Findings of upper gastrointestinal endoscopy in children with short stature
DOI:
https://doi.org/10.22516/25007440.494Keywords:
Growth failure, Children, EndoscopyAbstract
Introduction: The study of short stature of digestive origin in children shows no pre-established laboratory patterns. However, endoscopy of the digestive tract may be a useful tool for this purpose.
Objective: To report a series of cases of children with a diagnosis of short stature who underwent upper digestive tract endoscopy as part of their study.
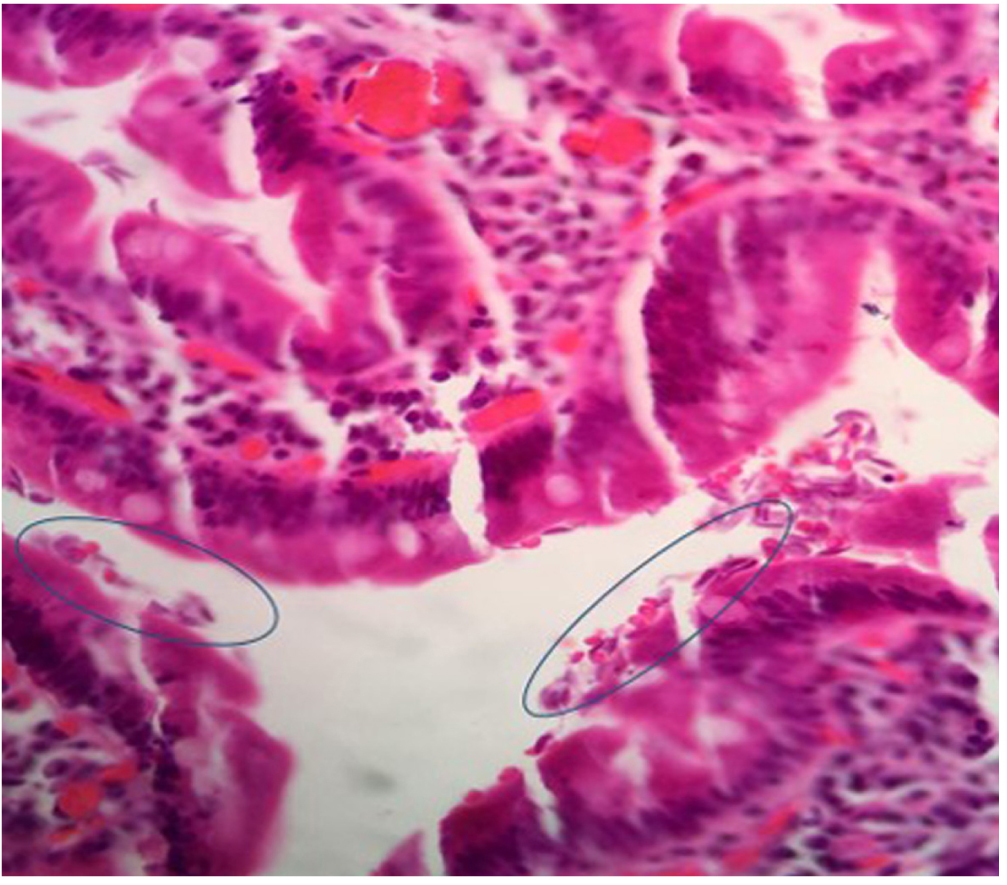
Case report: 15 children between the ages of 2 and 16 years were included; 53.3 % were girls. 26.7 % presented with malnutrition according to their body mass index and height-for-age, 66.7 % had short stature, and 33.3 % moderate short stature. Abdominal pain was reported in 53.3 % of the cases, and no weight gain in 46.7 %. Other symptoms were lack of appetite in 26.7 %, vomiting in 13.3 %, among others. Between 40 % and 93.4 % of the children presented macro and/or microscopic esophagitis, gastritis, and duodenitis. The most important microscopic findings were chronic duodenitis with giardiasis, duodenal ulcers, duodenal nodular lymphoid hyperplasia, Helicobacter pylori, and chronic eosinophilic duodenitis.
Conclusions: Although endoscopy of the digestive tract is a method barely used and not well described in the study of children with short stature, this case report describes organicity in 80 % of the children analyzed.
Downloads
References
Becker P, Carney LN, Corkins MR, Monczka J, Smith E, Smith SE, Spear BA, White JV; Academy of Nutrition and Dietetics; American Society for Parenteral and Enteral Nutrition. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). Nutr Clin Pract. 2015;30(1):147-61. https://doi.org/10.1177/0884533614557642
Larson-Nath C, Biank VF. Clinical Review of Failure to Thrive in Pediatric Patients. Pediatr Ann. 2016;45(2):e46-9. https://doi.org/10.3928/00904481-20160114-01
Homan GJ. Failure to Thrive: A Practical Guide. Am Fam Physician. 2016;94(4):295-9.
