Colestasis en el adulto: enfoque diagnóstico y terapéutico. Revisión de tema
DOI:
https://doi.org/10.22516/25007440.375Palabras clave:
Colestasis, intrahepática, extrahepáticaResumen
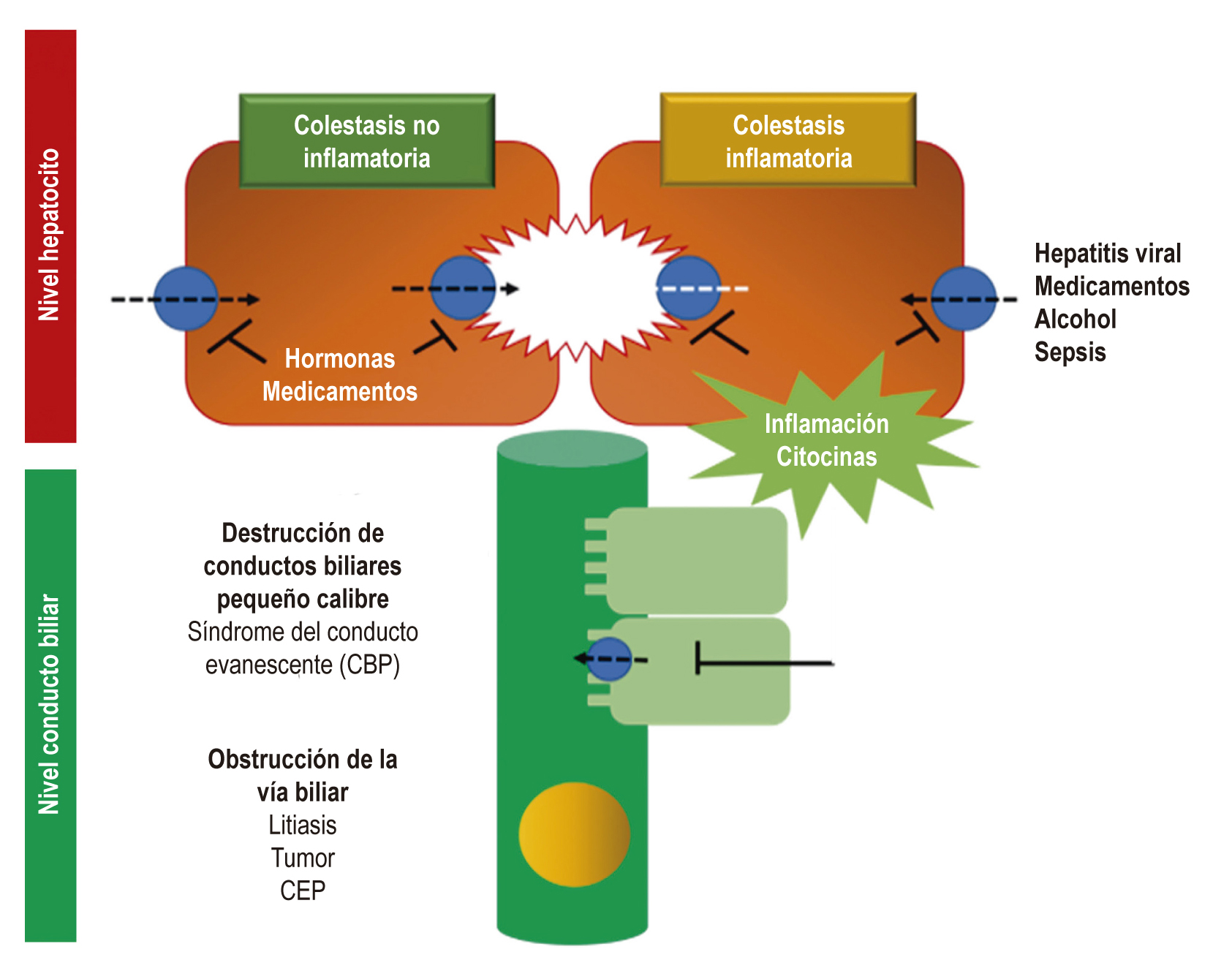
La colestasis es uno de los motivos de consulta más frecuentes en hepatología. Se genera por una alteración en la síntesis, la secreción o el flujo de la bilis, a través del tracto biliar. Esta se define por una elevación de enzimas como la fosfatasa alcalina (Alkaline Phosphatase, ALP) y la gamma-glutamil transferasa, y en estadios tardíos con la hiperbilirrubinemia, al igual que con otras manifestaciones clínicas, tales como el prurito y la ictericia.
