Granulomatous hepatitis, deciphering an elusive spectrum: a clinical case-based approach
DOI:
https://doi.org/10.22516/25007440.980Keywords:
Granuloma, Hepatitis, Sarcoidosis, Tuberculosis, Fever of unknown originAbstract
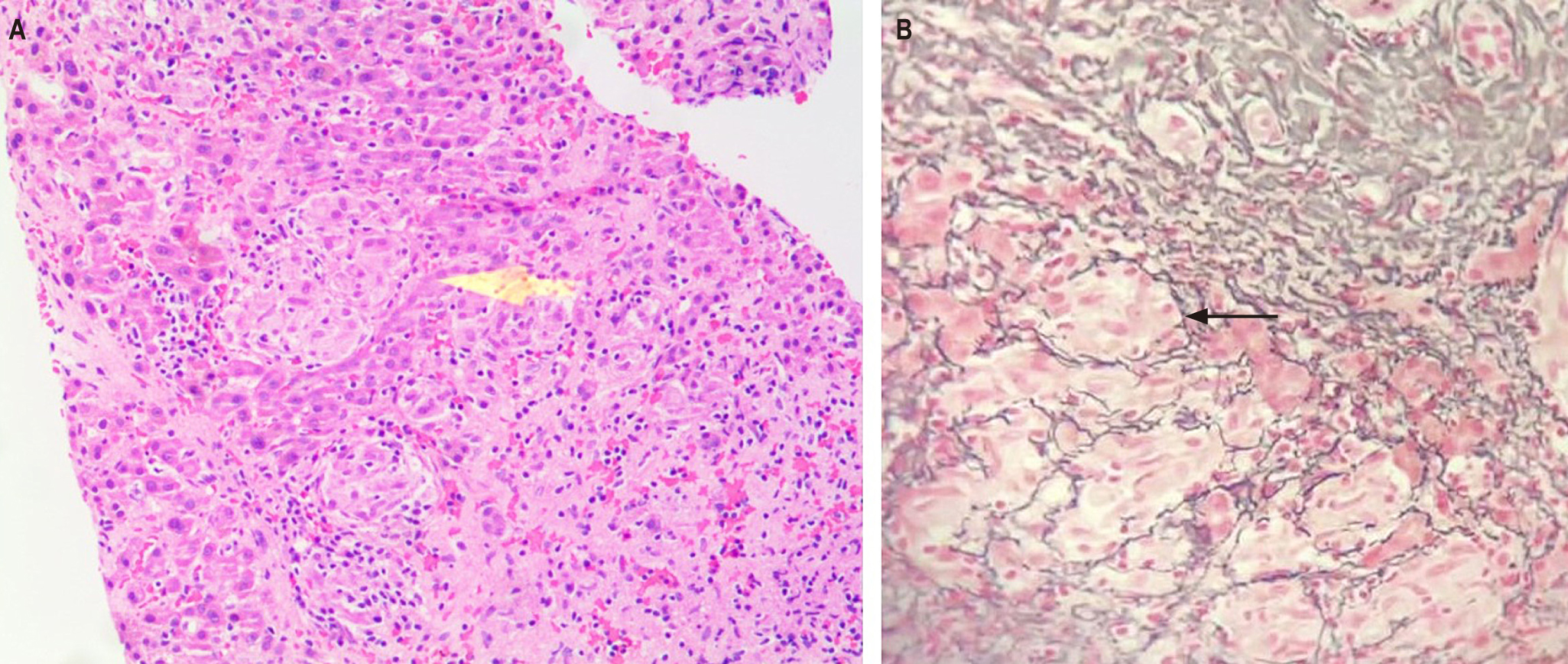
Granulomatous hepatitis is a well-defined histopathologic entity characterized by aggregates of modified macrophages (epithelioid in appearance) and other inflammatory cells that accumulate after persistent exposure to antigens. It induces a cellular immune response mediated by the release of various cytokines (including interferon-gamma [INF-γ], tumor necrosis factor-alpha [TNF-α], and interleukin 12 [IL-12]) that stimulate mononuclear cell fusion, culminating in the formation of multinucleated giant cells with a surrounding border of lymphocytes and fibroblasts. It represents between 2% and 15% of all pathological liver studies, usually during an infiltrative or cholestatic biochemical pattern. A practical approach is proposed based on a challenging clinical case of a patient with a fever of unknown origin in an intermediate incidence area for tuberculosis, such as Colombia.
