Beyond the Gut: Extraintestinal Manifestations of Inflammatory Bowel Disease in Children and Adolescents
DOI:
https://doi.org/10.22516/25007440.1168Keywords:
inflamatory bowel disease, arthritis, uveitis, erythema nodosum, hepatitis, pyoderma, pediatricsAbstract
Background: Extraintestinal manifestations (EIM) are common in children and adults and their presence is associated with a higher severity of inflammatory bowel disease (IBD). In pediatrics, studies are scarce in Latin America and do not exist in Colombia.
Objective: To describe the prevalence of EIM in children with IBD and the associated demographic, clinical, and biochemical characteristics.
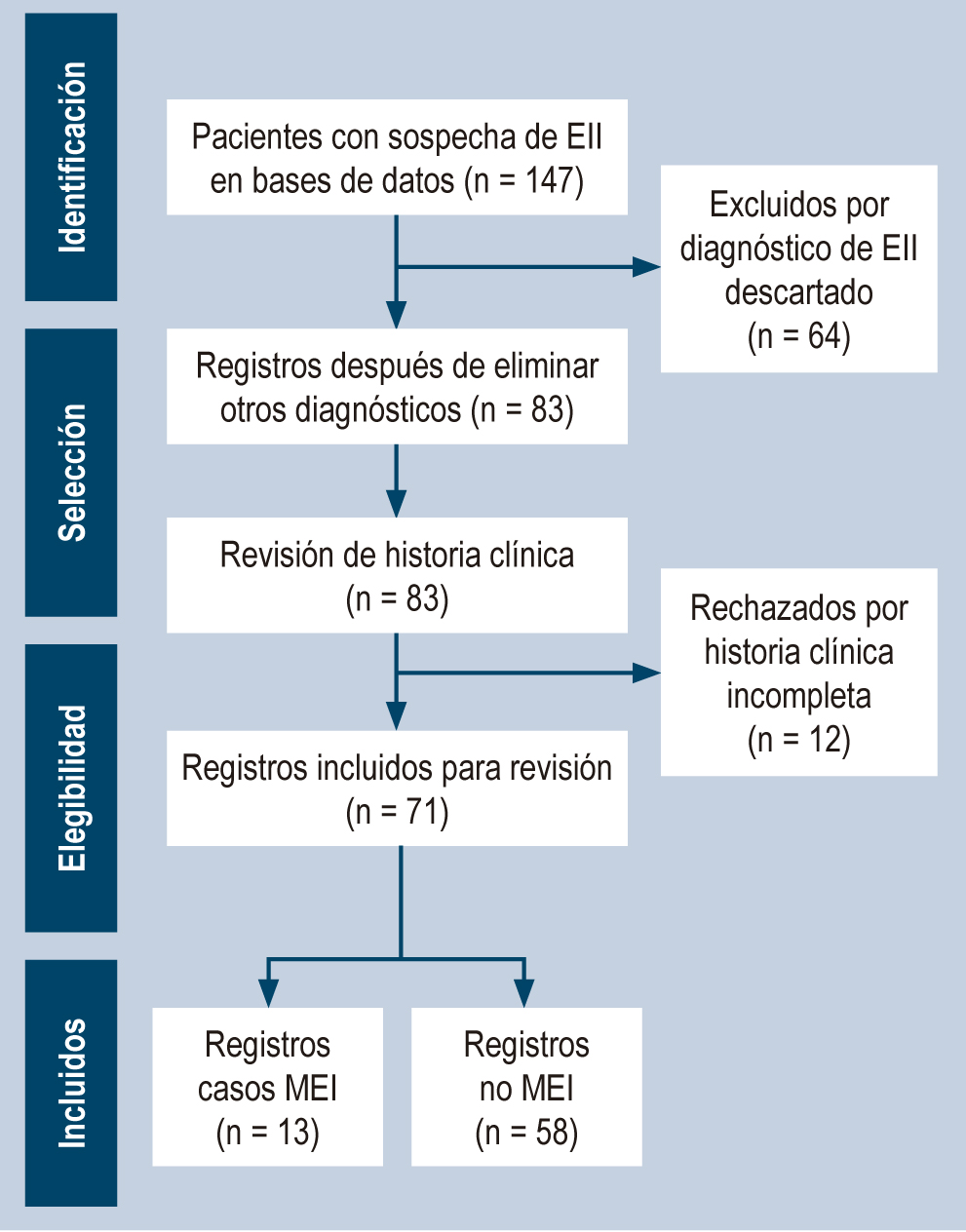
Methodology: Retrospective study of patients diagnosed with pediatric-onset IBD between 2007 and 2022 treated at an institution in Bogotá. A descriptive analysis was performed and in the groups with and without EIM clinical and biochemical variables were compared using Fisher’s exact test, Student’s T, and Mann-Whitney’s U.
