Ultrasonido endoscópico, aplicaciones actuales en tumores sólidos gastrointestinales
DOI:
https://doi.org/10.22516/25007440.521Palabras clave:
Endosonografía, estadificación de neoplasias, neoplasias gastrointestinales, neoplasias pancreáticasResumen
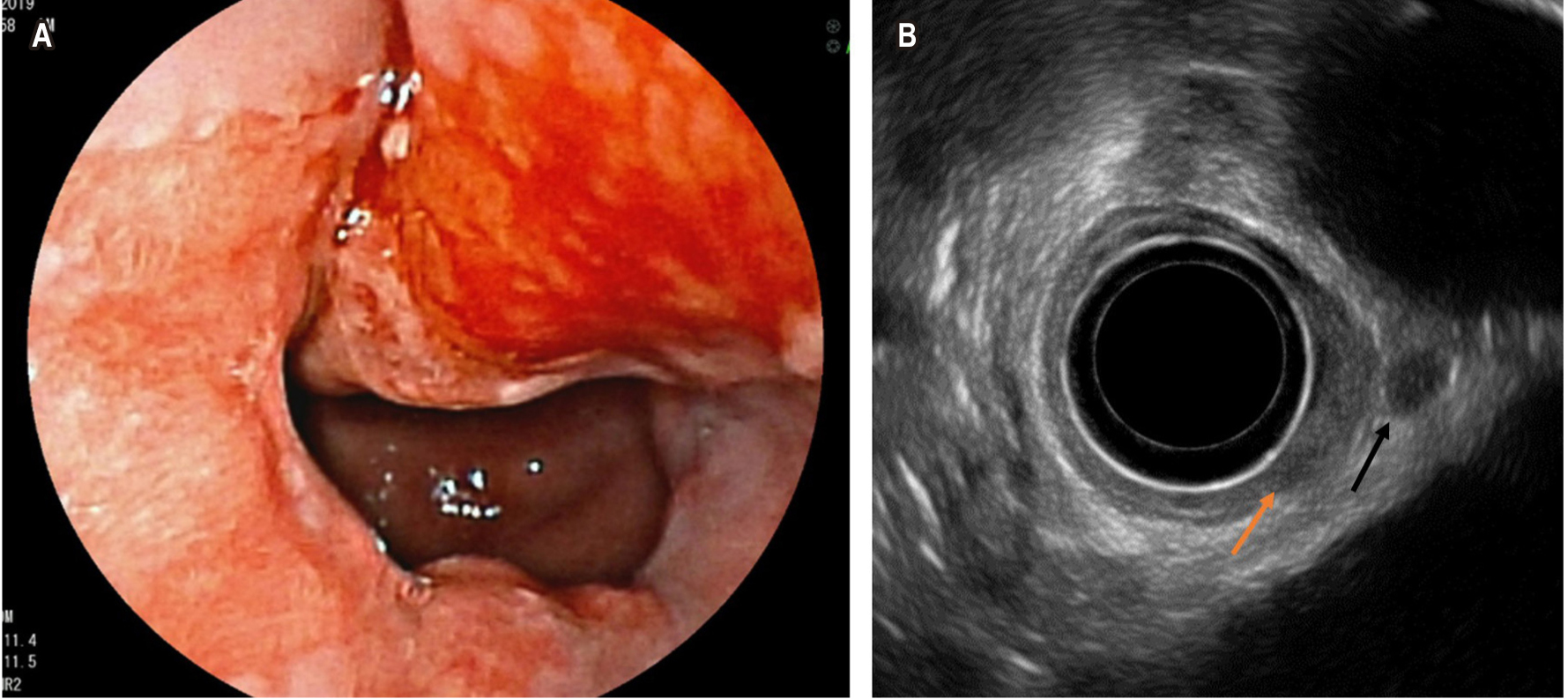
La endosonografía es un método diagnóstico que viene revolucionando el abordaje de los pacientes con tumores del tracto gastrointestinal y de otros órganos y estructuras extradigestivas. En la actualidad, se viene posicionando como un método de elección en la evaluación de lesiones subepiteliales gastrointestinales, además en la estadificación de muchos tumores gastrointestinales como esófago, estomago, recto, páncreas. Por lo cual pretendemos hacer una revisión de tema mostrando la evidencia de la endosonografía en indicaciones clásicas y aplicaciones actuales en tumores gastrointestinales.
