Neoplasia sólida pseudopapilar de páncreas: una serie de cinco casos y revisión de la literatura
DOI:
https://doi.org/10.22516/25007440.840Palabras clave:
Páncreas, sólido, pseudopapilar, neoplasia, tumorResumen
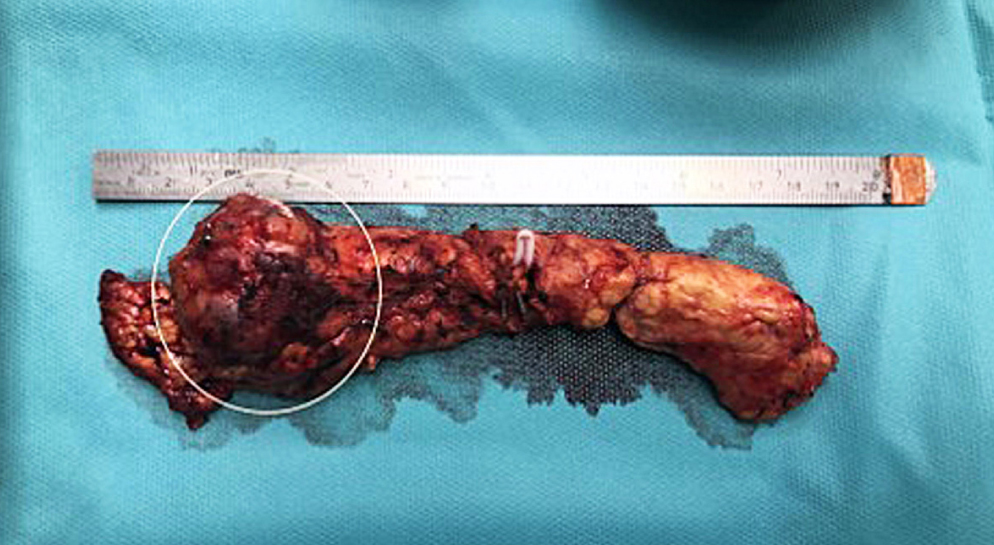
Introducción: las neoplasias sólidas pseudopapilares de páncreas representan alrededor del 3% de los tumores pancreáticos quísticos resecados. Se presentan con mayor frecuencia en mujeres jóvenes entre la segunda y tercera décadas de la vida. Es un tumor con poco potencial maligno que se ubica principalmente en la cola; sin embargo, puede encontrarse en cualquier localización anatómica pancreática.
Métodos: se presentan 5 casos de cuatro mujeres y un hombre, entre 16 y 36 años, que consultaron principalmente por dolor abdominal.
Resultados: cuatro pacientes fueron llevados a pancreatectomía distal sin esplenectomía por laparoscopia, y una paciente a pancreatoduodenectomía por laparotomía. Se logró extraer por completo y satisfactoriamente el tumor a los cinco pacientes. No se evidenció metástasis. Los tumores se localizaron en la cabeza (1), cuello (1) y predominantemente en cuerpo y cola (3). El reporte histopatológico posoperatorio confirmó el diagnóstico en los cinco casos, en la paciente más joven se había realizado una biopsia percutánea previa a la intervención quirúrgica.
Conclusiones: la resección quirúrgica completa del tumor con preservación del bazo es el tratamiento de elección en pacientes con neoplasia sólida pseudopapilar de páncreas.
Descargas
Referencias bibliográficas
Lanke G, Ali FS, Lee JH. Clinical update on the management of pseudopapillary tumor of pancreas. World J Gastrointest Endosc. 2018;10(9):145-155. https://doi.org/10.4253/wjge.v10.i9.145
Lichtenstein L. Papillary cystadenocarcinoma of pancreas: case report, with notes on classification of malignant cystic tumors of pancreas. American Journal of Cancer. 1934;21(3):542-553. https://doi.org/10.1158/ajc.1934.542
Frantz VK. Tumors of the pancreas. In: Frantz, VK (ed) Atlas of tumor pathology, vol. 1, no. 27. Washington, DC: US Armed Forces Institute of Pathology, 1959, p. 32-33.
