Prevalencia y características histológicas de los pólipos diminutos del recto y del sigmoides en una población colombiana
DOI:
https://doi.org/10.22516/25007440.363Palabras clave:
Pólipos diminutos, pólipos, adenomasResumen
Introducción: el cáncer de colon y recto (CCR) se origina a partir de pólipos adenomatosos y serrados. Por tanto, se recomienda que todos los pólipos colónicos sean resecados y enviados a patología. Sin embargo, en los pólipos diminutos (<5 mm) del recto y del sigmoides existe controversia sobre esta conducta, razón por la cual se ha planteado la estrategia de resecar y descartar o dejar in situ, a partir de la utilización de endoscopios avanzados (con una imagen de banda angosta [Narrow Band Imaging, NBI] u otras), y se logre concordancia con la histopatología, superior al 90 %. En nuestro medio, no hay estudios prospectivos con luz blanca sobre la prevalencia y las características histológicas de estos pólipos en el recto y el sigmoides. Por esta razón, se desarrolló este trabajo.
Materiales y métodos: estudio de prevalencia analítica, prospectivo. Se incluyeron las colonoscopias de tamización realizadas en la Unidad de Gastroenterología de la Clínica Fundadores de Bogotá, entre enero y julio de 2018.
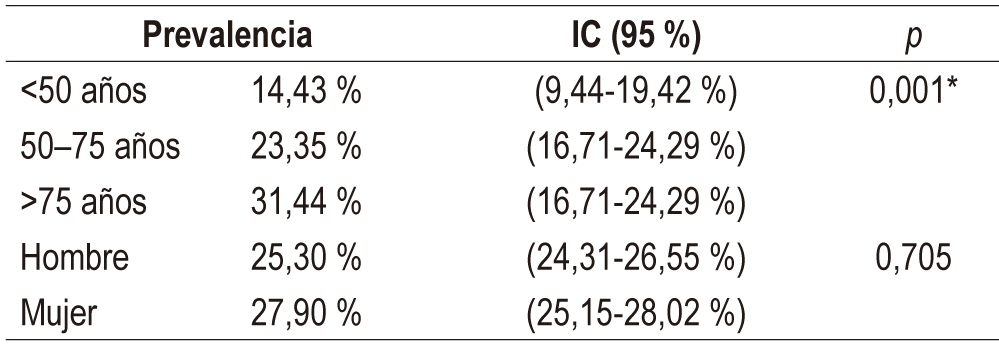
Resultados: se incluyeron 719 pacientes. La prevalencia de pólipos diminutos en el recto y el sigmoides fue del 27 % (intervalo de confianza [IC], 95 %: 23,7-30,2 %). El 50 % eran pólipos adenomatosos, mientras que en 8 casos se presentó una displasia de alto grado (DAG). Entre los pólipos diminutos, 3 fueron tumores neuroendocrinos. No hubo cáncer en ninguna de las lesiones.
Conclusiones: la mitad de los pólipos diminutos encontrados fueron adenomatosos y 8 (0,83 %) tuvieron DAG. Recomendamos resecar todos los pólipos diminutos hasta que los estudios locales realizados con NBI u otra tecnología demostrasen la capacidad para discriminar en más del 90 % los pólipos hiperplásicos (dejarlos in situ) o adenomatosos (resecarlos).
Descargas
Referencias bibliográficas
Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3(4):524-548. https://doi.org/10.1001/jamaoncol.2016.5688
Gil FL, Torres M, Riveros SV, Castaño R, Ibáñez H, Huertas MM, et al. Guía de práctica clínica para la tamización del cáncer colorrectal – 2015. Rev Col Gastroenterol. 2015;30(1 Suppl ):67-74.