El enfoque diagnóstico implica establecer el origen de dicha elevación, determinando si es intrahepática o extrahepática. Si es intrahepática, se debe esclarecer si proviene de los hepatocitos o de la vía biliar de pequeño y de gran calibre. El tratamiento dependerá de la etiología, por lo cual es importante un diagnóstico preciso. En esta revisión se presenta la fisiopatología y un enfoque diagnóstico y terapéutico.
Descargas
Referencias bibliográficas
McIntyre N. Cholestasis. En: Bircher J, Benhamou JP, McIntyre N, Rizzeto M, Rodés J. Oxford Textbook of Clinical Hepatology. Oxford: Oxford Medical Publications, 2a edición; 1999. p. 1574-9.
Heathcote EJ. Diagnosis and management of cholestatic liver disease. Clin Gastroenterol Hepatol. 2007;5(7):776-82. https://doi.org/10.1016/j.cgh.2007.05.008
Pérez Fernández T, López Serrano P, Tomás E, Gutiérrez ML, Lledó JL, Cacho G, et al. Diagnostic and therapeutic approach to cholestatic liver disease. Rev Esp Enferm Dig. 2004;96(1):60-73. https://doi.org/10.4321/S1130-01082004000100008
Trauner M, Meier PJ, Boyer JL. Molecular pathogenesis of cholestasis. N Engl J Med. 1998;339(17):1217-27. https://doi.org/10.1056/NEJM199810223391707
Zollner G, Trauner M. Mechanisms of cholestasis. Clin Liver Dis. 2008;12(1):1-26, vii. https://doi.org/10.1016/j.cld.2007.11.010
Elferink RO. Cholestasis. Gut. 2003;52 Suppl 2(Suppl 2):ii42–ii48. https://doi.org/10.1136/gut.52.suppl_2.ii42
Meier PJ. Molecular mechanisms of hepatic bile salt transport from sinusoidal blood into bile. Am J Physiol. 1995;269(6 Pt 1):G801-12. https://doi.org/10.1152/ajpgi.1995.269.6.G801
Hofmann AF, Hagey LR. Bile acids: chemistry, pathochemistry, biology, pathobiology, and therapeutics. Cell Mol Life Sci. 2008;65(16):2461-83. https://doi.org/10.1007/s00018-008-7568-6
Maillette de Buy Wenniger L, Beuers U. Bile salts and cholestasis. Dig Liver Dis. 2010;42(6):409-18. https://doi.org/10.1016/j.dld.2010.03.015
Siddique A, Kowdley KV. Approach to a patient with elevated serum alkaline phosphatase. Clin Liver Dis. 2012;16(2):199–229. https://doi.org/10.1016/j.cld.2012.03.012
Assis DN. Chronic Complications of Cholestasis: Evaluation and Management. Clin Liver Dis. 2018;22(3):533-544. https://doi.org/10.1016/j.cld.2018.03.014
Shen YM, Wu JF, Hsu HY, Ni YH, Chang MH, Liu YW, et al. Oral absorbable fat-soluble vitamin formulation in pediatric patients with cholestasis. J Pediatr Gastroenterol Nutr. 2012;55(5):587-91. https://doi.org/10.1097/MPG.0b013e31825c9732
Shneider BL, Magee JC, Bezerra JA, Harber B, Karpen SJ, Raghunathan T, et al. Efficacy of fat-soluble vitamin supplementation in infants with biliary atresia. Pediatrics. 2012;130(3):e607–e614. https://doi.org/10.1097/MPG.0b013e31825c9732
Craddock AL, Love MW, Daniel RW, et al. Expression and transport properties of the human ileal and renal sodium- dependent bile acid transporter. Am J Physiol 1998; 274 (1): 157–69. https://doi.org/10.1152/ajpgi.1998.274.1.G157
Kwo PY, Cohen SM, Lim JK. ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries. Am J Gastroenterol. 2017;112(1):18-35. https://doi.org/10.1038/ajg.2016.517
Schiele F, Henny J, Hitz J, Petitclerc C, Gueguen R, Siest G. Total bone and liver alkaline phosphatases in plasma: biological variations and reference limits. Clin Chem. 1983;29(4):634-41. https://doi.org/10.1093/clinchem/29.4.634
Stigbrand T. Present status and future trends of human alkaline phosphatases. Prog Clin Biol Res. 1984;166:3-14.