Results: Of 71 confirmed cases, 45% had typical ulcerative colitis, 27% Crohn’s disease, 7% atypical ulcerative colitis, 1.4% colonic Crohn’s, and 20% unclassifiable IBD. Thirteen patients (18%) had at least one EIM, and mucocutaneous was the most frequent (58%). The time from symptoms onset to diagnosis was higher in the EIM group (13.2 years vs. 10.2 years; p = 0.02). Nocturnal diarrhea, hyporexia, and weight loss were more frequent in children with EIM. The EIM group showed lower hemoglobin levels, and higher globular sedimentation rate, and received biologics more frequently (38% vs. 23%, p = 0.2).
Conclusions: The frequency of MEI in this series is similar to that reported in the literature; its presence is associated with higher disease severity, higher frequency of biological use, and longer time IBD diagnosis.
Downloads
References
Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, De Ridder L, et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58(6):795-806. https://doi.org/10.1097/MPG.0000000000000239
Vera-Chamorro JF, Sanchez-Franco C, Vargas-Sandoval M, Mora-Quintero DV, Riveros-López JP, Sarmiento-Quintero F, et al. Consenso colombiano de la enfermedad inflamatoria intestinal pediátrica. Rev Colomb Gastroenterol. 2023;38(Supl 1):1-72. https://doi.org/10.22516/25007440.943
Sýkora J, Pomahačová R, Kreslová M, Cvalínová D, Štych P, Schwarz J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J Gastroenterol. 2018;24(25):2741-63. https://doi.org/10.3748/wjg.v24.i25.2741
Larrosa-Haro A, Abundis-Castro L, Contreras MB, Gallo MJ, Peña-Quintana L, Targa Ferreira CH, et al. Epidemiologic trend of pediatric inflammatory bowel disease in Latin America: The Latin American Society for Pediatric Gastroenterology, Hepatology and Nutrition (LASPGHAN) Working Group. Rev Gastroenterol Mex. 2021;86(4):328-34. https://doi.org/10.1016/j.rgmxen.2021.07.004
Rubalcava NS, Gadepalli SK. Inflammatory Bowel Disease in Children and Adolescents. Adv Pediatr. 2021;68:121-142. https://doi.org/10.1016/j.yapd.2021.05.005
Juliao-Baños F, Arrubla M, Osorio L, Camargo J, Londoño J, Cáceres C, et al. Characterization and prevalence of extraintestinal manifestations in a cohort of patients with inflammatory intestinal disease in Medellin, Colombia. Gastroenterol Hepatol. 2021;44(6):398-404. https://doi.org/10.1016/j.gastre.2020.07.015
Vavricka SR, Rogler G, Gantenbein C, Spoerri M, Vavricka MP, Navarini AA, et al. Chronological order of appearance of extraintestinal manifestations relative to the time of IBD diagnosis in the Swiss Inflammatory Bowel Disease Cohort. Inflamm Bowel Dis. 2015;21(8):1794-800. https://doi.org/10.1097/MIB.0000000000000429
Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21(8):1982-92. https://doi.org/10.1097/MIB.0000000000000392
Hedin CRH, Vavricka SR, Stagg AJ, Schoepfer A, Raine T, Puig L, et al. The Pathogenesis of Extraintestinal Manifestations: Implications for IBD Research, Diagnosis, and Therapy. J Crohn’s Colitis. 2019;13(5):541-54. https://doi.org/10.1093/ecco-jcc/jjy191