Hamoudi AB, Misugi K, Grosfeld JL, Reiner CB. Papillary epithelial neoplasm of pancreas in a child. Report of a case with electron microscopy. Cancer; 1970;26(5):1126-1134. https://doi.org/10.1002/1097-0142(197011)26:5<1126::AID-CNCR2820260524>3.0.CO;2-K
Jena SS, Ray S, Das SAP, Mehta NN, Yadav A, Nundy S. Rare Pseudopapillary Neoplasm of the Pancreas: A 10-Year Experience. Surg Res Pract. 2021;2021:7377991. https://doi.org/10.1155/2021/7377991
Law JK, Ahmed A, Singh VK, Akshintala VS, Olson MT, Raman SP, et al. A systematic review of solid-pseudopapillary neoplasms: are these rare lesions? Pancreas. 2014;43(3):331-337. https://doi.org/10.1097/MPA.0000000000000061
Kloppel G, Basturk O, Klimstra DS, Ak L, Notohara K. "Solid pseudo-papillary neoplasm of the pancreas," in Tumors of Pancreas. In Who Classification of Tumors Editorial Board Eds: WHO Classification of Tumours. Digestive System Tumours, International Agency for Research on Cancer (IARC), A. J. Gill, D. S. Klimstra, A. K. Lam, and M. K. Washington, Eds., p. 340-342, 5th edition, 2019.
Valsangkar NP, Morales-Oyarvide V, Thayer SP, Ferrone CR, Wargo JA, Warshaw AL, et al. 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery. 2012;152(3 Suppl 1):S4-S12. https://doi.org/10.1016/j.surg.2012.05.033
Guo T, Wang L, Xie P, Zhang Z, Yu Y. Diagnosis and Surgical Treatment and Pathological Findings of Solid Pseudopapillary Tumor of the Pancreas: A Single-Institution Experience. Cancer Manag Res. 2020; 12:581-588. https://doi.org/10.2147/CMAR.S238527
Gurzu S, Bara T, Sincu M, Gabos S, Vlad DM, Bara Jr T, et al. Solid pseudopapillary neoplasm of pancreas: Two case reports. Medicine (Baltimore). 2019;98(29):e16455. https://doi.org/10.1097/MD.0000000000016455
La Rosa S, Bongiovanni M. Pancreatic Solid Pseudopapillary Neoplasm: Key Pathologic and Genetic Features [published online ahead of print, 2020 Jan 20]. Arch Pathol Lab Med. 2020;10.5858/arpa.2019-0473-RA. https://doi.org/10.5858/arpa.2019-0473-RA
Tiemann K, Heitling U, Kosmahl M, Klöppel G. Solid pseudopapillary neoplasms of the pancreas show an interruption of the Wnt-signaling pathway and express gene products of 11q. Mod Pathol. 2007;20(9):955-960. https://doi.org/10.1038/modpathol.3800902
Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg. 2005;200(6):965-972. https://doi.org/10.1016/j.jamcollsurg.2005.02.011
Tanaka Y, Kato K, Notohara K, Hojo H, Ijiri R, Miyake T, et al. Frequent beta-catenin mutation and cytoplasmic/nuclear accumulation in pancreatic solid-pseudopapillary neoplasm. Cancer Res. 2001;61(23):8401-8404
Hruban R. Lacobuzio-Donahue C. Pancreas. En: Kumar V, Abbas A, Aster J, editores. Patología Estructural y Funcional. 9° Edición. España, Elsevier Saunders. 2015. p. 883-896
Santini D, Poli F, Lega S. Solid-papillary tumors of the pancreas: histopathology. JOP 2006;7(1):131-136 [PMID: 16407635]
Jhala N, Siegal GP, Jhala D. Large, clear cytoplasmic vacuolation: an under-recognized cytologic clue to distinguish solid pseudopapillary neoplasms of the pancreas from pancreatic endocrine neoplasms on fine-needle aspiration. Cancer. 2008;114(4):249-254. https://doi.org/10.1002/cncr.23595
Meriaden Z, Shi C, Edil BH, Ellison T, Wolfgang CL, Cornish TC, et al. Hyaline globules in neuroendocrine and solid- pseudopapillary neoplasms of the pancreas: a clue to the diagnosis. Am J Surg Pathol. 2011;35(7):981-988. https://doi.org/10.1097/PAS.0b013e31821a9a14
Singh P, Kumar P, Rohilla M, Gupta P, Gupta N, Dey P, et al. Fine needle aspiration cytology with the aid of immunocytochemistry on cell-block confirms the diagnosis of solid pseudopapillary neoplasm of the pancreas [published online ahead of print, 2020 Apr 22]. Cytopathology. 2020;10.1111/cyt.12838. https://doi.org/10.1111/cyt.12838