Bouma S. Diagnosing Pediatric Malnutrition. Nutr Clin Pract. 2017;32(1):52-67. https://doi.org/10.1177/0884533616671861
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660-7. https://doi.org/10.2471/blt.07.043497
Thomson M, Tringali A, Dumonceau JM, Tavares M, Tabbers MM, Furlano R, Spaander M, Hassan C, Tzvinikos C, Ijsselstijn H, Viala J, Dall’Oglio L, Benninga M, Orel R, Vandenplas Y, Keil R, Romano C, Brownstone E, Hlava Š, Gerner P, Dolak W, Landi R, Huber WD, Everett S, Vecsei A, Aabakken L, Amil-Dias J, Zambelli A. Paediatric Gastrointestinal Endoscopy: European Society for Paediatric Gastroenterology Hepatology and Nutrition and European Society of Gastrointestinal Endoscopy Guidelines. J Pediatr Gastroenterol Nutr. 2017;64(1):133-153. https://doi.org/10.1097/MPG.0000000000001408
Ihejirika OC, Nwaorgu OC, Ebirim CI, Nwokeji CM. Effects of intestinal parasitic infections on nutritional status of primary children in Imo State Nigeria. Pan Afr Med J. 2019;33:34. https://doi.org/10.11604/pamj.2019.33.34.17099
Lehto KM, Fan YM, Oikarinen S, Nurminen N, Hallamaa L, Juuti R, Mangani C, Maleta K, Hyöty H, Ashorn P. Presence of Giardia lamblia in stools of six- to 18-month old asymptomatic Malawians is associated with children’s growth failure. Acta Paediatr. 2019;108(10):1833-1840. https://doi.org/10.1111/apa.14832
Rivero MR, De Angelo C, Nuñez P, Salas M, Liang S. Intestinal parasitism and nutritional status among indigenous children from the Argentinian Atlantic Forest: Determinants of enteroparasites infections in minority populations. Acta Trop. 2018;187:248-256. https://doi.org/10.1016/j.actatropica.2018.08.015
Yentur Doni N, Yildiz Zeyrek F, Simsek Z, Gurses G, Sahin İ. Risk Factors and Relationship Between Intestinal Parasites and the Growth Retardation and Psychomotor Development Delays of Children in Şanlıurfa, Turkey. Turkiye Parazitol Derg. 2015;39(4):270-6. https://doi.org/10.5152/tpd.2015.3620
Heimer J, Staudacher O, Steiner F, Kayonga Y, Havugimana JM, Musemakweri A, Harms G, Gahutu JB, Mockenhaupt FP. Age-dependent decline and association with stunting of Giardia duodenalis infection among schoolchildren in rural Huye district, Rwanda. Acta Trop. 2015;145:17-22. https://doi.org/10.1016/j.actatropica.2015.01.011
Centeno-Lima S, Rosado-Marques V, Ferreira F, Rodrigues R, Indeque B, Camará I, De Sousa B, Aguiar P, Nunes B, Ferrinho P. Giardia Duodenalis e Desnutrição Crónica em Crianças Menores de Cinco Anos de uma Região Rural da Guiné-Bissau. Acta Med Port. 2013;26(6):721-4.
