Management of upper gastrointestinal bleeding in patients with SARS-COV-2 infection in a hospital in Lima-Peru
DOI:
https://doi.org/10.22516/25007440.742Keywords:
SARS-CoV-2, Treatment, Endoscopy, Gastrointestinal bleedingAbstract
Introduction: The SARS-CoV-2 pandemic has led to the restructuring of digestive endoscopy units around the world, limiting endoscopic procedures and prioritizing emergency indications such as upper gastrointestinal hemorrhage (UGH). However, there is little evidence regarding its impact on evolution and outcomes.
Objective: To evaluate the management of UGH in the context of the SARS-CoV-2 coronavirus pandemic.
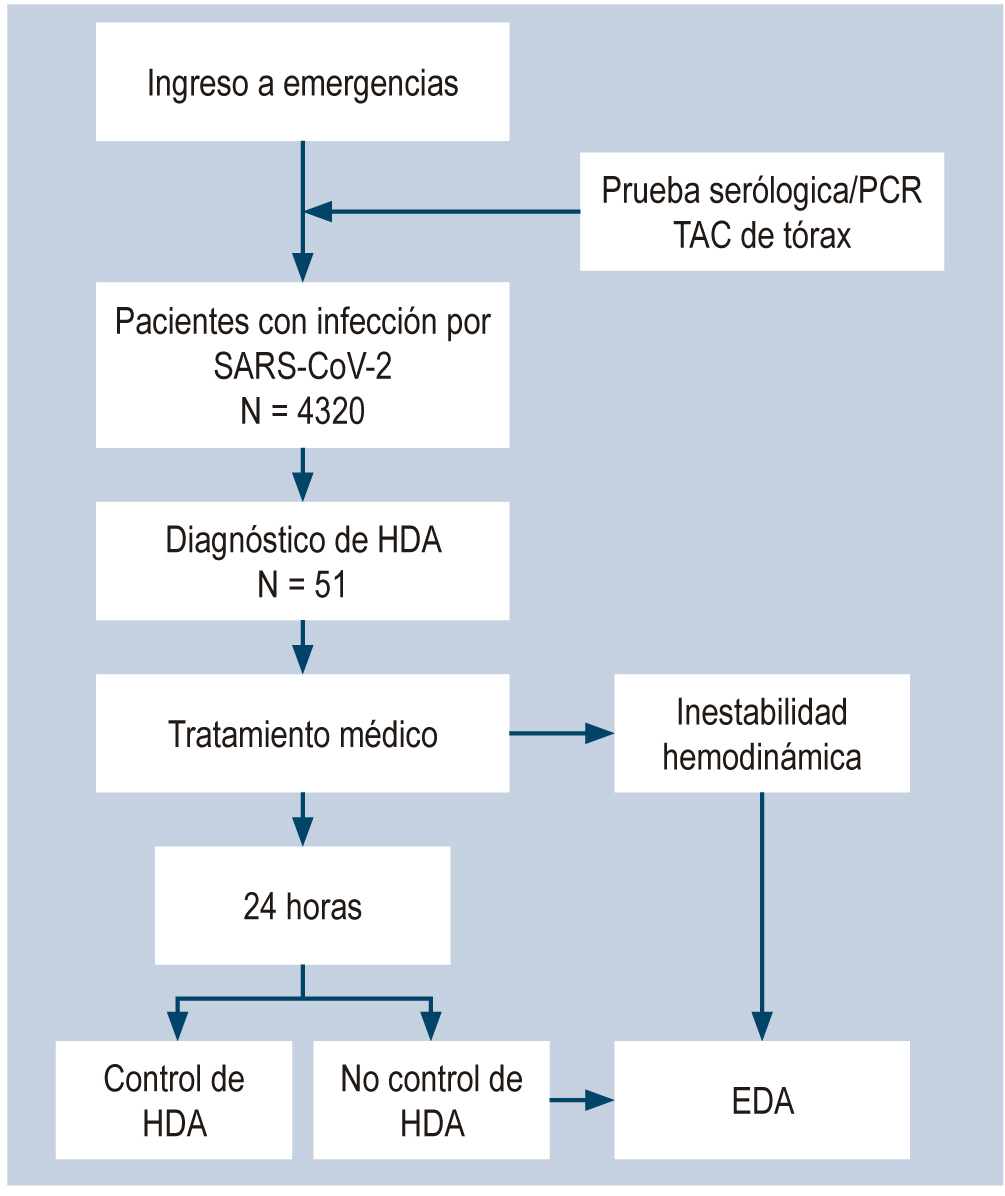
Materials and methods: Observational, descriptive, retrospective study carried out between March and August 2020 in patients with diagnosis of UGH and SARS-CoV-2 infection.
Results: Of 4 320 patients with SARS-CoV-2 infection, 51 had UGH on admission. The median age of the population was 70 years and 58.8% were male. Glasgow-Blatchford Bleeding Score (GBS) of ≥12 was obtained in 56.9%. Oxygen support was required by 21.6%. 34 (66.7%) patients received medical treatment only, while 17 (33.3%) received medical treatment plus upper gastrointestinal endoscopy (UGE), of which 6 (35.3%) underwent therapeutic endoscopy. Peptic ulcer disease was the most frequent finding. When comparing the type of treatment received, there were no significant differences between the number of red blood cell transfusions, rebleeding, re-admission due to UGH, hospital stay, or mortality secondary to UGH. Overall mortality was 25.4% (13 patients), mainly due to respiratory failure due to SARS-CoV-2.