Descargas
Referencias bibliográficas
Yasuda K. The Handbook of endoscopic ultrasonography in digestive tract. 1st edition. New York: Blackwell; 2000.
Polkowski M, Larghi A, Weynand B, Boustière C, Giovannini M, Pujol B, Dumonceau JM; European Society of Gastrointestinal Endoscopy (ESGE). Learning, techniques, and complications of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline. Endoscopy. 2012;44(2):190-205.
https://doi.org/10.1055/s-0031-1291543
Wani S, Keswani RN, Petersen B, Edmundowicz SA, Walsh CM, Huang C, Cohen J, Cote G. Training in EUS and ERCP: standardizing methods to assess competence. Gastrointest Endosc. 2018;87(6):1371-1382.
https://doi.org/10.1016/j.gie.2018.02.009
Eloubeidi MA, Tamhane A, Lopes TL, Morgan DE, Cerfolio RJ. Cervical esophageal perforations at the time of endoscopic ultrasound: a prospective evaluation of frequency, outcomes, and patient management. Am J Gastroenterol. 2009;104(1):53-6.
https://doi.org/10.1038/ajg.2008.21
Mosquera-Klinger G, Torres Rincón R. Perforación iatrogénica faringoesofágica tratada con prótesis esofágica totalmente cubierta: reporte de caso. Gastroenterol Hepatol. 2019;42(7):429-30.
https://doi.org/10.1016/j.gastrohep.2018.08.008
ASGE Standards of Practice Committee, Early DS, Acosta RD, Chandrasekhara V, Chathadi KV, Decker GA, Evans JA, Fanelli RD, Fisher DA, Fonkalsrud L, Hwang JH, Jue TL, Khashab MA, Lightdale JR, Muthusamy VR, Pasha SF, Saltzman JR, Sharaf RN, Shergill AK, Cash BD. Adverse events associated with EUS and EUS with FNA. Gastrointest Endosc. 2013;77(6):839-43.
https://doi.org/10.1016/j.gie.2013.02.018
Standards of Practice Committee, Faulx AL, Kothari S, Acosta RD, Agrawal D, Bruining DH, Chandrasekhara V, Eloubeidi MA, Fanelli RD, Gurudu SR, Khashab MA, Lightdale JR, Muthusamy VR, Shaukat A, Qumseya BJ, Wang A, Wani SB, Yang J, DeWitt JM. The role of endoscopy in subepithelial lesions of the GI tract. Gastrointest Endosc. 2017;85(6):1117-1132.
https://doi.org/10.1016/j.gie.2017.02.022
Polkowski M. Endoscopic ultrasound and endoscopic ultrasound- guided fine-needle biopsy for the diagnosis of malignant submucosal tumors. Endoscopy 2005;37(7):635-45.
https://doi.org/10.1055/s-2005-861422
Nishida T, Blay JY, Hirota S, Kitagawa Y, Kang YK. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer. 2016;19(1):3-14.
https://doi.org/10.1007/s10120-015-0526-8
Trindade AJ, Benias PC, Alshelleh M, Bazarbashi AN, Tharian B, Inamdar S, Sharma N, Zelt C, Korrapati P, Barakat M, Sejpal DV, Ryou M. Fine-needle biopsy is superior to fine-needle aspiration of suspected gastrointestinal stromal tumors: a large multicenter study. Endosc Int Open. 2019;7(7):E931-E936.
https://doi.org/10.1055/a-0953-1640
Kim SY, Shim KN, Lee JH, Lim JY, Kim TO, Choe AR, Tae CH, Jung HK, Moon CM, Kim SE, Jung SA. Comparison of the Diagnostic Ability of Endoscopic Ultrasonography and Abdominopelvic Computed Tomography in the Diagnosis of Gastric Subepithelial Tumors. Clin Endosc. 2019;52(6):565-573.
https://doi.org/10.5946/ce.2019.019
Sabik JF, Rice TW, Goldblum JR, Koka A, Kirby TJ, Medendorp SV, Adelstein DJ. Superficial esophageal carcinoma. Ann Thorac Surg. 1995;60(4):896-901; discussion 902.
