Quality of Life and Sexual Function in Women with Liver Cirrhosis in Colombia
DOI:
https://doi.org/10.22516/25007440.1063Keywords:
Quality of life, Women, Cirrhosis, Sexual health, Psychological sexual dysfunctionsAbstract
Introduction: The female sex has been systematically identified as one of the predictors of poor quality of life in patients with cirrhosis. However, the relationship between quality of life and sexual function in women with cirrhosis has not been widely studied.
Aim: To determine the relationship between quality of life and sexual function in women with cirrhosis.
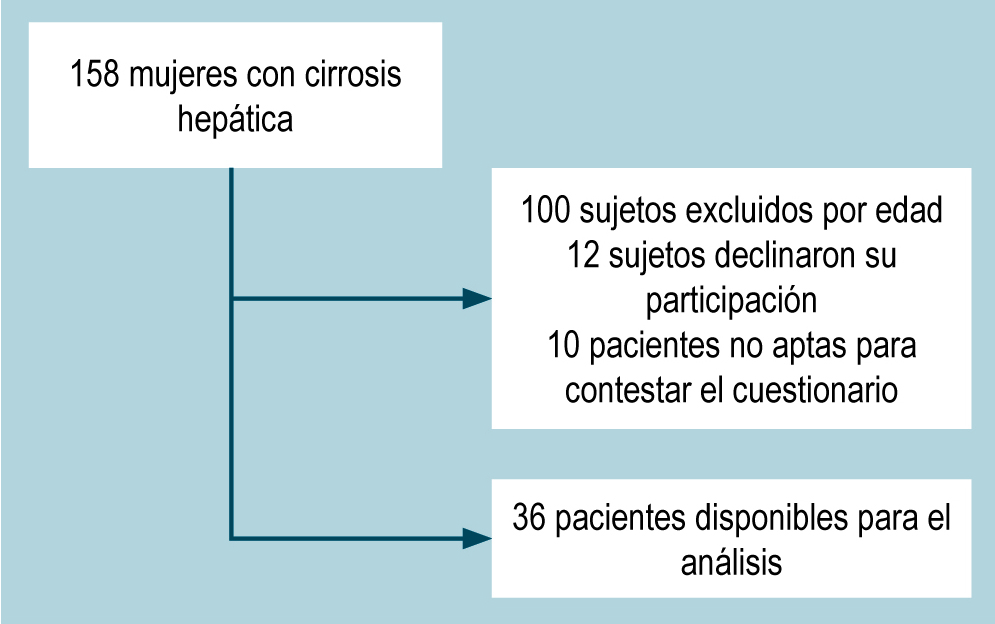
Materials and methods: A cross-sectional observational study. Female patients aged 18 to 69 years were included. The SF-36-V2 survey assessed health-related quality of life, and the IFSF-6 evaluated sexual function. Univariate and multivariate linear regression was used to identify the relationship between quality of life and sexual function. Statistical significance was set at a p-value < 0.05.
Results: 36 patients were available for analysis. The average age was 61 years. In the SF36-V2 survey, the physical component summary mean was 58, and the mental component summary mean was 56. The IFSF-6 had an average of 10. Sexual dysfunction occurred in 80% of patients. The IFSF-6 score was positively related to health-related quality of life. Factors associated with the deterioration of sexual function were age and menopause. The Child-Pugh score and body mass index were the main determinants of health-related quality of life.
Conclusions: Sexual function could be a determinant of quality of life in women with cirrhosis.