Conclusions: A reduction in the number of emergency upper gastrointestinal endoscopies for UGH was observed during the current pandemic, as well as a longer than standard time for their performance. More than 80% of patients who received medical treatment alone evolved favorably and only one third of the patients who underwent UGE required endoscopic therapy.
Downloads
References
WHO | Pneumonia of unknown cause – China. WHO [Internet]. 2020 [consultado el 13 de octubre de 2020]. Disponible en: http://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/
Tan W, Zhao X, Ma X, Wang W, Niu P, Xu W, Cao GF, Wu G. A Novel Coronavirus Genome Identified in a Cluster of Pneumonia Cases — Wuhan, China 2019−2020. China CDC Wkly. 2020;2(4):61–2. https://doi.org/10.46234/ccdcw2020.017
WHO. WHO Director-General’s opening remarks at themedia briefing on COVID-19 - 11 March 2020 [Internet]. WHO Director General’s speeches. 2020. p. 4. [Consultado el 13 de octubre de 2020]. Disponible en: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarksat-the-media-briefing-on-covid-19---11-march-2020
WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. [Consultado el 21 de mayo de 2021]. Disponible en: https://covid19.who.int/
Danese S, Ran ZH, Repici A, Tong J, Omodei P, Aghemo A, Malesci A. Gastroenterology department operational reorganisation at the time of covid-19 outbreak: an Italian and Chinese experience. Gut. 2020;69(6):981-83. http://dx.doi.org/10.1136/gutjnl-2020-321143
Chan SM, Ma TW, Ka-Chun Chong M, Chan DL, Ng EKW, Chiu PWY. A proof of concept study: Esophagogastroduodenoscopy is an aerosol-generating procedure and continuous oral suction during the procedure reduces the amount of aerosol generated. Gastroenterology. 2020. https://doi.org/10.1053/j.gastro.2020.07.002
Gralnek IM, Hassan C, Beilenhoff U, Antonelli G, Ebigbo A, Pellisè M, Arvanitakis M, Bhandari P, Bisschops R, Van Hooft JE, Kaminski MF, Triantafyllou K, Webster G, Pohl H, Dunkley I, Fehrke B, Gazic M, Gjergek T, Maasen S, Waagenes W, de Pater M, Ponchon T, Siersema PD, Messmann H, Dinis-Ribeiro M. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020;52(6):483-90. https://doi.org/10.1055/a-1155-6229
Soetikno R, Teoh AYB, Kaltenbach T, Lau JYW, Asokkumar R, Cabral-Prodigalidad P, Shergill A. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. 2020;92(1):176-83. https://doi.org/10.1016/j.gie.2020.03.3758
Chiu PWY, Ng SC, Inoue H, Reddy DN, Ling Hu E, Cho JY, Ho LK, Hewett DG, Chiu HM, Rerknimitr R, Wang HP, Ho SH, Seo DW, Goh KL, Tajiri H, Kitano S, Chan FKL. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements). Gut. 2020;69(6):991–6. http://dx.doi.org/10.1136/gutjnl-2020-321185
Castro-Filho EC, Castro R, Fernandes FF, Pereira G, Perazzo H. Gastrointestinal endoscopy during the COVID-19 pandemic: an updated review of guidelines and statements from international and national societies. Gastrointest Endosc. 2020;92(2):440-445.e6. https://doi.org/10.1016/j.gie.2020.03.3854
Lanas A, Dumonceau JM, Hunt RH, Fujishiro M, Scheiman JM, Gralnek IM, Campbell HE, Rostom A, Villanueva C, Sung JJY. Non-variceal upper gastrointestinal bleeding. Nat Rev Dis Primers. 2018;4:18020. https://doi.org/10.1038/nrdp.2018.20
Lau JYW, Yu Y, Tang RSY, Chan HCH, Yip HC, Chan SM, Luk SWY, Wong SH, Lau LHS, Lui RN, Chan TT, Mak JWY, Chan FKL, Sung JJY. Timing of endoscopy for acute upper gastrointestinal bleeding. N Engl J Med. 2020;382(14):1299-1308. https://doi.org/10.1056/NEJMoa1912484
Barkun AN, Almadi M, Kuipers EJ, Laine L, Sung J, Tse F, Leontiadis GI, Abraham NS, Calvet X, Chan FKL, Douketis J, Enns R, Gralnek IM, Jairath V, Jensen D, Lau J, Lip GYH, Loffroy R, Maluf-Filho F, Meltzer AC, Reddy N, Saltzman JR, Marshall JK, Bardou M. Management of Nonvariceal Upper Gastrointestinal Bleeding: Guideline Recommendations From the International Consensus Group. Ann Intern Med. 2019;171(11):805-22. https://doi.org/10.7326/M19-1795
Shalimar, Vaishnav M, Elhence A, Kumar R, Mohta S, Palle C, Kumar P, Ranjan M, Vajpai T, Prasad S, Yegurla J, Dhooria A, Banyal V, Agarwal S, Bansal R, Bhattacharjee S, Aggarwal R, Soni KD, Rudravaram S, Singh AK, Altaf I, Choudekar A, Mahapatra SJ, Gunjan D, Kedia S, Makharia G, Trikha A, Garg P, Saraya A. Outcome of Conservative Therapy in Coronavirus disease-2019 Patients Presenting With Gastrointestinal Bleeding. J Clin Exp Hepatol. 2021;11(3):327-333. https://doi.org/10.1016/j.jceh.2020.09.007
Cavaliere K, Levine C, Wander P, Sejpal DV, Trindade AJ. Management of upper GI bleeding in patients with COVID-19 pneumonia. Gastrointest Endosc. 2020;92(2):454-55. https://doi.org/10.1016/j.gie.2020.04.028
Baradarian R, Ramdhaney S, Chapalamadugu R, Skoczylas L, Wang K, Rivilis S, Remus K, Mayer I, Iswara K, Tenner S. Early intensive resuscitation of patients with upper gastrointestinal bleeding decreases mortality. Am J Gastroenterol. 2004;99(4):619-22. https://doi.org/10.1111/j.1572-0241.2004.04073.x.