Kethu SR. Extraintestinal manifestations of inflammatory bowel diseases. J Clin Gastroenterol. 2006;40(6):467-75. https://doi.org/10.1097/00004836-200607000-00003
Harbord M, Annese V, Vavricka SR, Allez M, Acosta MB de, Boberg KM, et al. The first european evidence-based consensus on extra-intestinal manifestations in inflammatory bowel disease. J Crohn’s Colitis. 2016;10(3):239-54. https://doi.org/10.1093/ecco-jcc/jjv213
Rogler G, Singh A, Kavanaugh A, Rubin DT. Extraintestinal Manifestations of Inflammatory Bowel Disease: Current Concepts, Treatment, and Implications for Disease Management. Gastroenterology. 2021;161(4):1118-1132. https://doi.org/10.1053/j.gastro.2021.07.042
Duricova D, Leroyer A, Savoye G, Sarter H, Pariente B, Aoucheta D, et al. Extra-intestinal Manifestations at Diagnosis in Paediatric- and Elderly-onset Ulcerative Colitis are Associated With a More Severe Disease Outcome: A Population-based Study. J Crohns Colitis. 2017;11(11):1326-1334. https://doi.org/10.1093/ecco-jcc/jjx092
Duricova D, Sarter H, Savoye G, Leroyer A, Pariente B, Armengol-Debeir L, et al. Impact of Extra-Intestinal Manifestations at Diagnosis on Disease Outcome in Pediatric- and Elderly-Onset Crohn’s Disease: A French Population-Based Study. Inflamm Bowel Dis. 2019;25(2):394-402. https://doi.org/10.1093/ibd/izy254
Jansson S, Malham M, Paerregaard A, Jakobsen C, Wewer V. Extraintestinal Manifestations Are Associated With Disease Severity in Pediatric Onset Inflammatory Bowel Disease. J Pediatr Gastroenterol Nutr. 2020;71(1):40-5. https://doi.org/10.1097/MPG.0000000000002707
Jose FA, Garnett EA, Vittinghoff E, Ferry GD, Winter HS, Baldassana RN, et al. Development of extraintestinal manifestations in pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(1):63-8. https://doi.org/10.1002/ibd.20604
Nóbrega VG, Silva IN de N, Brito BS, Silva J, da SILVA MCM, Santana GO. The onset of clinical manifestations in inflammatory bowel disease patients. Arq Gastroenterol. 2018;55(3):290-5. https://doi.org/10.1590/s0004-2803.201800000-73
Gordon H, Burisch J, Ellul P, Karmiris K, Katsanos K, Allocca M, et al. ECCO Guidelines on Extraintestinal Manifestations in Inflammatory Bowel Disease. J Crohns Colitis. 2024;18(1):1-37. https://doi.org/10.1093/ecco-jcc/jjad108
Greuter T, Vavricka SR. Extraintestinal manifestations in inflammatory bowel disease-epidemiology, genetics, and pathogenesis. Expert Rev Gastroenterol Hepatol. 2019;13(4):307-17. https://doi.org/10.1080/17474124.2019.1574569
Herzog D, Fournier N, Buehr P, Rueger V, Koller R, Heyland K, et al. Age at disease onset of inflammatory bowel disease is associated with later extraintestinal manifestations and complications. Eur J Gastroenterol Hepatol. 2018;30(6):598-607. https://doi.org/10.1097/MEG.0000000000001072
Wiskin AE, Fleming BJ, Wootton SA, Beattie RM. Anaemia and iron deficiency in children with inflammatory bowel disease. J Crohn’s Colitis. 2012;6(6):687-91. https://doi.org/10.1016/j.crohns.2011.12.001
Jang HJ, Kang B, Choe BH. The difference in extraintestinal manifestations of inflammatory bowel disease for children and adults. Transl Pediatr. 2019;8(1):4-15. https://doi.org/10.21037/tp.2019.01.06