https://doi.org/10.1016/0003-4975(95)00542-s
Hulshoff JB, Mul VEM, de Boer HEM, Noordzij W, Korteweg T, van Dullemen HM, Nagengast WB, Oppedijk V, Pierie JPEN, Plukker JTM. Impact of Endoscopic Ultrasonography on 18F-FDG-PET/CT Upfront Towards Patient Specific Esophageal Cancer Treatment. Ann Surg Oncol. 2017;24(7):1828-1834.
https://doi.org/10.1245/s10434-017-5835-1
Foley KG, Morgan C, Roberts SA, Crosby T. Impact of Positron Emission Tomography and Endoscopic Ultrasound Length of Disease Difference on Treatment Planning in Patients with Oesophageal Cancer. Clin Oncol (R Coll Radiol). 2017;29(11):760-766.
https://doi.org/10.1016/j.clon.2017.07.014
Foley K, Findlay J, Goh V. Novel imaging techniques in staging oesophageal cancer. Best Pract Res Clin Gastroenterol. 2018;36-37:17-25.
https://doi.org/10.1016/j.bpg.2018.11.009
Morgan MA, Twine CP, Lewis WG, Lambe R, Oliphant HE, Robinson M, Crosby TD, Roberts SA. Prognostic significance of failure to cross esophageal tumors by endoluminal ultrasound. Dis Esophagus. 2008;21(6):508-13. https://doi.org/10.1111/j.1442-2050.2008.00809.x
Sitarz R, Skierucha M, Mielko J, Offerhaus GJA, Maciejewski R, Polkowski WP. Gastric cancer: epidemiology, prevention, classification, and treatment. Cancer Manag Res. 2018;10:239-248.
https://doi.org/10.2147/CMAR.S149619
Mocellin S, Pasquali S. Diagnostic accuracy of endoscopic ultrasonography (EUS) for the preoperative locoregional staging of primary gastric cancer. Cochrane Database Syst Rev. 2015;2015(2):CD009944.
https://doi.org/10.1002/14651858.CD009944.pub2
Cimavilla Román M, de la Serna Higuera C, Loza Vargas LA, Benito Fernández C, Barrio Andrés J, Madrigal Rubiales B, Fernández Pérez G, Pérez-Miranda M. Endoscopic ultrasound versus multidetector computed tomography in preoperative gastric cancer staging. Rev Esp Enferm Dig. 2017;109(11):761-767.
https://doi.org/10.17235/reed.2017.4638/2016
Banerjee AK, Longcroft-Wheaton G, Beable R, Conti J, Khan J, Bhandari P. The role of imaging and biopsy in the management and staging of large non-pedunculated rectal polyps. Expert Rev Gastroenterol Hepatol. 2018;12(8):749-755.
https://doi.org/10.1080/17474124.2018.1492377
Fuchsjäger MH, Maier AG, Schima W, Zebedin E, Herbst F, Mittlböck M, Wrba F, Lechner GL. Comparison of transrectal sonography and double-contrast MR imaging when staging rectal cancer. AJR Am J Roentgenol. 2003;181(2):421-7.
https://doi.org/10.2214/ajr.181.2.1810421
Puli SR, Bechtold ML, Reddy JB, Choudhary A, Antillon MR, Brugge WR. How good is endoscopic ultrasound in differentiating various T stages of rectal cancer? Meta-analysis and systematic review. Ann Surg Oncol. 2009;16(2):254-65.
https://doi.org/10.1245/s10434-008-0231-5
Beets-Tan RGH, Lambregts DMJ, Maas M, Bipat S, Barbaro B, Curvo-Semedo L, Fenlon HM, Gollub MJ, Gourtsoyianni S, Halligan S, Hoeffel C, Kim SH, Laghi A, Maier A, Rafaelsen SR, Stoker J, Taylor SA, Torkzad MR, Blomqvist L. Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol. 2018;28(4):1465-1475.
https://doi.org/10.1007/s00330-017-5026-2
Worrell S, Horvath K, Blakemore T, Flum D. Endorectal ultrasound detection of focal carcinoma within rectal adenomas. Am J Surg. 2004;187(5):625-9; discussion 629. https://doi.org/10.1016/j.amjsurg.2004.01.005
Waage JE, Leh S, Røsler C, Pfeffer F, Bach SP, Havre RF, Haldorsen IS, Ødegaard S, Baatrup G. Endorectal ultrasonography, strain elastography and MRI differentiation of rectal adenomas and adenocarcinomas. Colorectal Dis. 2015;17(2):124-31.