Dinarvand P, Lai J. Solid Pseudopapillary Neoplasm of the Pancreas: A Rare Entity with Unique Features. Arch Pathol Lab Med. 2017;141(7):990-995. https://doi.org/10.5858/arpa.2016-0322-RS
Tafur A, Suarez D. Tumor de Frantz: el tumor de las mujeres jóvenes. Correlación radiologico-patologica de dos casos en tomografía. Revisión de la literatura. Rev Med. 2017;25(1):70-77. https://doi.org/10.18359/rmed.2922
Chung EM, Travis MD, Conran RM. Pancreatic tumors in children: radiologic-pathologic correlation. Radiographics. 2006;26(4):1211-1238. https://doi.org/10.1148/rg.264065012
Escobar MA, Bond BJ, Schopp J. Solid pseudopapillary tumour (Frantz's tumour) of the pancreas in childhood. BMJ Case Rep. 2014;2014: bcr2013200889. https://doi.org/10.1136/bcr-2013-200889
Shi S, Zhou Y, Hu C. Clinical manifestations and multi-slice computed tomography characteristics of solid pseudopapillary neoplasms of the pancreas between males and females. BMC Med Imaging. 2019;19(1):87. https://doi.org/10.1186/s12880-019-0390-9
Liu M, Liu J, Hu Q, Xu W, Liu W, Zhang Z, et al. Management of solid pseudopapillary neoplasms of pancreas: A single center experience of 243 consecutive patients. Pancreatology. 2019;19(5):681-685. https://doi.org/10.1016/j.pan.2019.07.001
Cai Y, Ran X, Xie S, Wang X, Peng B, Mai G, et al. Surgical Management and Long-Term Follow-Up of Solid Pseudopapillary Tumor of Pancreas: A Large Series from a Single Institution. J Gastrointest Surg. 2014;18(5):935-940. https://doi.org/10.1007/s11605-014-2476-6
Tang CW, Feng WM, Bao Y, Fei MY, Tao YL. Spleen-preserving distal pancreatectomy or distal pancreatectomy with splenectomy?: Perioperative and patient-reported outcome analysis. J Clin Gastroenterol. 2014;48(7):e62-6. https://doi.org/10.1097/MCG.0000000000000021
Shoup M, Brennan MF, McWhite K, Leung DHY, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002;137(2):164-168. https://doi.org/10.1001/archsurg.137.2.164
White SA, Sutton CD, Berry DP, Dennison AR. Value of splenic preservation during distal pancreatectomy for chronic pancreatitis. Br J Surg. 2000;87(1):124. https://doi.org/10.1046/j.1365-2168.2000.01329-7.
Kashuk JL, Moore EE, Johnson JL, Biffl WL, Burlew CC, Barnett C, et al. Progressive postinjury thrombocytosis is associated with thromboembolic complications. Surgery. 2010;148(4):667-674; discussion 674-675. https://doi.org/10.1016/j.surg.2010.07.013
Li BQ, Qiao YX, Li J, Yang WQ, Guo JC. Preservation or Ligation of Splenic Vessels During Spleen-Preserving Distal Pancreatectomy: A Meta-Analysis. J Invest Surg. 2019;32(7):654-669. https://doi.org/10.1080/08941939.2018.1449918
Matsushima H, Kuroki T, Adachi T, Kitasato A, Hirabaru M, Hidaka M, et al. Laparoscopic spleen-preserving distal pancreatectomy with and without splenic vessel preservation: The role of the Warshaw procedure. Pancreatology. 2014;14(6):530-535. https://doi.org/10.1016/j.pan.2014.09.007
Zhou ZQ, Kim SC, Song KB, Park KM, Lee JH, Lee YJ. Laparoscopic spleen-preserving distal pancreatectomy: comparative study of spleen preservation with splenic vessel resection and splenic vessel preservation. World J Surg. 2014;38(11):2973-2979. https://doi.org/10.1007/s00268-014-2671-3
Tsiouris A, Cogan CM, Velanovich V. Distal pancreatectomy with or without splenectomy: Comparison of postoperative outcomes and surrogates of splenic function. HPB (Oxford). 2011;13(10):738-744. https://doi.org/10.1111/j.1477-2574.2011.00369.x
Kang CM, Choi SH, Hwang HK, Lee WJ, Chi HS. Minimally invasive (laparoscopic and robot-assisted) approach for solid pseudopapillary tumor of the distal pancreas: A single-center experience. J Hepatobiliary Pancreat Sci. 2011;18(1):87-93. https://doi.org/10.1007/s00534-010-0316-y