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Epidemiology. 2007;18(6):800-4. https://doi.org/10.1097/EDE.0b013e3181577654
Ministerio de Salud y Protección Social. Resolución 2465 de 2016, por la cual se adoptan los indicadores antropométricos, patrones de referencia y puntos de corte para la clasificación antropométrica del estado nutricional de niñas, niños y adolescentes menores de 18 años de edad, adultos de 18 a 64 años de edad y gestantes adultas y se dictan otras disposiciones [Internet]. Colombia: Minsalud; 2016 [consultado el 1 de junio de 2023]. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/resolucion-2465-2016.pdf
Rudwaleit M, Van Der Heijde D, Landewé R, Akkoc N, Brandt J, Chou CT, et al. The Assessment of SpondyloArthritis international Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis. 2011;70(1):25-31. https://doi.org/10.1136/ard.2010.133645
Burgos-Vargas R. The assessment of the spondyloarthritis international society concept and criteria for the classification of axial spondyloarthritis and peripheral spondyloarthritis: A critical appraisal for the pediatric rheumatologist. Pediatr Rheumatol Online J. 2012;10(1):14. https://doi.org/10.1186/1546-0096-10-14
Diaconescu S, Strat S, Balan GG, Anton C, Stefanescu G, Ioniuc I, et al. Dermatological manifestations in pediatric inflammatory bowel disease. Medicina (Kaunas). 2020;56(9):425. https://doi.org/10.3390/medicina56090425
Sridhar S, Maltz RM, Boyle B, Kim SC. Dermatological Manifestations in Pediatric Patients with Inflammatory Bowel Diseases on Anti-TNF Therapy. Inflamm Bowel Dis. 2018;24(9):2086-92. https://doi.org/10.1093/ibd/izy112
Antonelli E, Bassotti G, Tramontana M, Hansel K, Stingeni L, Ardizzone S, et al. Dermatological manifestations in inflammatory bowel diseases. J Clin Med. 2021;10(2):364. https://doi.org/10.3390/jcm10020364
Karreman MC, Karreman MC, Luime JJ, Hazes JMW, Weel AEAM, Weel AEAM. The prevalence and incidence of axial and peripheral spondyloarthritis in inflammatory bowel disease: A systematic review and meta-analysis. J Crohn’s Colitis. 2017;11(5):631-42. https://doi.org/10.1093/ecco-jcc/jjw199
Ali A, Schmidt M, Piskin D, Crowley E, Berard R. Epidemiology of Musculoskeletal Manifestations in Pediatric Inflammatory Bowel Disease: A Systematic Review. ACR Open Rheumatol. 2022;4(6):547-54. https://doi.org/10.1002/acr2.11431
Fritz J, Walia C, Elkadri A, Pipkorn R, Dunn RK, Sieracki R, et al. A Systematic Review of Micronutrient Deficiencies in Pediatric Inflammatory Bowel Disease. Inflamm Bowel Dis. 2019;25(3):445-59. https://doi.org/10.1093/ibd/izy271
Isa HM, Alahmed FA, Mohamed M, Mohamed A. The Prevalence of Iron and Vitamin D Deficiencies in Pediatric Patients With Inflammatory Bowel Disease in Bahrain. Cureus. 2023;15(4):e37074. https://doi.org/10.7759/cureus.37074
Orfei M, Gasparetto M, Hensel KO, Zellweger F, Heuschkel RB, Zilbauer M. Guidance on the interpretation of faecal calprotectin levels in children. PLoS One. 2021;16(2):e0246091. https://doi.org/10.1371/journal.pone.0246091
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |
