https://doi.org/10.1111/codi.12845
Marone P, de Bellis M, D’Angelo V, Delrio P, Passananti V, Di Girolamo E, Rossi GB, Rega D, Tracey MC, Tempesta AM. Role of endoscopic ultrasonography in the loco-regional staging of patients with rectal cancer. World J Gastrointest Endosc. 2015;7(7):688-701.
https://doi.org/10.4253/wjge.v7.i7.688
Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging--a meta-analysis. Radiology. 2004;232(3):773-83.
https://doi.org/10.1148/radiol.2323031368
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Garrido-Laguna I, Grem JL, Gunn A, Hoffe S, Hubbard J, Hunt S, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Miller ED, Mulcahy MF, Nurkin S, Overman MJ, Parikh A, Patel H, Pedersen K, Saltz L, Schneider C, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Johnson-Chilla A, Gurski LA. NCCN Guidelines Insights: Rectal Cancer, Version 6.2020. J Natl Compr Canc Netw. 2020 Jul;18(7):806-815.
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Engstrom PF, Grem JL, Grothey A, Hochster HS, Hoffe S, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Mulcahy MF, Murphy JD, Nurkin S, Saltz L, Sharma S, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Wuthrick E, Gregory KM, Gurski L, Freedman-Cass DA. Rectal Cancer, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2018;16(7):874-901.
https://doi.org/10.6004/jnccn.2018.0061
Bhutani MS, Koduru P, Joshi V, Saxena P, Suzuki R, Irisawa A, Yamao K. The role of endoscopic ultrasound in pancreatic cancer screening. Endosc Ultrasound. 2016;5(1):8-16. https://doi.org/10.4103/2303-9027.175876
Uehara H, Ikezawa K, Kawada N, Fukutake N, Katayama K, Takakura R, Takano Y, Ishikawa O, Takenaka A. Diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration for suspected pancreatic malignancy in relation to the size of lesions. J Gastroenterol Hepatol. 2011;26(8):1256-61.
https://doi.org/10.1111/j.1440-1746.2011.06747.x
Hewitt MJ, McPhail MJ, Possamai L, Dhar A, Vlavianos P, Monahan KJ. EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. Gastrointest Endosc. 2012;75(2):319-31.
https://doi.org/10.1016/j.gie.2011.08.049
Ayres LR, Kmiotek EK, Lam E, Telford JJ. A Comparison of Endoscopic Ultrasound-Guided Fine-Needle Aspiration and Fine-Needle Biopsy in the Diagnosis of Solid Pancreatic Lesions. Can J Gastroenterol Hepatol. 2018;2018:1415062.
https://doi.org/10.1155/2018/1415062
Mosquera-Klinger G, Carvajal JJ, Echeverri C, Pérez JC, Cardona R, Valencia-Maturana J, Sánchez-Garrido H. Rendimiento diagnóstico de las punciones de lesiones biliopancreáticas guiadas por ultrasonido endoscopio con patólogo en sala. En prensa.
Goldberg SN, Mallery S, Gazelle GS, Brugge WR. EUS-guided radiofrequency ablation in the pancreas: results in a porcine model. Gastrointest Endosc. 1999;50(3):392-401. https://doi.org/10.1053/ge.1999.v50.98847
Wu Y, Tang Z, Fang H, Gao S, Chen J, Wang Y, Yan H. High operative risk of cool-tip radiofrequency ablation for unresectable pancreatic head cancer. J Surg Oncol. 2006;94(5):392-5.
https://doi.org/10.1002/jso.20580
Spiliotis JD, Datsis AC, Michalopoulos NV, Kekelos SP, Vaxevanidou A, Rogdakis AG, Christopoulou AN. Radiofrequency ablation combined with palliative surgery may prolong survival of patients with advanced cancer of the pancreas. Langenbecks Arch Surg. 2007;392(1):55-60. https://doi.org/10.1007/s00423-006-0098-5
Elias D, Baton O, Sideris L, Lasser P, Pocard M. Necrotizing pancreatitis after radiofrequency destruction of pancreatic tumours. Eur J Surg Oncol. 2004;30(1):85-7.
https://doi.org/10.1016/j.ejso.2003.10.013
Lakhtakia S, Ramchandani M, Galasso D, Gupta R, Venugopal S, Kalpala R, Reddy DN. EUS-guided radiofrequency ablation for management of pancreatic insulinoma by using a novel needle electrode (with videos). Gastrointest Endosc. 2016;83(1):234-9.