Al-Mekhlafi HM, Al-Maktari MT, Jani R, Ahmed A, Anuar TS, Moktar N, Mahdy MA, Lim YA, Mahmud R, Surin J. Burden of Giardia duodenalis infection and its adverse effects on growth of schoolchildren in rural Malaysia. PLoS Negl Trop Dis. 2013;7(10):e2516. https://doi.org/10.1371/journal.pntd.0002516
Verhagen LM, Incani RN, Franco CR, Ugarte A, Cadenas Y, Sierra Ruiz CI, Hermans PW, Hoek D, Campos Ponce M, de Waard JH, Pinelli E. High malnutrition rate in Venezuelan Yanomami compared to Warao Amerindians and Creoles: significant associations with intestinal parasites and anemia. PLoS One. 2013;8(10):e77581. https://doi.org/10.1371/journal.pone.0077581
Zonta ML, Oyhenart EE, Navone GT. Nutritional status, body composition, and intestinal parasitism among the Mbyá-Guaraní communities of Misiones, Argentina. Am J Hum Biol. 2010;22(2):193-200. https://doi.org/10.1002/ajhb.20977
Maia MM, Fausto MA, Vieira EL, Benetton ML, Carneiro M. Intestinal parasitic infection and associated risk factors, among children presenting at outpatient clinics in Manaus, Amazonas state, Brazil. Ann Trop Med Parasitol. 2009;103(7):583-91. https://doi.org/10.1179/000349809X12459740922417
Silva RR, da Silva CA, de Jesus Pereira CA, de Carvalho Nicolato RL, Negrão-Corrêa D, Lamounier JA, Carneiro M. Association between nutritional status, environmental and socio-economic factors and Giardia lamblia infections among children aged 6-71 months in Brazil. Trans R Soc Trop Med Hyg. 2009;103(5):512-9. https://doi.org/10.1016/j.trstmh.2008.10.019
Nematian J, Gholamrezanezhad A, Nematian E. Giardiasis and other intestinal parasitic infections in relation to anthropometric indicators of malnutrition: a large, population-based survey of schoolchildren in Tehran. Ann Trop Med Parasitol. 2008;102(3):209-14. https://doi.org/10.1179/136485908X267876
Muniz-Junqueira MI, Queiroz EF. Relationship between protein-energy malnutrition, vitamin A, and parasitoses in living in Brasília. Rev Soc Bras Med Trop. 2002;35(2):133-41. https://doi.org/10.1590/s0037-86822002000200002
Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet. 2002;359(9306):564-71. https://doi.org/10.1016/S0140-6736(02)07744-9
Chiu NC, Lin CY, Chi H, Yeung CY, Ting WH, Chan WT, Jiang CB, Li ST, Lin CH, Lee HC. Helicobacter pylori infection is not associated with failure to thrive: a case control study. Ther Clin Risk Manag. 2017;13:273-278. https://doi.org/10.2147/TCRM.S123148
Kocaoglu C, Ozel A, Cayci M, Solak ES. Effect of long-term Helicobacter pylori infection on growth of children: a cohort study. World J Pediatr. 2016;12(2):196-201. https://doi.org/10.1007/s12519-015-0021-7
Soylu OB, Ozturk Y. Helicobacter pylori infection: effect on malnutrition and growth failure in dyspeptic children. Eur J Pediatr. 2008;167(5):557-62. https://doi.org/10.1007/s00431-007-0552-6
Fialho AM, Braga AB, Queiroz DM, Rodrigues MN, Herbster ID, Braga LL. The association between Helicobacter pylori infection and height in children from an urban community in north-east Brazil. Ann Trop Paediatr. 2007;27(1):55-61. https://doi.org/10.1179/146532807X170510
Süoglu OD, Gökçe S, Saglam AT, Sökücü S, Saner G. Association of Helicobacter pylori infection with gastroduodenal disease, epidemiologic factors and iron-deficiency anemia in Turkish children undergoing endoscopy, and impact on growth. Pediatr Int. 2007;49(6):858-63. https://doi.org/10.1111/j.1442-200X.2007.02444.x
Chimonas MA, Baggett HC, Parkinson AJ, Muth PT, Dunaway E, Gessner BD. Asymptomatic Helicobacter pylori infection and iron deficiency are not associated with decreased growth among Alaska Native children aged 7-11 years. Helicobacter. 2006;11(3):159-67. https://doi.org/10.1111/j.1523-5378.2006.00395.x
Richter T, Richter T, List S, Müller DM, Deutscher J, Uhlig HH, Krumbiegel P, Herbarth O, Gutsmuths FJ, Kiess W. Five- to 7-year-old children with Helicobacter pylori infection are smaller than Helicobacter-negative children: a cross-sectional population-based study of 3,315 children. J Pediatr Gastroenterol Nutr. 2001;33(4):472-5. https://doi.org/10.1097/00005176-200110000-00010
Larson-Nath CM, Goday PS. Failure to Thrive: A Prospective Study in a Pediatric Gastroenterology Clinic. J Pediatr Gastroenterol Nutr. 2016;62(6):907-13. https://doi.org/10.1097/MPG.0000000000001099