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58(6 Suppl):S3-43. https://doi.org/10.1016/S0016-5107(03)02159-X
Rex DK, Alikhan M, Cummings O, Ulbright TM. Accuracy of pathologic interpretation of colorectal polyps by general pathologists in Community practice. Gastrointest Endosc. 1999;50(4):468-74. https://doi.org/10.1016/S0016-5107(99)70067-2
Pickhardt PJ, Kim DH. Colorectal cancer screening with CT colonography: key concepts regarding polyp prevalence, size, histology, morphology, and natural history. AJR Am J Roentgenol. 2009;193(1):40-6. https://doi.org/10.2214/AJR.08.1709
Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329(27):1977-81. https://doi.org/10.1056/NEJM199312303292701
Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154(1):22-30. https://doi.org/10.7326/0003-4819-154-1-201101040-00004
Brenner H, Altenhofen L, Stock C, Hoffmeister M. Natural history of colorectal adenomas: birth cohort analysis among 3.6 million participants of screening colonoscopy. Cancer Epidemiol Biomarkers Prev. 2013;22(6):1043-51. https://doi.org/10.1158/1055-9965.EPI-13-0162
Regula J, Rupinski M, Kraszewska E, Polkowski M, Pachlewski J, Orlowska J, et al. Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N Engl J Med. 2006;355(18):1863-72. https://doi.org/10.1056/NEJMoa054967
Patel S, Scott FI, McGill S, Kaltenbach TR, Ahnen D, Das A, et al. 945 Cost Effectiveness Analysis Evaluating Real-Time Characterization of Diminutive Colorectal Polyp Histology Using Narrow Band Imaging (NBI): Implications for the Resect and Discard Strategy. 2017;85(5): AB116-AB117. https://doi.org/10.1016/j.gie.2017.03.190
Kessler WR, Imperiale TF, Klein RW, Wielage RC, Rex DK. A quantitative assessment of the risks and cost savings of forgoing histologic examination of diminutive polyps. Endoscopy. 2011;43(8):683-91. https://doi.org/10.1055/s-0030-1256381
Hassan C, Pickhardt PJ, Rex DK. A resect and discard strategy would improve cost-effectiveness of colorectal cancer screening. Clin Gastroenterol Hepatol. 2010;8(10):865-9, 869.e1-3. https://doi.org/10.1016/j.cgh.2010.05.018
Rex DK, Kahi C, O’Brien M, Levin TR, Pohl H, Rastogi A, et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;73(3):419-22. https://doi.org/10.1016/j.gie.2011.01.023
Kamiński MF, Hassan C, Bisschops R, Pohl J, Pellisé M, Dekker E, et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2014;46(5):435-49. https://doi.org/10.1055/s-0034-1365348
Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69(3 Pt 2):620–625. https://doi.org/10.1016/j.gie.2008.05.057
Zhao S, Yang X, Meng Q, Wang S, Fang J, Qian W, et al. Impact of the supine position versus left horizontal position on colonoscopy insertion: a 2-center, randomized controlled trial. Gastrointest Endosc. 2019;89(6):1193-1201.e1. https://doi.org/10.1016/j.gie.2019.01.009
ASGE Standards of Practice Committee, Saltzman JR, Cash BD, Pasha SF, Early DS, Muthusamy VR, et al. Bowel preparation before colonoscopy. Gastrointest Endosc. 2015;81(4):781-94. https://doi.org/10.1016/j.gie.2014.09.048
Lee J. Resection of Diminutive and Small Colorectal Polyps: What Is the Optimal Technique? Clin Endosc. 2016;49(4):355–358. https://doi.org/10.5946/ce.2016.063
Paggi S, Radaelli F, Repici A, Hassan C. Advances in the removal of diminutive colorectal polyps. Expert Rev Gastroenterol Hepatol. 2015;9(2):237-44. https://doi.org/10.1586/17474124.2014.950955
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American Association of Clinical Endocrinologistis and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Endocr Pract. 2016;22 Suppl 3:1-203. https://doi.org/10.4158/EP161365.GL
Hassan C, Repici A, Zullo A, Kanakadandi V, Sharma P. Colonic polyps: are we ready to resect and discard? Gastrointest Endosc Clin N Am. 2013;23(3):663-78. https://doi.org/10.1016/j.giec.2013.03.005
Ponugoti PL, Cummings OW, Rex DK. Risk of cancer in small and diminutive colorectal polyps. Dig Liver Dis. 2017;49(1):34-37. https://doi.org/10.1016/j.dld.2016.06.025
Lieberman D, Moravec M, Holub J, Michaels L, Eisen G. Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology. 2008;135(4):1100-5. https://doi.org/10.1053/j.gastro.2008.06.083
Gupta N, Bansal A, Rao D, Early DS, Jonnalagadda S, Wani SB, et al. Prevalence of advanced histological features in diminutive and small colon polyps. Gastrointest Endosc. 2012;75(5):1022-30. https://doi.org/10.1016/j.gie.2012.01.020
Odom SR, Duffy SD, Barone JE, Ghevariya V, McClane SJ. The rate of adenocarcinoma in endoscopically removed colorectal polyps. Am Surg. 2005;71(12):1024-6.