https://doi.org/10.1016/j.gie.2015.08.085
Waung JA, Todd JF, Keane MG, Pereira SP. Successful management of a sporadic pancreatic insulinoma by endoscopic ultrasound-guided radiofrequency ablation. Endoscopy. 2016;48 Suppl 1:E144-5.
https://doi.org/10.1055/s-0042-104650
Limmer S, Huppert PE, Juette V, Lenhart A, Welte M, Wietholtz H. Radiofrequency ablation of solitary pancreatic insulinoma in a patient with episodes of severe hypoglycemia. Eur J Gastroenterol Hepatol. 2009;21(9):1097-101. https://doi.org/10.1097/MEG.0b013e328323d70e
Pai M, Habib N, Senturk H, Lakhtakia S, Reddy N, Cicinnati VR, Kaba I, Beckebaum S, Drymousis P, Kahaleh M, Brugge W. Endoscopic ultrasound guided radiofrequency ablation, for pancreatic cystic neoplasms and neuroendocrine tumors. World J Gastrointest Surg. 2015;7(4):52-9.
https://doi.org/10.4240/wjgs.v7.i4.52
Rossi S, Viera FT, Ghittoni G, Cobianchi L, Rosa LL, Siciliani L, Bortolotto C, Veronese L, Vercelli A, Gallotti A, Ravetta V. Radiofrequency ablation of pancreatic neuroendocrine tumors: a pilot study of feasibility, efficacy, and safety. Pancreas. 2014;43(6):938-45.
https://doi.org/10.1097/MPA.0000000000000133
Mosquera-Klinger G, Carvajal JJ. Insulinoma pancreático sintomático: Tratamiento ablativo mediante etanolización guiado por ultrasonido endoscópico. Rev Esp Enf Dig. En prensa, 2020.
https://doi.org/10.17235/reed.2020.7109/2020
Civardi G, Vallisa D, Bertè R, Giorgio A, Filice C, Caremani M, Caturelli E, Pompili M, De Sio I, Buscarini E, Cavanna L. Ultrasound-guided fine needle biopsy of the spleen: high clinical efficacy and low risk in a multicenter Italian study. Am J Hematol. 2001;67(2):93-9.
https://doi.org/10.1002/ajh.1085
Quinn SF, vanSonnenberg E, Casola G, Wittich GR, Neff CC. Interventional radiology in the spleen. Radiology. 1986;161(2):289-91.
https://doi.org/10.1148/radiology.161.2.3763890
Werner T, Koch J, Frenzel C, Lohse AW, Denzer UW. Effectiveness and safety of minilaparoscopy-guided spleen biopsy: a
retrospective series of 57 cases. Surg Endosc. 2012;26(9):2416-22.
https://doi.org/10.1007/s00464-012-2190-y
Söderström N. How to use cytodiagnostic spleen puncture. Acta Med Scand. 1976;199(1-2):1-5.
https://doi.org/10.1111/j.0954-6820.1976.tb06683.x
Solbiati L, Bossi MC, Bellotti E, Ravetto C, Montali G. Focal lesions in the spleen: sonographic patterns and guided biopsy. AJR Am J Roentgenol. 1983;140(1):59-65. https://doi.org/10.2214/ajr.140.1.59
Silverman JF, Geisinger KR, Raab SS, Stanley MW. Fine needle aspiration biopsy of the spleen in the evaluation of neoplastic disorders. Acta Cytol. 1993;37(2):158-62.
Zeppa P, Vetrani A, Luciano L, Fulciniti F, Troncone G, Rotoli B, Palombini L. Fine needle aspiration biopsy of the spleen. A useful procedure in the diagnosis of splenomegaly. Acta Cytol. 1994;38(3):299-309.
Mosquera-Klinger G, de la Serna Higuera C, Bazaga S, García-Alonso FJ, Sánchez Ocaña R, Antolín Melero B, de Benito Sanz M, Madrigal B, Torres Á, Pérez-Miranda M. Endoscopic ultrasound-guided fine-needle aspiration for splenomegaly and focal splenic lesion: is it safe, effective and necessary? Rev Esp Enferm Dig. 2020;112(5):355-359.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |
