Downloads
References
Holtz T, Moseley RH, Scheiman JM. Liver Biopsy in Fever of Unknown Origin. J Clin Gastroenterol. 1993;17(1):29-32. https://doi.org/10.1097/00004836-199307000-00009
Mora C, Bastidas Goyes AR, Patiño J, Vera JD, Beltrán A, Mutis C, et al. Prevalencia de tuberculosis latente determinada mediante la prueba de derivado proteico purificado (PPD) en una población de pacientes adultos con artritis reumatoide llevados a terapia biotecnológica. Rev Colomb Reumatol. 2021;28(3):178-83. https://doi.org/10.1016/j.rcreu.2020.08.004
Amado Garzón S, Moreno Mercado S, Martínez Vernaza S, Lasso JI, Laserna A. Tuberculosis extrapulmonar, un reto clínico vigente. Universitas Médica. 2020;61(4). https://doi.org/10.11144/Javeriana.umed61-4.reto
Coash M, Forouhar F, Wu CH, Wu GY. Granulomatous liver diseases: A review. J Formos Med Assoc. 2012;111(1):3-13. https://doi.org/10.1016/j.jfma.2011.11.023
Gaya DR. Hepatic granulomas: a 10 year single centre experience. J Clin Pathol. 2003;56(11):850-3. https://doi.org/10.1136/jcp.56.11.850
Choi EYK, Lamps LW. Granulomas in the Liver, with a Focus on Infectious Causes. Surg Pathol Clin. 2018;11(2):231-50. https://doi.org/10.1016/j.path.2018.02.008
James DG. A clinicopathological classification of granulomatous disorders. Postgrad Med J. 2000;76(898):457-65. https://doi.org/10.1136/pmj.76.898.457
Álvarez SZ. Hepatobiliary tuberculosis. J Gastroenterol Hepatol. 1998;13(8):833-9. https://doi.org/10.1111/j.1440-1746.1998.tb00743.x
Almadi MA, Aljebreen AM, Sanai FM, Marcus V, AlMeghaiseeb ES, Ghosh S. New insights into gastrointestinal and hepatic granulomatous disorders. Nat Rev Gastroenterol Hepatol. 2011;8(8):455-66. https://doi.org/10.1038/nrgastro.2011.115
Purohit M. Laboratory Diagnosis of Extra-pulmonary Tuberculosis (EPTB) in Resource- constrained Setting: State of the Art, Challenges and the Need. J Clin Diagn Res. 2015;9(4):EE01-6. https://doi.org/10.7860/JCDR/2015/12422.5792
Ayala US, Padilla ML. Diagnosis and treatment of hepatic sarcoidosis. Curr Treat Options Gastroenterol. 2006;9(6):475-83. https://doi.org/10.1007/s11938-006-0004-9
Farooq PD, Potosky DR. The Klatskin Tumor That Wasn’t: An Unusual Presentation of Sarcoidosis. ACG Case Rep J. 2016;3(1):e141. https://doi.org/10.14309/crj.2016.114
Judson MA. Hepatic, Splenic, and Gastrointestinal Involvement with Sarcoidosis. Semin Respir Crit Care Med. 2002;23(6):529-42. https://doi.org/10.1055/s-2002-36517
Devaney K, Goodman ZD, Epstein MS, Zimmerman HJ, Ishak KG. Hepatic Sarcoidosis. Am J Surg Pathol. 1993;17(12):1272-80. https://doi.org/10.1097/00000478-199312000-00009
Momah N, Otesile A, Pawa R, Shedlofsky S. Sarcoidosis Presenting as Necrotizing Sarcoid Granulomatosis of the Liver, Sclerosing Cholangitis, and Gastric Ulcer. ACG Case Rep J. 2014;1(3):164-6. https://doi.org/10.14309/crj.2014.38
Narula N, Iannuzzi M. Sarcoidosis: Pitfalls and Challenging Mimickers. Front Med (Lausanne). 2021;7:594275. https://doi.org/10.3389/fmed.2020.594275
Badar F, Azfar SF, Ahmad I, Yasmeen S, Kirmani S. Diagnostic Difficulties in Differentiating Sarcoidosis from Tuberculosis. Oman Med J. 2011;26(3):210-1. https://doi.org/10.5001/omj.2011.53
Grenier P, Valeyre D, Cluzel P, Brauner MW, Lenoir S, Chastang C. Chronic diffuse interstitial lung disease: diagnostic value of chest radiography and high-resolution CT. Radiology. 1991;179(1):123-32. https://doi.org/10.1148/radiology.179.1.2006262
Crouser ED, Maier LA, Wilson KC, Bonham CA, Morgenthau AS, Patterson KC, et al. Diagnosis and Detection of Sarcoidosis. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;201(8):e26-51. https://doi.org/10.1164/rccm.202002-0251ST
Lim EJ, Johnson PDR, Crowley P, Gow PJ. Granulomatous hepatitis: tuberculosis or not? Med J Aust. 2008;188(3):166-7. https://doi.org/10.5694/j.1326-5377.2008.tb01564.x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