Downloads
References
The WHOQOL Group. The Development of the World Health Organization Quality of Life Assessment Instrument (the WHOQOL). En: Orley J, Kuyken W (editores). Quality of Life Assessment: International Perspectives. Springer Berlin Heidelberg; 1994. p. 41-57. https://doi.org/10.1007/978-3-642-79123-9_4
Urzúa MA. Calidad de vida relacionada con la salud: elementos conceptuales. Rev Med Chil. 2010;138(3):358-65. https://doi.org/10.4067/S0034-98872010000300017
Loria A, Escheik C, Gerber NL, Younossi ZM. Quality of life in cirrhosis. Curr Gastroenterol Rep. 2013;15(1):301. https://doi.org/10.1007/s11894-012-0301-5
North CS, Devereaux R, Pollio DE, Hong BA, Jain MK. Patient perspectives on hepatitis C and its treatment. Eur J Gastroenterol Hepatol. 2014;26(1):74-81. https://doi.org/10.1097/MEG.0b013e32836382b5
Orr JG, Homer T, Ternent L, Newton J, McNeil CJ, Hudson M, et al. Health related quality of life in people with advanced chronic liver disease. J Hepatol. 2014;61(5):1158-65. https://doi.org/10.1016/j.jhep.2014.06.034
Afendy A, Kallman JB, Stepanova M, Younoszai Z, Aquino RD, Bianchi G, et al. Predictors of health-related quality of life in patients with chronic liver disease. Aliment Pharmacol Ther. 2009;30(5):469-76. https://doi.org/10.1111/j.1365-2036.2009.04061.x
Mejía G, Gómez MT, Moreno-Medina K. Evaluación de la calidad de vida relacionada con la salud pre y post trasplante hepático, en pacientes de un hospital de alta complejidad. Psychologia. 2019;13(1):65-72. https://doi.org/10.21500/19002386.3721
Hamer J, McDonald R, Zhang L, Verma S, Leahey A, Ecclestone C, et al. Quality of life (QOL) and symptom burden (SB) in patients with breast cancer. Support Care Cancer. 2017;25(2):409-19. https://doi.org/10.1007/s00520-016-3417-6
Amodio P, Salari L, Montagnese S, Schiff S, Neri D, Bianco T, et al. Hepatitis C virus infection and health-related quality of life. World J Gastroenterol. 2012;18(19):2295-9. https://doi.org/10.3748/wjg.v18.i19.2295
Neong SF, Billington EO, Congly SE. Sexual Dysfunction and Sex Hormone Abnormalities in Patients With Cirrhosis: Review of Pathogenesis and Management. Hepatology. 2019;69(6):2683-95. https://doi.org/10.1002/hep.30359
Blümel JE, Binfa EL, Cataldo AP, Carrasco VA, Izaguirre LH, Sarrá CS. Índice de función sexual femenina: un test para evaluar la sexualidad de la mujer. Rev Chil Obstet Ginecol. 2004;69(2):118-25. https://doi.org/10.4067/S0717-75262004000200006
Faubion SS, Rullo JE. Sexual dysfunction in women: A practical approach. Am Fam Physician. 2015;92(4):281-8.
Fliegner M, Richter-Appelt H, Krupp K, Brunner F. Sexual Function and Socio-Sexual Difficulties in Women with Polycystic Ovary Syndrome (PCOS). Geburtshilfe Frauenheilkd. 2019;79(5):498-509. https://doi.org/10.1055/a-0828-7901
Pozzo MJ, Mociulsky J, Martinez ET, Senatore G, Farias JM, Sapetti A, et al. Diabetes and Quality of Life: Initial Approach to Depression, Physical Activity, and Sexual Dysfunction. Am J Ther. 2016;23(1):e159-71. https://doi.org/10.1097/01.mjt.0000433949.24277.19
Chang SR, Yang CF, Chen KH. Relationships between body image, sexual dysfunction, and health-related quality of life among middle-aged women: A cross-sectional study. Maturitas. 2019;126:45-50. https://doi.org/10.1016/j.maturitas.2019.04.218
Abozead SE, Abdelrahman G, Hassan A, Ibrahim WH. Sexual Dysfunction and Health Related Quality of Life among Female Patients Undergoing Hemodialysis. American Journal of Nursing Research. 2018;6(6):547-52. https://doi.org/10.12691/ajnr-6-6-24