El Mouzan MI, Assiri AM, Al Herbish AS, Al Sohaibani MO. Endoscopic duodenal biopsy in children. Saudi J Gastroenterol. 2006;12(1):31-3. https://doi.org/10.4103/1319-3767.27742
Stephenson LS, Latham MC, Ottesen EA. Malnutrition and parasitic helminth infections. Parasitology. 2000;121 Suppl:S23-38. https://doi.org/10.1017/s0031182000006491
Northrop-Clewes CA, Rousham EK, Mascie-Taylor CN, Lunn PG. Anthelmintic treatment of rural Bangladeshi children: effect on host physiology, growth, and biochemical status. Am J Clin Nutr. 2001;73(1):53-60. https://doi.org/10.1093/ajcn/73.1.53
Gendrel D, Treluyer JM, Richard-Lenoble D. Parasitic diarrhea in normal and malnourished children. Fundam Clin Pharmacol. 2003;17(2):189-97. https://doi.org/10.1046/j.1472-8206.2003.00169.x
Halliez MC, Buret AG. Extra-intestinal and long term consequences of Giardia duodenalis infections. World J Gastroenterol. 2013;19(47):8974-85. https://doi.org/10.3748/wjg.v19.i47.8974
Queiroz DM, Rocha AM, Crabtree JE. Unintended consequences of Helicobacter pylori infection in children in developing countries: iron deficiency, diarrhea, and growth retardation. Gut Microbes. 2013;4(6):494-504. https://doi.org/10.4161/gmic.26277
Owino V, Ahmed T, Freemark M, Kelly P, Loy A, Manary M, Loechl C. Environmental Enteric Dysfunction and Growth Failure/Stunting in Global Child Health. Pediatrics. 2016;138(6):e20160641. https://doi.org/10.1542/peds.2016-0641
Budge S, Parker AH, Hutchings PT, Garbutt C. Environmental enteric dysfunction and child stunting. Nutr Rev. 2019;77(4):240-253. https://doi.org/10.1093/nutrit/nuy068
Holguín L, Gallego-Yépes C, Toro Y, Díez-Zuluaga LS, Mopan J, Chinchilla C. Caracterización epidemiológica, clínica y diagnóstica de niños con gastroenteropatía eosinofílica. Estudio retrospectivo de tres instituciones de salud de alta complejidad. Rev Alerg Mex. 2018;65(2):148-159. https://doi.org/10.29262/ram.v65i2.354
Busoni VB, Lifschitz C, Christiansen S, G de Davila MT, Orsi M. Gastroenteropatía eosinofílica: una serie pediátrica. Arch Argent Pediatr. 2011;109(1):68-73. https://doi.org/10.1590/S0325-00752011000100019
Friesen CA, Kearns GL, Andre L, Neustrom M, Roberts CC, Abdel-Rahman SM. Clinical efficacy and pharmacokinetics of montelukast in dyspeptic children with duodenal eosinophilia. J Pediatr Gastroenterol Nutr. 2004;38(3):343-51. https://doi.org/10.1097/00005176-200403000-00021
Berezenko V, Bogdanova T, Krotevich M, Savenko Y, Vankhanova T. Morphological characteristics of chronic gastroduodenitis in adolescents with food hypersensitivity. Georgian Med News. 2018;(284):93-97.
Neilan NA, Dowling PJ, Taylor DL, Ryan P, Schurman JV, Friesen CA. Useful biomarkers in pediatric eosinophilic duodenitis and their existence: a case-control, single-blind, observational pilot study. J Pediatr Gastroenterol Nutr. 2010;50(4):377-84. https://doi.org/10.1097/MPG.0b013e3181c2c28a
Akbulut UE, Emeksiz HC, Kocak FG, Livaoglu A. Diagnostic yield of esophagogastroduodenoscopy in children with chronic abdominal pain. Arch Med Sci. 2018;14(1):74-80. https://doi.org/10.5114/aoms.2017.67675
Thakkar K, Chen L, Tessier ME, Gilger MA. Outcomes of children after esophagogastroduodenoscopy for chronic abdominal pain. Clin Gastroenterol Hepatol. 2014;12(6):963-9. https://doi.org/10.1016/j.cgh.2013.08.041
Sierra D, Wood M, Kolli S, Felipez LM. Pediatric Gastritis, Gastropathy, and Peptic Ulcer Disease. Pediatr Rev. 2018;39(11):542-549. https://doi.org/10.1542/pir.2017-0234
Blanco Rodríguez G, García Cárdenas E, Velasco Sánchez F, Bernal Redondo RM, López Facio K, Faure Fontenla A, Penchyna Grub J, Valencia Mayoral P. Hallazgos clínico-patológicos en niños con nódulos duodenales. Patologia (Mex). 2011;49(4):257-261.
Pernas Gómez P, Iglesias Meleiro J, García Rodríguez C, Martiñón Sánchez F. Dos observaciones de hiperplasia nodular linfoide intestinal asociadas a déficits inmunitarios. An Pediatr. 2011;75(1):72-3. https://doi.org/10.1016/j.anpedi.2010.12.008
Gonul CD, Bilge C, Gazi KA, Filiz K. Duodenal nodularity in children: a clinical and pathologic study of 17 cases. Indian J Pathol Microbiol. 2011;54(2):312-7. https://doi.org/10.4103/0377-4929.81611
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |
















