. Pediatr Allergy Immunol. 2001;12(2):83-6. https://doi.org/10.1034/j.1399-3038.2001.012002083.x
Vandenplas Y, De Greef E, Devreker T. Treatment of Cow›s Milk Protein Allergy. Pediatr Gastroenterol Hepatol Nutr. 2014;17(1):1–5. http://dx.doi.org/10.5223/pghn.2014.17.1.1
Isolauri E, Sütas Y, Mäkinen-Kiljunen S, Oja SS, Isosomppi R, Turjanmaa K. Efficacy and safety of hydrolyzed cow milk and amino acid-derived formulas in infants with cow milk allergy. J Pediatr. 1995;127(4):550-7. https://doi.org/10.1016/S0022-3476(95)70111-7
Cordero C, Prado F, Bravo P. Actualización en manejo de alergia a la proteína de leche de vaca: fórmulas lácteas disponibles y otros brebajes. 2018;89(3):310-317. https://doi.org/10.4067/S0370-41062018005000503
Halpern SR, Sellars WA, Johnson RB, Anderson DW, Saperstein S, Reisch JS. Development of childhood allergy in infants fed breast, soy, or cow milk. J Allergy Clin Immunol. 1973;51(3):139-51. https://doi.org/10.1016/0091-6749(73)90019-5
Bhatia J, Greer F; American Academy of Pediatrics Committee on Nutrition. Use of soy protein-based formulas in infant feeding. Pediatrics. 2008;121(5):1062-8. https://doi.org/10.1542/peds.2008-0564
Vandenplas Y, Castrellon PG, Rivas R, Gutiérrez CJ, Garcia LD, Jimenez JE, et al. Safety of soya-based infant formulas in children. Br J Nutr. 2014;111(8):1340-60. https://doi.org/10.1017/S0007114513003942
ESPGHAN Committee on Nutrition, Agostoni C, Axelsson I, Goulet O, Koletzko B, Michaelsen KF, et al. Soy protein infant formulae and follow-on formulae: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2006;42(4):352-61. https://doi.org/10.1097/01.mpg.0000189358.38427.cd
Høst A, Koletzko B, Dreborg S, Muraro A, Wahn U, Aggett P, et al. Dietary products used in infants for treatment and prevention of food allergy. Joint Statement of the European Society for Paediatric Allergology and Clinical Immunology (ESPACI) Committee on Hypoallergenic Formulas and the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Committee on Nutrition. Arch Dis Child. 1999;81(1):80-4. https://doi.org/10.1136/adc.81.1.80
Järvinen KM, Chatchatee P. Mammalian milk allergy: clinical suspicion, cross-reactivities and diagnosis. Curr Opin Allergy Clin Immunol. 2009;9(3):251-8. https://doi.org/10.1097/ACI.0b013e32832b3f33
Laitinen K, Kalliomäki M, Poussa T, Lagström H, Isolauri E. Evaluation of diet and growth in children with and without atopic eczema: follow-up study from birth to 4 years. Br J Nutr. 2005;94(4):565-74. https://doi.org/10.1079/BJN20051503
Nowak-Wegrzyn A, Czerkies L, Reyes K, Collins B, Heine RG. Confirmed Hypoallergenicity of a Novel Whey-Based Extensively Hydrolyzed Infant Formula Containing Two Human Milk Oligosaccharides. Nutrients. 2019;11(7). pii: E1447. https://doi.org/10.3390/nu11071447
Dupont C, Chouraqui JP, Linglart A, Bocquet A, Darmaun D, Feillet F, et al. Nutritional management of cow’s milk allergy in children: An update. Arch Pediatr. 2018;25(3):236-243. https://doi.org/10.1016/j.arcped.2018.01.007
Klemola T, Vanto T, Juntunen-Backman K, Kalimo K, Korpela R, Varjonen E. Allergy to soy formula and to extensively hydrolyzed whey formula in infants with cow’s milk allergy: a prospective, randomized study with a follow-up to the age of 2 years. J Pediatr. 2002;140(2):219-24. https://doi.org/10.1067/mpd.2002.121935
Nowak-Wegrzyn A, Sampson HA, Wood RA, Sicherer SH. Food protein-induced enterocolitis syndrome caused by solid food proteins. Pediatrics. 2003;111(4 Pt 1):829-35. https://doi.org/10.1542/peds.111.4.829
American College of Allergy, Asthma, & Immunology. Food allergy: a practice parameter. Ann Allergy Asthma Immunol. 2006;96(3 Suppl 2):S1-68.
Fergusson DM, Horwood LJ, Shannon FT. Early solid feeding and recurrent childhood eczema: a 10-year longitudinal study. Pediatrics. 1990;86(4):541-6.
Morgan J, Williams P, Norris F, Williams CM, Larkin M, Hampton S. Eczema and early solid feeding in preterm infants. Arch Dis Child. 2004;89(4):309–314. https://doi.org/10.1136/adc.2002.020065
Zutavern A, Brockow I, Schaaf B, Bolte G, von Berg A, Diez U, et al. Timing of solid food introduction in relation to atopic dermatitis and atopic sensitization: results from a prospective birth cohort study. Pediatrics. 2006;117(2):401-11. https://doi.org/10.1542/peds.2004-2521
Koplin JJ, Osborne NJ, Wake M, Martin PE, Gurrin LC, Robinson MN, et al. Can early introduction of egg prevent egg allergy in infants? A population-based study. J Allergy Clin Immunol. 2010;126(4):807-13. https://doi.org/10.1016/j.jaci.2010.07.028
Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. Nutr Res. 2011;31(1):61–75. https://doi.org/10.1016/j.jaci.2010.10.008
Osborn DA, Sinn JK. Prebiotics in infants for prevention of allergy. Cochrane Database Syst Rev. 2013;(3):CD006474. https://doi.org/10.1002/14651858.CD006474.pub3
Qamer S, Deshmukh M, Patole S. Probiotics for cow’s milk protein allergy: a systematic review of randomized controlled trials. Eur J Pediatr. 2019;178(8):1139-1149. https://doi.org/10.1007/s00431-019-03397-6
Kalliomäki M, Salminen S, Poussa T, Arvilommi H, Isolauri E. Probiotics and prevention of atopic disease: 4-year follow-up of a randomised placebo-controlled trial. Lancet. 2003;361(9372):1869-71. https://doi.org/10.1016/S0140-6736(03)13490-3
Arslanoglu S, Moro GE, Schmitt J, Tandoi L, Rizzardi S, Boehm G. Early dietary intervention with a mixture of prebiotic oligosaccharides reduces the incidence of allergic manifestations and infections during the first two years of life. J Nutr. 2008;138(6):1091-5. https://doi.org/10.1093/jn/138.6.1091
Bavaro SL, De Angelis E, Barni S, Pilolli R, Mori F, Novembre EM, et al. Modulation of Milk Allergenicity by Baking Milk in Foods: A Proteomic Investigation. Nutrients. 2019;11(7). pii: E1536. https://doi.org/10.3390/nu11071536
Chen M, Sutherland A, Birrueta G, Laubach S, Leonard S, Peters B, et al. Analysis of Allergen-Specific T Cell and IgE Reactivity to Different Preparations of Cow’s Milk-Containing Food Extracts. Cells. 2019;8(7):667. https://doi.org/10.3390/cells8070667
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |
