Sun V, Grant M, Wendel CS, McMullen CK, Bulkley JE, Herrinton LJ, et al. Sexual Function and Health-Related Quality of Life in Long-Term Rectal Cancer Survivors. J Sex Med. 2016;13(7):1071-9. https://doi.org/10.1016/j.jsxm.2016.05.005
Yepes Barreto I, Lepesqueur Guillen L, Cadavid Asis S. Predictores de calidad de vida en pacientes con enfermedad hepática crónica en Colombia. Rev Col Gastroenterol. 2015;30(4):390-8. https://doi.org/10.22516/25007440.2
Yepes Barreto IDJ, Meza ZC, Contreras MNM. Calidad de vida en pacientes con hepatitis C crónica en Colombia. Rev Col Gastroenterol. 2017;32(2):112-9. https://doi.org/10.22516/25007440.139
Vilagut G, Ferrer M, Rajmil L, Rebollo P, Permanyer M, Quintana JM. et al. El Cuestionario de Salud SF-36 español: una década de experiencia y nuevos desarrollos. Gac Sanit. 2005;19(2):135-150. https://doi.org/10.1157/13074369
Alonso J, Ferrer M, Gandek B, Ware JE Jr, Aaronson NK, Mosconi P, et al. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13(2):283-298. https://doi.org/10.1023/B:QURE.0000018472.46236.05
Isidori AM, Pozza C, Esposito K, Giugliano D, Morano S, Vignozzi L, et al. Development and validation of a 6-item version of the female sexual function index (FSFI) as a diagnostic tool for female sexual dysfunction. J Sex Med. 2010;7(3):1139-46. https://doi.org/10.1111/j.1743-6109.2009.01635.x
Bae H, Park H. Sexual function, depression, and quality of life in patients with cervical cancer. Support Care Cancer. 2016;24(3):1277-83. https://doi.org/10.1007/s00520-015-2918-z
Aslan E, Beji NK, Gungor I, Kadioglu A, Dikencik BK. Prevalence and risk factors for low sexual function in women: a study of 1,009 women in an outpatient clinic of a university hospital in Istanbul. J Sex Med. 2008;5(9):2044-52. https://doi.org/10.1111/j.1743-6109.2008.00873.x
Nazarpour S, Simbar M, Ramezani Tehrani F, Alavi Majd H. Quality of life and sexual function in postmenopausal women. J Women Aging. 2018;30(4):299-309. https://doi.org/10.1080/08952841.2017.1395539
Kılıç M. Prevalence and risk factors of sexual dysfunction in healthy women in Turkey. Afr Health Sci. 2019;19(3):2623-33. https://doi.org/10.4314/ahs.v19i3.38
Elshimi E, Morad W, Mohamad NE, Shebl N, Waked I. Female Sexual Dysfunction Among Egyptian Patients with Chronic Hepatitis C. J Sex Med. 2014;11(3):768-75. https://doi.org/10.1111/jsm.12412
Bach N, Schaffner F, Kapelman B. Sexual behavior in women with nonalcoholic liver disease. Hepatology. 1989;9(5):698-703. https://doi.org/10.1002/hep.1840090507
Thiele M, Askgaard G, Timm HB, Hamberg O, Gluud LL. Predictors of health-related quality of life in outpatients with cirrhosis: results from a prospective cohort. Hepat Res Treat. 2013;2013:479639. https://doi.org/10.1155/2013/479639
Apple R, Samuels LR, Fonnesbeck C. Body mass index and health‐related quality of life. Obes Sci Pract. 2018;4(5):417-426. https://doi.org/10.1002/osp4.292
Poggiogalle E, Di Lazzaro l, Pinto A. Health-related quality of life and quality of sexual life in obese subjects. Int J Endocrinol. 2014;2014:847871. https://doi.org/10.1155/2014/847871
Morotti E, Battaglia B. Body mass index, stunkard figure rating scale, and sexuality in young italian women: a pilot study. J Sexual Med. 2013;10(4):1034-1043. https://doi.org/10.1111/jsm.12045
Vallejo-Medina P, Pérez-Durán C, Saavedra-Roa A. Translation, Adaptation, and Preliminary Validation of the Female Sexual Function Index into Spanish (Colombia). Arch Sex Behav. 2018;47(3):797-810. https://doi.org/10.1007/s10508-017-0976-7
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