Zhang RC, Yan JF, Xu XW, Chen K, Ajoodhea H, Mou YP. Laparoscopic vs open distal pancreatectomy for solid pseudopapillary tumor of the pancreas. World J Gastroenterol. 2013;19(37):6272-6277. https://doi.org/10.3748/wjg.v19.i37.6272
Namgoong JM, Kim DY, Kim SC, Kim SC, Hwang JH, Song KB. Laparoscopic distal pancreatectomy to treat solid pseudopapillary tumors in children: Transition from open to laparoscopic approaches in suitable cases. Pediatr Surg Int. 2014;30(3):259-266. https://doi.org/10.1007/s00383-014-3471-4
Stewart CL, Meguid C, Chapman B, Schulick R, Edil BH. Evolving Trends Towards Minimally Invasive Surgery for Solid-Pseudopapillary Neoplasms. Ann Surg Oncol. 2016;23(13):4165-4168. https://doi.org/10.1245/s10434-016-5491-x
Tan HL, Tan EK, Teo JY, Kam JH, Lee SY, Cheow PC, et al. Outcome of minimally-invasive versus open pancreatectomies for solid pseudopapillary neoplasms of the pancreas: A 2:1 matched case-control study. Ann Hepato-Biliary-Pancreatic Surg. 2019;23(3):252-257. https://doi.org/10.14701/ahbps.2019.23.3.252
You L, Yang F, Fu DL. Prediction of malignancy and adverse outcome of solid pseudopapillary tumor of the pancreas. World J Gastrointest Oncol. 2018;10(7):184-193. https://doi.org/10.4251/wjgo.v10.i7.184
Park JK, Cho EJ, Ryu JK, Kim YT, Yoon YB. Natural history and malignant risk factors of solid Pseudopapillary tumors of the pancreas. Postgrad Med. 2013;125(2):92-99. https://doi.org/10.3810/pgm.2013.03.2634
Zou C, Yang F, Wu W, Fu D. Ki-67 and malignancy in solid pseudopapillary tumor of the pancreas: A systematic review and meta-analysis. Pancreatology. 2020;20(4):683-685. https://doi.org/10.1016/j.pan.2020.03.015
Tang LH, Aydin H, Brennan MF, Klimstra DS. Clinically aggressive solid pseudopapillary tumors of the pancreas: A report of two cases with components of undifferentiated carcinoma and a comparative clinicopathologic analysis of 34 conventional cases. Am J Surg Pathol. 2005;29(4):512-519. https://doi.org/10.1097/01.pas.0000155159.28530.88
Amato E, Mafficini A, Hirabayashi K, Lawlor RT, Fassan M, Vicentini C, et al. Molecular alterations associated with metastases of solid pseudopapillary neoplasms of the pancreas. J Pathol. 2019;247(1):123-134. https://doi.org/10.1002/path.5180
Yepuri N, Naous R, Meier AH, Cooney RN, Kittur D, Are C, et al. A systematic review and meta-analysis of predictors of recurrence in patients with Solid Pseudopapillary Tumors of the Pancreas. HPB (Oxford). 2020;22(1):12-19. https://doi.org/10.1016/j.hpb.2019.06.005
Gao H, Gao Y, Yin L, Wang G, Wei J, Jiang K, et al. Risk factors of the recurrences of pancreatic solid pseudopapillary tumors: A systematic review and meta-analysis. J Cancer. 2018;9(11):1905-1914. https://doi.org/10.7150/jca.24491
Inzani F, Petrone G, Rindi G. The New World Health Organization Classification for Pancreatic Neuroendocrine Neoplasia. Endocrinol Metab Clin North Am. 2018;47(3):463-470. https://doi.org/10.1016/j.ecl.2018.04.008
Yang F, Jin C, Long J, Yu XJ, Xu J, Di Y, et al. Solid pseudopapillary tumor of the pancreas: a case series of 26 consecutive patients. Am J Surg. 2009;198(2):210-215. https://doi.org/10.1016/j.amjsurg.2008.07.062
Kim EK, Jang M, Park M, Kim H. LEF1, TFE3, and AR are putative diagnostic markers of solid pseudopapillary neoplasms. Oncotarget. 2017;8(55):93404-93413. https://doi.org/10.18632/oncotarget.21854
Karsenti D, Caillol F, Chaput U, Perrot B, Koch S, Vuitton L, et al. Safety of Endoscopic Ultrasound-Guided Fine-Needle Aspiration for Pancreatic Solid Pseudopapillary Neoplasm before Surgical Resection: A European Multicenter Registry-Based Study on 149 Patients. Pancreas. 2020;49(1):34-38. https://doi.org/10.1097/MPA.0000000000001460
Descargas
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |
