Sharma U, Pal D, Prasad R. Alkaline phosphatase: an overview. Indian J Clin Biochem. 2014;29(3):269–278. https://doi.org/10.1007/s12291-013-0408-y
Moussavian SN, Becker RC, Piepmeyer JL, Mezey E, Bozian RC. Serum gamma-glutamyl transpeptidase and chronic alcoholism. Influence of alcohol ingestion and liver disease. Dig Dis Sci. 1985;30(3):211-4. https://doi.org/10.1007/BF01347885
Lee DH, Silventoinen K, Hu G, Jacobs DR, Jousilahti P, Sundvall J, et al. Serum gamma-glutamyltransferase predicts non-fatal myocardial infarction and fatal coronary heart disease among 28,838 middle-aged men and women. Eur Heart J. 2006;27(18):2170-6. https://doi.org/10.1093/eurheartj/ehl086
Kim HW, Lee SH, Lee DH. Relationship of serum gamma-glutamyltransferase levels with pulmonary function and chronic obstructive pulmonary disease. Lung. 2014;192(5):719-27. https://doi.org/10.1007/s00408-014-9616-3
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis. J Hepatol. 2017;67(1):145-172. https://doi.org/10.1016/j.jhep.2017.03.022
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of cholestatic liver diseases. J Hepatol. 2009;51(2):237-67. https://doi.org/10.1016/j.jhep.2009.04.009
Patel A, Seetharam A. Primary Biliary Cholangitis: Disease Pathogenesis and Implications for Established and Novel Therapeutics. J Clin Exp Hepatol. 2016;6(4):311-318. https://doi.org/10.1016/j.jceh.2016.10.001
Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ, et al. Primary biliary cirrhosis. Hepatology. 2009;50(1):291-308. https://doi.org/10.1002/hep.22906
Jansen PL, Ghallab A, Vartak N, Reif R, Schaap FG, Hampe J, et al. The ascending pathophysiology of cholestatic liver disease. Hepatology. 2017;65(2):722-738. https://doi.org/10.1002/hep.28965
Williamson KD, Chapman RW. New Therapeutic Strategies for Primary Sclerosing Cholangitis. Semin Liver Dis. 2016;36(1):5-14. https://doi.org/10.1055/s-0035-1571274
Lindor KD, Kowdley KV, Harrison ME; American College of Gastroenterology. ACG Clinical Guideline: Primary Sclerosing Cholangitis. Am J Gastroenterol. 2015;110(5):646-59. https://doi.org/10.1038/ajg.2015.112
Smit WL, Culver EL, Chapman RW. New Thoughts on Immunoglobulin G4-Related Sclerosing Cholangitis. Clin Liver Dis. 2016;20(1):47-65. https://doi.org/10.1016/j.cld.2015.08.004
Nguyen KD, Sundaram V, Ayoub WS. Atypical causes of cholestasis. World J Gastroenterol. 2014;20(28):9418-26. http://dx.doi.org/10.3748/wjg.v20.i28.9418
Bhamidimarri KR, Schiff E. Drug-induced cholestasis. Clin Liver Dis. 2013;17(4):519-31, vii. https://doi.org/10.1016/j.cld.2013.07.015
Padda MS, Sanchez M, Akhtar AJ, Boyer JL. Drug-induced cholestasis. Hepatology. 2011;53(4):1377–1387. https://doi.org/10.1002/hep.24229
Floreani A, Gervasi MT. New Insights on Intrahepatic Cholestasis of Pregnancy. Clin Liver Dis. 2016;20(1):177-89. https://doi.org/10.1016/j.cld.2015.08.010
Lammert F, Marschall HU, Glantz A, Matern S. Intrahepatic cholestasis of pregnancy: molecular pathogenesis, diagnosis and management. J Hepatol. 2000;33(6):1012-21. https://doi.org/10.1016/S0168-8278(00)80139-7
Jacquemin E, De Vree JM, Cresteil D, Sokal EM, Sturm E, Dumont M, et al. The wide spectrum of multidrug resistance 3 deficiency: from neonatal cholestasis to cirrhosis of adulthood. Gastroenterology. 2001;120(6):1448-58. https://doi.org/10.1053/gast.2001.23984