Aguila EJT, Cua IHY, Raymundo NTV. The Dilemma in the Management of Gastrointestinal Bleeding During the COVID-19 Pandemic. Gastroenterology. 2021;160(5):1889-90. https://doi.org/10.1053/j.gastro.2020.05.088
Tong ZD, Tang A, Li KF, Li P, Wang HL, Yi JP, Zhang YL, Yan JB. Potential Presymptomatic Transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. 2020;26(5):1052-54. https://doi.org/10.3201/eid2605.200198
Deeks JJ, Dinnes J, Takwoingi Y, Davenport C, Spijker R, Taylor-Phillips S, Adriano A, Beese S, Dretzke J, Ferrante di Ruffano L, Harris IM, Price MJ, Dittrich S, Emperador D, Hooft L, Leeflang MM, Van den Bruel A; Cochrane COVID-19 Diagnostic Test Accuracy Group. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst Rev. 2020;6(6):CD013652. https://doi.org/10.1002/14651858.CD013652
Clinical management of COVID-19. Geneva: World Health Organization; 2020. [Consultado el 14 de octubre de 2020]. Disponible en: https://www.who.int/publications/i/item/clinical-management-of-covid-19
Laursen SB, Leontiadis GI, Stanley AJ, Møller MH, Hansen JM, Schaffalitzky de Muckadell OB. Relationship between timing of endoscopy and mortality in patients with peptic ulcer bleeding: a nationwide cohort study. Gastrointest Endosc. 2017;85(5):936-944.e3. https://doi.org/10.1016/j.gie.2016.08.049
Martin TA, Wan DW, Hajifathalian K, Tewani S, Shah SL, Mehta A, Kaplan A, Ghosh G, Choi AJ, Krisko TI, Fortune BE, Crawford CV, Sharaiha RZ. Gastrointestinal Bleeding in Patients With Coronavirus Disease 2019: A Matched Case-Control Study. Am J Gastroenterol. 2020;115(10):1609-16. https://doi.org/10.14309/ajg.0000000000000805
Mauro A, De Grazia F, Lenti MV, Penagini R, Frego R, Ardizzone S, Savarino E, Radaelli F, Bosani M, Orlando S, Amato A, Dinelli M, Ferretti F, Filippi E, Vecchi M, Stradella D, Bardone M, Pozzi L, Rovedatti L, Strada E, Di Sabatino A. Upper gastrointestinal bleeding in COVID-19 inpatients: Incidence and management in a multicenter experience from Northern Italy. Clin Res Hepatol Gastroenterol. 2021;45(3):101521. https://doi.org/10.1016/j.clinre.2020.07.025
Gadiparthi C, Perisetti A, Sayana H, Tharian B, Inamdar S, Korman A. Gastrointestinal Bleeding in Patients with Severe SARS-CoV-2. Am J Gastroenterol. 2020;115(8):1283-85. https://doi.org/10.14309/ajg.0000000000000719
Barrett LF, Lo KB, Stanek SR, Walter JW. Self-limited gastrointestinal bleeding in COVID-19. Clin Res Hepatol Gastroenterol. 2020;44(4):e77-e80. https://doi.org/10.1016/j.clinre.2020.06.015
Kim J, Doyle JB, Blackett JW, May B, Hur C, Lebwohl B; HIRE study group. Effect of the Coronavirus 2019 Pandemic on Outcomes for Patients Admitted With Gastrointestinal Bleeding in New York City. Gastroenterology. 2020;159(3):1155-57.e1. https://doi.org/10.1053/j.gastro.2020.05.031
Perisetti A, Goyal H, Sharma N. Gastrointestinal Endoscopy in the Era of COVID-19. Front Med 2020;7:587602.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