Church JM. Clinical significance of small colorectal polyps. Dis Colon Rectum. 2004;47(4):481-5. https://doi.org/10.1007/s10350-003-0078-6
Hofstad B, Vatn MH, Andersen SN, Huitfeldt HS, Rognum T, Larsen S, et al. Growth of colorectal polyps: redetection and evaluation of unresected polyps for a period of three years. Gut. 1996;39(3):449-56. https://doi.org/10.1136/gut.39.3.449
Bird-Lieberman E, East JE. Diminutive polyps and future colorectal cancer risk perception: how low do we need to go? Endoscopy. 2018;50(3):197-199. https://doi.org/10.1055/s-0044-100493
von Renteln D, Bouin M, Barkun AN, Weber A, Robertson DJ, Anderson JC, et al. Patients’ willingness to defer resection of diminutive polyps: results of a multicenter survey. Endoscopy. 2018;50(3):221-229. https://doi.org/10.1055/s-0043-121221
Paspatis GA, Tribonias G, Konstantinidis K, Theodoropoulou A, Vardas E, Voudoukis E, et al. A prospective randomized comparison of cold vs hot snare polypectomy in the occurrence of postpolypectomy bleeding in small colonic polyps. Colorectal Dis. 2011;13(10):e345-8. https://doi.org/10.1111/j.1463-1318.2011.02696.x
Ichise Y, Horiuchi A, Nakayama Y, Tanaka N. Prospective randomized comparison of cold snare polypectomy and conventional polypectomy for small colorectal polyps. Digestion. 2011;84(1):78-81. https://doi.org/10.1159/000323959
Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017;49(3):270-297. https://doi.org/10.1055/s-0043-102569
Lieberman D, Brill J, Canto M, DeMarco D, Fennerty B, Gupta N, et al. Management of Diminutive Colon Polyps Based on Endoluminal Imaging. Clin Gastroenterol Hepatol. 2015;13(11):1860-6; quiz e168-9. https://doi.org/10.1016/j.cgh.2015.07.011
Sikong Y, Lin X, Liu K, Wu J, Lin W, Wei N, et al. Effectiveness of systematic training in the application of narrow-band imaging international colorectal endoscopic (NICE) classification for optical diagnosis of colorectal polyps: Experience from a single center in China. Dig Endosc. 2016;28(5):583-91. https://doi.org/10.1111/den.12600
Atkinson NS, East JE. Optical biopsy and sessile serrated polyps: Is DISCARD dead? Long live DISCARD-lite! Gastrointest Endosc. 2015;82(1):118-21. https://doi.org/10.1016/j.gie.2015.01.059
Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006;355(24):2533-41. https://doi.org/10.1056/NEJMoa055498
Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143(3):844-857. https://doi.org/10.1053/j.gastro.2012.06.001
Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370(14):1298-306. https://doi.org/10.1056/NEJMoa1309086
Basuroy R, Haji A, Ramage JK, Quaglia A, Srirajaskanthan R. Review article: the investigation and management of rectal neuroendocrine tumours. Aliment Pharmacol Ther. 2016;44(4):332-45. https://doi.org/10.1111/apt.13697
Kaminski M, Polkowski M, Regula J: Prevalence and endoscopic features of rectal neuroendocrine tumors (carcinoids) among 50148 participants of the Polish colorectal-cancer screening programme. Gut. 2007;56(suppl III):A310.
Scherübl H. Rectal carcinoids are on the rise: early detection by screening endoscopy. Endoscopy. 2009;41(2):162-5. https://doi.org/10.1055/s-0028-1119456
Rex DK, Hassan C, Bourke MJ. The colonoscopist’s guide to the vocabulary of colorectal neoplasia: histology, morphology, and management. Gastrointest Endosc. 2017;86(2):253-263. https://doi.org/10.1016/j.gie.2017.03.1546
Shah TU, Voils CI, McNeil R, Wu R, Fisher DA. Understanding gastroenterologista adherence to polyp surveillance guidelines. Am J Gastroenterol. 2012;107(9):1283-7. https://doi.org/10.1038/ajg.2012.59
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |
















