Nutrición en pancreatitis aguda: nuevos conceptos para un viejo problema
DOI:
https://doi.org/10.22516/25007440.447Palabras clave:
nutrición, reposo pancreático, sonda nasogástrica, sonda nasoyeyunalResumen
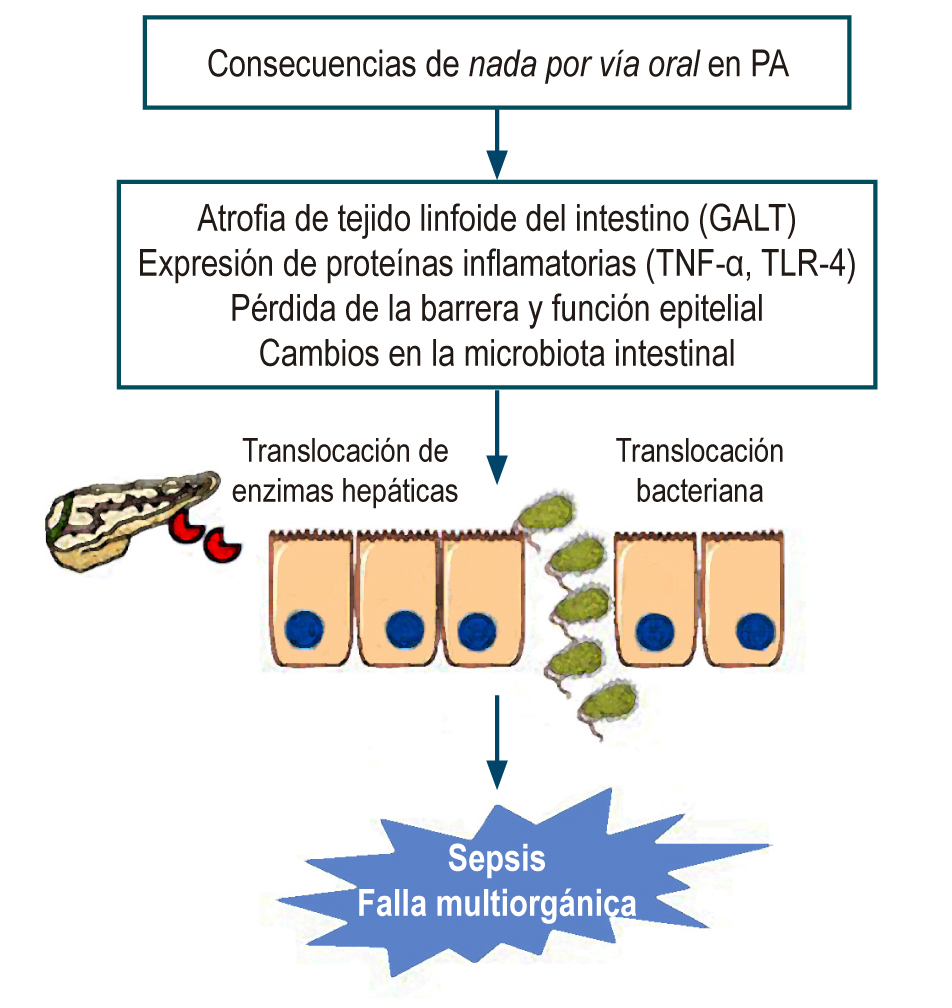
El manejo de la nutrición en pancreatitis aguda ha sido cuestión de debate. Durante muchos años el concepto de reposo pancreático fue generalizado y aceptado en el manejo de la pancreatitis aguda; actualmente se conoce que la nutrición temprana permite mantener la integridad de la barrera intestinal, que previene la aparición de complicaciones infeccionas y se asocia con una menor estancia hospitalaria, menos complicaciones y un mejor pronóstico. En esta revisión se discuten las principales ventajas de la nutrición temprana en pancreatitis aguda, la seguridad de la misma y la vía de administración.
Descargas
Referencias bibliográficas
Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, Jensen ET, Shaheen NJ, Barritt AS, Lieber SR, Kochar B, Barnes EL, Fan YC, Pate V, Galanko J, Baron TH, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology. 2019;156(1): 254-272.e11.
https://doi.org/10.1053/j.gastro.2018.08.063
Olson E, Perelman A, Birk JW. Acute management of pancreatitis: the key to best outcomes. Postgrad Med J. 2019;95(1124):328-333.
https://doi.org/10.1136/postgradmedj-2018-136034
Tenner S, Baillie J, DeWitt J, Vege SS; American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400-15;1416.
https://doi.org/10.1038/ajg.2013.218
Bollen TL. Acute pancreatitis: international classification and nomenclature. Clin Radiol. 2016;71(2):121-33. https://doi.org/10.1016/j.crad.2015.09.013
van Dijk SM, Hallensleben NDL, van Santvoort HC, Fockens P, van Goor H, Bruno MJ, Besselink MG; Dutch Pancreatitis Study Group. Acute pancreatitis: recent advances through randomised trials. Gut. 2017;66(11):2024-2032.
https://doi.org/10.1136/gutjnl-2016-313595
Petrov MS, Pylypchuk RD, Emelyanov NV. Systematic review: nutritional support in acute pancreatitis. Alim Pharmacol Ther. 2008;28(6):704-712.
https://doi.org/10.1111/j.1365-2036.2008.03786.x
Singh P, Garg PK. Pathophysiological mechanisms in acute pancreatitis: Current understanding. Indian J Gastroenterol. 2016;35(3):153-66.
https://doi.org/10.1007/s12664-016-0647-y
Schietroma M, Pessia B, Carlei F, Mariani P, Sista F, Amicucci G. Intestinal permeability and systemic endotoxemia in patients with acute pancreatitis. Ann Ital Chir. 2016;87:138-44.