Guglielmi FW, Regano N, Mazzuoli S, Fregnan S, Leogrande G, Guglielmi A, et al. Cholestasis induced by total parenteral nutrition. Clin Liver Dis. 2008;12(1):97-110, viii. https://doi.org/10.1016/j.cld.2007.11.004
Lauriti G, Zani A, Aufieri R, Cananzi M, Chiesa PL, Eaton S, et al. Incidence, prevention, and treatment of parenteral nutrition-associated cholestasis and intestinal failure-associated liver disease in infants and children: a systematic review. JPEN J Parenter Enteral Nutr. 2014;38(1):70-85. https://doi.org/10.1177/0148607113496280
Geier A, Fickert P, Trauner M. Mechanisms of disease: mechanisms and clinical implications of cholestasis in sepsis. Nat Clin Pract Gastroenterol Hepatol. 2006;3(10):574-85. https://doi.org/10.1038/ncpgasthep0602
Delemos AS, Friedman LS. Systemic causes of cholestasis. Clin Liver Dis. 2013;17(2):301-17. https://doi.org/10.1016/j.cld.2012.11.001
Strnad P, Tacke F, Koch A, Trautwein C. Liver - guardian, modifier and target of sepsis. Nat Rev Gastroenterol Hepatol. 2017;14(1):55-66. https://doi.org/10.1038/nrgastro.2016.168
Davit-Spraul A, Gonzáles E, Baussan C, Jacquemin E. The spectrum of liver diseases related to ABCB4 gene mutations: pathophysiology and clinical aspects. Semin Liver Dis. 2010;30(2):134-46. https://doi.org/10.1055/s-0030-1253223
Luketic VA, Shiffman ML. Benign recurrent intrahepatic cholestasis. Clin Liver Dis. 2004;8(1):133-49, vii. https://doi.org/10.1016/S1089-3261(03)00133-8
Elborn JS. Cystic fibrosis. Lancet. 2016;388(10059):2519-2531. https://doi.org/10.1016/S0140-6736(16)00576-6
Memon N, Weinberger BI, Hegyi T, Aleksunes LM. Inherited disorders of bilirubin clearance. Pediatr Res. 2016;79(3):378-86. https://doi.org/10.1038/pr.2015.247
Marzorati S, Invernizzi P, Lleo A. Making Sense of Autoantibodies in Cholestatic Liver Diseases. Clin Liver Dis. 2016;20(1):33-46. https://doi.org/10.1016/j.cld.2015.08.003
Shea JA, Berlin JA, Escarce JJ, Clarke JR, Kinosian BP, Cabana MD, et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med. 1994;154(22):2573-81. https://doi.org/10.1001/archinte.1994.00420220069008
Balci NC, Befeler AS, Leiva P, Pilgram TK, Havlioglu N. Imaging of liver disease: comparison between quadruple-phase multidetector computed tomography and magnetic resonance imaging. J Gastroenterol Hepatol. 2008;23(10):1520-7. https://doi.org/10.1111/j.1440-1746.2008.05434.x
Samant H, Manatsathit W, Dies D, Shokouh-Amiri H, Zibari G, Boktor M, et al. Cholestatic liver diseases: An era of emerging therapies. World J Clin Cases. 2019;7(13):1571–1581. https://doi.org/10.12998/wjcc.v7.i13.1571
Arab JP, Cabrera D, Arrese M. Bile Acids in Cholestasis and its Treatment. Ann Hepatol. 2017;16(Suppl. 1: s3-105.):s53-s57. https://doi.org/10.5604/01.3001.0010.5497
Beuers U, Trauner M, Jansen P, Poupon R. New paradigms in the treatment of hepatic cholestasis: from UDCA to FXR, PXR and beyond. J Hepatol. 2015;62(1 Suppl):S25-37. https://doi.org/10.1016/j.jhep.2015.02.023
Chazouillères O. Novel Aspects in the Management of Cholestatic Liver Diseases. Dig Dis. 2016;34(4):340-6. https://doi.org/10.1159/000444544
Czul F, Levy C. Novel Therapies on Primary Biliary Cirrhosis. Clin Liver Dis. 2016;20(1):113-30. https://doi.org/10.1016/j.cld.2015.08.006
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |
