Gupta R, Patel K, Calder PC, Yaqoob P, Primrose JN, Johnson CD. A randomised clinical trial to assess the effect of total enteral and total parenteral nutritional support on metabolic, inflammatory and oxidative markers in patients with predicted severe acute pancreatitis (APACHE II > or =6). Pancreatology. 2003;3(5):406-13.
https://doi.org/10.1159/000073657
Ramanathan M, Aadam AA. Nutrition Management in Acute Pancreatitis. Nutr Clin Pract. 2019;34 Suppl 1:S7-S12.
https://doi.org/10.1002/ncp.10386
Vaughn VM, Shuster D, Rogers MAM, Mann J, Conte ML, Saint S, Chopra V. Early Versus Delayed Feeding in Patients With Acute Pancreatitis: A Systematic Review. Ann Intern Med. 2017;166(12):883-892.
https://doi.org/10.7326/M16-2533
Zhang D, Li H, Li Y, Qu L. Gut rest strategy and trophic feeding in the acute phase of critical illness with acute gastrointestinal injury. Nutr Res Rev. 2019;32(2):176-182.https://doi.org/10.1017/S0954422419000027
Pan LL, Li J, Shamoon M, Bhatia M, Sun J. Recent advances on nutrition in treatment of acute pancreatitis. Front Immunol. 2017;8:762.
https://doi.org/10.3389/fimmu.2017.00762
Gianotti L, Meier R, Lobo DN, Bassi C, Dejong CH, Ockenga J, Irtun O, MacFie J; ESPEN. ESPEN guidelines on parenteral nutrition: pancreas. Clin Nutr. 2009;28(4):428-35.
https://doi.org/10.1016/j.clnu.2009.04.003
Ziegler TR. Parenteral nutrition in the critically ill patient. N Engl J Med. 2009;361(11):1088-97.
https://doi.org/10.1056/NEJMct0806956
Storck LJ, Imoberdorf R, Ballmer PE. Nutrition in Gastrointestinal Disease: Liver, Pancreatic, and Inflammatory Bowel Disease. J Clin Med. 2019;8(8). pii: E1098.
https://doi.org/10.3390/jcm8081098
Pasquel FJ, Spiegelman R, McCauley M, Smiley D, Umpierrez D, Johnson R, Rhee M, Gatcliffe C, Lin E, Umpierrez E, Peng L, Umpierrez GE. Hyperglycemia during total parenteral nutrition: an important marker of poor outcome and mortality in hospitalized patients. Diabetes Care. 2010;33(4):739-741.
https://doi.org/10.2337/dc09-1748
Petrov MS, Whelan K. Comparison of complications attributable to enteral and parenteral nutrition in predicted severe acute pancreatitis: a systematic review and meta-analysis. Br J Nutr. 2010;103(9):1287-95.
https://doi.org/10.1017/S0007114510000887
Petrov MS. Gastric feeding and “gut rousing” in acute pancreatitis. Nutr Clin Pract. 2014;29(3):287-90.
https://doi.org/10.1177/0884533614528986
Al-Omran M, Albalawi ZH, Tashkandi MF, Al-Ansary LA. Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst Rev. 2010;(1):Cd002837. https://doi.org/10.1002/14651858.CD002837.pub2
Yao H, He C, Deng L, Liao G. Enteral versus parenteral nutrition in critically ill patients with severe pancreatitis: a meta-analysis. Eur J Clin Nutr. 2018;72(1):66-68.
https://doi.org/10.1038/ejcn.2017.139
Wu P, Li L, Sun W. Efficacy comparisons of enteral nutrition and parenteral nutrition in patients with severe acute pancreatitis: a meta- analysis from randomized controlled trials. Biosci Rep. 2018;38(6):pii: BSR20181515.
https://doi.org/10.1042/BSR20181515
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN; American Gastroenterological Association Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018;154(4):1096-1101.
https://doi.org/10.1053/j.gastro.2018.01.032
Feng P, He C, Liao G, Chen Y. Early enteral nutrition versus delayed enteral nutrition in acute pancreatitis: A PRISMA compliant systematic review and meta-analysis. Medicine (Baltimore). 2017;96(46):e8648.
https://doi.org/10.1097/MD.0000000000008648
Song J, Zhong Y, Lu X, Kang X, Wang Y, Guo W, Liu J, Yang Y, Pei L. Enteral nutrition provided within 48 hours after admission in severe acute pancreatitis: a systematic review and meta-analysis. Medicine (Baltimore). 2018;97(34):e11871.
https://doi.org/10.1097/MD.0000000000011871
Qi D, Yu B, Huang J, Peng M. Meta-Analysis of Early Enteral Nutrition Provided Within 24 Hours of Admission on Clinical Outcomes in Acute Pancreatitis. JPEN J Parenter Enteral Nutr. 2018;42(7):1139-1147.
https://doi.org/10.1002/jpen.1139
Valverde-López F, Wilcox CM, Redondo-Cerezo E. Evaluation and management of acute pancreatitis in Spain. Gastroenterol Hepatol. 2018;41(10):618-628.
https://doi.org/10.1016/j.gastrohep.2018.06.012
Moggia E, Koti R, Belgaumkar AP, Fazio F, Pereira SP, Davidson BR, Gurusamy KS. Pharmacological interventions for acute pancreatitis. Cochrane Database Syst Rev. 2017;4(4):CD011384.
https://doi.org/10.1002/14651858.CD011384.pub2
Chang YS, Fu HQ, Xiao YM, Liu JC. Nasogastric or nasojejunal feeding in predicted severe acute pancreatitis: a meta-analysis. Crit Care. 2013;17(3):R118.
https://doi.org/10.1186/cc12790
Faghih M, Fan C, Singh VK. New Advances in the Treatment of Acute Pancreatitis. Curr Treat Options Gastroenterol. 2019;17(1):146-160.
https://doi.org/10.1007/s11938-019-00223-8
Petrov MS, McIlroy K, Grayson L, Phillips AR, Windsor JA. Early nasogastric tube feeding versus nil per os in mild to moderate acute pancreatitis: a randomized controlled trial. Clin Nutr. 2013;32(5): 697-703.
https://doi.org/10.1016/j.clnu.2012.12.011
Li J, Chen J, Tang W. The consensus of integrative diagnosis and treatment of acute pancreatitis-2017. J Evid Based Med. 2019;12(1):76-88.
https://doi.org/10.1111/jebm.12342
Vege SS, DiMagno MJ, Forsmark CE, Martel M, Barkun AN. Initial medical treatment of acute pancreatitis: American Gastroenterological Association Institute technical review. Gastroenterology. 2018;154(4):1103-1139. https://doi.org/10.1053/j.gastro.2018.01.031
Lodewijkx PJ, Besselink MG, Witteman BJ, Schepers NJ, Gooszen HG, van Santvoort HC, Bakker OJ; Dutch Pancreatitis Study Group. Nutrition in acute pancreatitis: a critical review. Expert Rev Gastroenterol Hepatol. 2016;10(5):571-80.
https://doi.org/10.1586/17474124.2016.1141048
Roberts KM, Nahikian-Nelms M, Ukleja A, Lara LF. Nutritional Aspects of Acute Pancreatitis. Gastroenterol Clin North Am. 2018;47(1):77-94.
https://doi.org/10.1016/j.gtc.2017.10.002
Endo A, Shiraishi A, Fushimi K, Murata K, Otomo Y. Comparative effectiveness of elemental formula in the early enteral nutrition manage- ment of acute pancreatitis: a retrospective cohort study. Ann Intensive Care. 2018;8(1):69.
https://doi.org/10.1186/s13613-018-0414-6
Lariño-Noia J, Lindkvist B, Iglesias-García J, Seijo-Ríos S, Iglesias-Canle J, Domínguez-Muñoz JE. Early and/or immediately full caloric diet versus standard refeeding in mild acute pancreatitis: a randomized open-label trial. Pancreatology. 2014;14(3):167-73.
https://doi.org/10.1016/j.pan.2014.02.008
Tian X, Pi YP, Liu XL, Chen H, Chen WQ. Supplemented Use of Pre-, Pro-, and Synbiotics in Severe Acute Pancreatitis: An Updated Systematic Review and Meta-Analysis of 13 Randomized Controlled Trials. Front Pharmacol. 2018;9:690.
https://doi.org/10.3389/fphar.2018.00690
Ballesteros Pomar MD, González Arnaiz E. Role of prebiotics and probiotics in the functionality of the microbiota in the patients receiving enteral nutrition. Nutr Hosp. 2018;35(Spec no2):18-26.
https://doi.org/10.20960/nh.1956
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, Gervasio JM, Sacks GS, Roberts PR, Compher C; Society of Critical Care Medicine; American Society for Parenteral and Enteral Nutrition. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40(2):159-211.
https://doi.org/10.1177/0148607115621863
Lei QC, Wang XY, Xia XF, Zheng HZ, Bi JC, Tian F, Li N. The role of omega-3 fatty acids in acute pancreatitis: a meta-analysis of randomized controlled trials. Nutrients. 2015;7(4):2261-73.
https://doi.org/10.3390/nu7042261
Jeurnink SM, Nijs MM, Prins HA, Greving JP, Siersema PD. Antioxidants as a treatment for acute pancreatitis: A meta-analysis. Pancreatology. 2015;15(3):203-8.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |