EndoFLIP: una nueva tecnología
DOI:
https://doi.org/10.22516/25007440.741Palabras clave:
EndoFLIP, Acalasia, Impedancia, Motilidad, Sonda de imagen luminal funcionalResumen
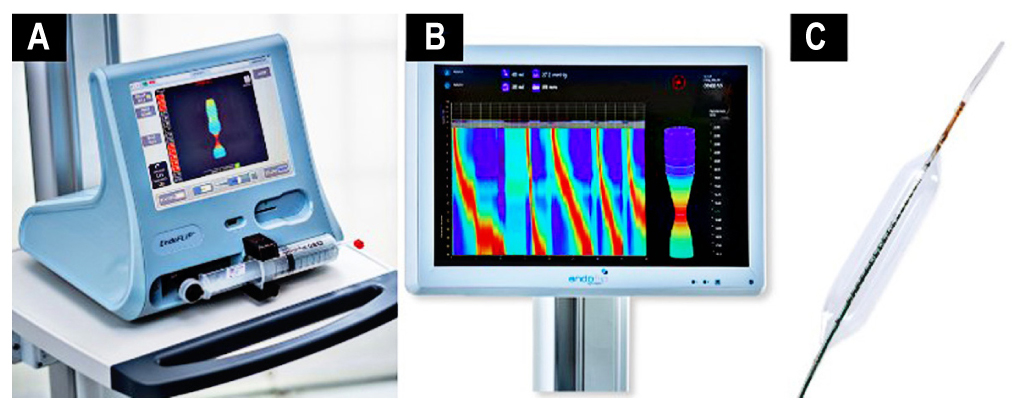
Mediante la distensión de un balón con líquido conductor, la sonda de imagen luminal funcional endoluminal (EndoFLIP) evalúa las propiedades biomecánicas como la distensibilidad, volumen, presión e inclusive diámetros de regiones esfinterianas como la unión gastroesofágica, píloro y ano. La mayor evidencia en la utilidad clínica de la EndoFLIP está en los trastornos de motilidad esofágica, principalmente para identificar acalasia cuando la manometría esofágica de alta resolución y otras imágenes no logran diagnosticarla e inclusive, mediante el programa de FLIP 2.0, caracteriza la acalasia en subtipos a partir de patrones de motilidad del esófago distal en respuesta a la distensión. Se ha demostrado recientemente que la EndoFLIP tiene un rol diagnóstico, pronóstico o terapéutico en otras patologías como la esofagitis eosinofílica, reflujo gastroesofágico, gastroparesia, durante la fundoplicatura y dilatación esofágica.
Descargas
Referencias bibliográficas
Dorsey YC, Posner S, Patel A. Esophageal Functional Lumen Imaging Probe (FLIP): How Can FLIP Enhance Your Clinical Practice? Dig Dis Sci. 2020;65(9):2473-2482. https://doi.org/10.1007/s10620-020-06443-8
Donnan EN, Pandolfino JE. EndoFLIP in the Esophagus: Assessing Sphincter Function, Wall Stiffness, and Motility to Guide Treatment. Gastroenterol Clin North Am. 2020;49(3):427-435. https://doi.org/10.1016/j.gtc.2020.04.002
Savarino E, di Pietro M, Bredenoord AJ, Carlson DA, Clarke JO, Khan A, et al. Use of the Functional Lumen Imaging Probe in Clinical Esophagology. Am J Gastroenterol. 2020;115(11):1786-1796. https://doi.org/10.14309/ajg.0000000000000773
Hirano I, Pandolfino JE, Boeckxstaens GE. Functional Lumen Imaging Probe for the Management of Esophageal Disorders: Expert Review From the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15(3):325-334. https://doi.org/10.1016/j.cgh.2016.10.022
Donnan EN, Pandolfino JE. Applying the Functional Luminal Imaging Probe to Esophageal Disorders. Curr Gastroenterol Rep. 2020;22(3):10. https://doi.org/10.1007/s11894-020-0749-7
Clarke JO, Ahuja NK, Fernandez-Becker NQ, Gregersen H, Kamal AN, Khan A, et al. The functional lumen imaging probe in gastrointestinal disorders: the past, present, and future. Ann N Y Acad Sci. 2020;1482(1):16-25. https://doi.org/10.1111/nyas.14463
McMahon BP, Frøkjaer JB, Liao D, Kunwald P, Drewes AM, Gregersen H. A new technique for evaluating sphincter function in visceral organs: application of the functional lumen imaging probe (FLIP) for the evaluation of the oesophago-gastric junction. Physiol Meas. 2005;26(5):823-36. https://doi.org/10.1088/0967-3334/26/5/019
McMahon BP, Frøkjaer JB, Drewes AM, Gregersen H. A new measurement of oesophago-gastric junction competence. Neurogastroenterol Motil. 2004;16(5):543-6. https://doi.org/10.1111/j.1365-2982.2004.00540.x
Bianca A, Schindler V, Schnurre L, Murray F, Runggaldier D, Gyawali CP, et al. Endoscope presence during endoluminal functional lumen imaging probe (FLIP) influences FLIP metrics in the evaluation of esophageal dysmotility. Neurogastroenterol Motil. 2020;32(6):e13823. https://doi.org/10.1111/nmo.13823
Valdovinos LR, Vela MI. Utilidad de la sonda de imagen luminal funcional (Endoflip) en las enfermedades esofágicas. Acta Gastroenterol Latinoam 2020,50:79-87
Carlson DA, Kahrilas PJ, Lin Z, Hirano I, Gonsalves N, Listernick Z, et al. Evaluation of Esophageal Motility Utilizing the Functional Lumen Imaging Probe. Am J Gastroenterol. 2016;111(12):1726-1735.
https://doi.org/10.1038/ajg.2016.454
Carlson DA, Lin Z, Rogers MC, Lin CY, Kahrilas PJ, Pandolfino JE. Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil. 2015;27(7):981-9. https://doi.org/10.1111/nmo.12572
Carlson DA, Kou W, Lin Z, Hinchcliff M, Thakrar A, Falmagne S, et al. Normal Values of Esophageal Distensibility and Distension-Induced Contractility Measured by Functional Luminal Imaging Probe Panometry. Clin Gastroenterol Hepatol. 2019;17(4):674-681.e1. https://doi.org/10.1016/j.cgh.2018.07.042
Gyawali CP, Carlson DA, Chen JW, Patel A, Wong RJ, Yadlapati RH. ACG Clinical Guidelines: Clinical Use of Esophageal Physiologic Testing. Am J Gastroenterol. 2020;115(9):1412-1428. https://doi.org/10.14309/ajg.0000000000000734
Desprez C, Roman S, Leroi AM, Gourcerol G. The use of impedance planimetry (Endoscopic Functional Lumen Imaging Probe, EndoFLIP® ) in the gastrointestinal tract: A systematic review. Neurogastroenterol Motil. 2020;32(9):e13980. https://doi.org/10.1111/nmo.13980
Patel DA, Lappas BM, Vaezi MF. An Overview of Achalasia and Its Subtypes. Gastroenterol Hepatol (N Y). 2017;13(7):411-421.
Jung HK, Hong SJ, Lee OY, Pandolfino J, Park H, Miwa H, et al. 2019 Seoul Consensus on Esophageal Achalasia Guidelines. J Neurogastroenterol Motil. 2020;26(2):180-203. https://doi.org/10.5056/jnm20014
Oude Nijhuis RAB, Zaninotto G, Roman S, Boeckxstaens GE, Fockens P, Langendam MW, et al. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United European Gastroenterol J. 2020;8(1):13-33. https://doi.org/10.1177/2050640620903213
Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021;33(1):e14058. https://doi.org/10.1111/nmo.14058
Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2020;115(9):1393-1411. https://doi.org/10.14309/ajg.0000000000000731
Massey BT. Clinical Functional Lumen Imaging Probe Testing in Esophageal Disorders: A Need for Better Quality Evidence. Am J Gastroenterol. 2020;115(11):1799-1801. https://doi.org/10.14309/ajg.0000000000000974
Rooney KP, Baumann AJ, Donnan E, Kou W, Triggs JR, Prescott J, et al. Esophagogastric Junction Opening Parameters Are Consistently Abnormal in Untreated Achalasia. Clin Gastroenterol Hepatol. 2021;19(5):1058-1060.e1. https://doi.org/10.1016/j.cgh.2020.03.069
Carlson DA, Lin Z, Kahrilas PJ, Sternbach J, Donnan EN, Friesen L, et al. The Functional Lumen Imaging Probe Detects Esophageal Contractility Not Observed With Manometry in Patients With Achalasia. Gastroenterology. 2015;149(7):1742-51. https://doi.org/10.1053/j.gastro.2015.08.005
Carlson DA, Kou W, Rooney KP, Baumann AJ, Donnan E, Triggs JR, et al. Achalasia subtypes can be identified with functional luminal imaging probe (FLIP) panometry using a supervised machine learning process. Neurogastroenterol Motil. 2021;33(3):e13932. https://doi.org/10.1111/nmo.13932
Sanagapalli S, Roman S, Hastier A, Leong RW, Patel K, Raeburn A, et al. Achalasia diagnosed despite normal integrated relaxation pressure responds favorably to therapy. Neurogastroenterol Motil. 2019;31(6):e13586. https://doi.org/10.1111/nmo.13586
Ang D, Hollenstein M, Misselwitz B, Knowles K, Wright J, Tucker E, et al. Rapid Drink Challenge in high-resolution manometry: an adjunctive test for detection of esophageal motility disorders. Neurogastroenterol Motil. 2017;29(1). https://doi.org/10.1111/nmo.12902
Horton A, Jawitz N, Patel A. The Clinical Utility of Provocative Maneuvers at Esophageal High-resolution Manometry (HRM). J Clin Gastroenterol. 2021;55(2):95-102. https://doi.org/10.1097/MCG.0000000000001466
Khashab MA, Vela MF, Thosani N, Agrawal D, Buxbaum JL, Abbas Fehmi SM, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020;91(2):213-227.e6. https://doi.org/10.1016/j.gie.2019.04.231
Carlson DA, Hirano I. Application of the Functional Lumen Imaging Probe to Esophageal Disorders. Curr Treat Options Gastroenterol. 2017;15(1):10-25. https://doi.org/10.1007/s11938-017-0116-4
Campagna RAJ, Carlson DA, Hungness ES, Holmstrom AL, Pandolfino JE, Soper NJ, et al. Intraoperative assessment of esophageal motility using FLIP during myotomy for achalasia. Surg Endosc. 2020;34(6):2593-2600. https://doi.org/10.1007/s00464-019-07028-x
Attaar M, Su B, Wong HJ, Kuchta K, Denham W, Haggerty SP, et al. Intraoperative impedance planimetry (EndoFLIP™) results and development of esophagitis in patients undergoing peroral endoscopic myotomy (POEM). Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-07876-y
Su B, Dunst C, Gould J, Jobe B, Severson P, Newhams K, et al. Experience-based expert consensus on the intra-operative usage of the Endoflip impedance planimetry system. Surg Endosc. 2021;35(6):2731-2742. https://doi.org/10.1007/s00464-020-07704-3
Carlson DA, Kathpalia P, Craft J, Tye M, Lin Z, Kahrilas PJ, et al. The relationship between esophageal acid exposure and the esophageal response to volumetric distention. Neurogastroenterol Motil. 2018;30(3):10.1111/nmo.13240. https://doi.org/10.1111/nmo.13240
Lee JM, Yoo IK, Kim E, Hong SP, Cho JY. The Usefulness of the Measurement of Esophagogastric Junction Distensibility by EndoFLIP in the Diagnosis of Gastroesophageal Reflux Disease. Gut Liver. 2020. https://doi.org/10.5009/gnl20117
Lottrup C, McMahon BP, Ejstrud P, Ostapiuk MA, Funch-Jensen P, Drewes AM. Esophagogastric junction distensibility in hiatus hernia. Dis Esophagus. 2016;29(5):463-71. https://doi.org/10.1111/dote.12344
Zikos TA, Triadafilopoulos G, Clarke JO. Esophagogastric Junction Outflow Obstruction: Current Approach to Diagnosis and Management. Curr Gastroenterol Rep. 2020;22(2):9. https://doi.org/10.1007/s11894-020-0743-0
Reddy AT, Shimpi RA, Parish A, Niedzwiecki D, Leiman DA. Predictors of Abnormal Functional Luminal Impedance Planimetry Findings in Non-mechanical Esophagogastric Junction Outflow Obstruction. Dig Dis Sci. 2020. https://doi.org/10.1007/s10620-020-06726-0
Triggs JR, Carlson DA, Beveridge C, Kou W, Kahrilas PJ, Pandolfino JE. Functional Luminal Imaging Probe Panometry Identifies Achalasia-Type Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2020;18(10):2209-2217. https://doi.org/10.1016/j.cgh.2019.11.037
Sullivan A, Temperley L, Ruban A. Pathophysiology, Aetiology and Treatment of Gastroparesis. Dig Dis Sci. 2020;65(6):1615-1631. https://doi.org/10.1007/s10620-020-06287-2
Usai-Satta P, Bellini M, Morelli O, Geri F, Lai M, Bassotti G. Gastroparesis: New insights into an old disease. World J Gastroenterol. 2020;26(19):2333-2348. https://doi.org/10.3748/wjg.v26.i19.2333
Saadi M, Yu D, Malik Z, Parkman HP, Schey R. Pyloric sphincter characteristics using EndoFLIP® in gastroparesis. Rev Gastroenterol Mex. 2018;83(4):375-384. https://doi.org/10.1016/j.rgmx.2018.02.013
Desprez C, Melchior C, Wuestenberghs F, Zalar A, Jacques J, Leroi AM, et al. Pyloric distensibility measurement predicts symptomatic response to intrapyloric botulinum toxin injection. Gastrointest Endosc. 2019;90(5):754-760.e1. https://doi.org/10.1016/j.gie.2019.04.228
Tao J, Patel V, Mekaroonkamol P, Luo H, Li B, Guan Q, et al. Technical Aspects of Peroral Endoscopic Pyloromyotomy. Gastrointest Endosc Clin N Am. 2019;29(1):117-126. https://doi.org/10.1016/j.giec.2018.08.012
Vosoughi K, Ichkhanian Y, Jacques J, Aadam AA, Benias PC, Law R, et al. Role of endoscopic functional luminal imaging probe in predicting the outcome of gastric peroral endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2020 Jun;91(6):1289-1299. https://doi.org/10.1016/j.gie.2020.01.044
Jehangir A, Malik Z, Petrov RV, Parkman HP. EndoFLIP and Pyloric Dilation for Gastroparesis Symptoms Refractory to Pyloromyotomy/Pyloroplasty. Dig Dis Sci. 2020. https://doi.org/10.1007/s10620-020-06510-0
Ilczyszyn A, Botha AJ. Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus. 2014;27(7):637-44. https://doi.org/10.1111/dote.12130
Kim MP, Meisenbach LM, Chan EY. Tailored Fundoplication With Endoluminal Functional Lumen Imaging Probe Allows for Successful Minimally Invasive Hiatal Hernia Repair. Surg Laparosc Endosc Percutan Tech. 2018;28(3):178-182. https://doi.org/10.1097/SLE.0000000000000527
DeHaan RK, Davila D, Frelich MJ, Gould JC. Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc. 2017;31(1):193-198. https://doi.org/10.1007/s00464-016-4956-0
Su B, Novak S, Callahan ZM, Kuchta K, Carbray J, Ujiki MB. Using impedance planimetry (EndoFLIP™) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc. 2020;34(4):1761-1768. https://doi.org/10.1007/s00464-019-06925-5
Yu JX, Baker JR, Watts L, Varban OA, Chen JW, Rubenstein JH, et al. Functional Lumen Imaging Probe Is Useful for the Quantification of Gastric Sleeve Stenosis and Prediction of Response to Endoscopic Dilation: a Pilot Study. Obes Surg. 2020;30(2):786-789. https://doi.org/10.1007/s11695-019-04105-x
Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128(1):3-20.e6; quiz 21-2. https://doi.org/10.1016/j.jaci.2011.02.040
Schoepfer AM, Safroneeva E, Bussmann C, Kuchen T, Portmann S, Simon HU, et al. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time-dependent manner. Gastroenterology. 2013;145(6):1230-6.e1-2. https://doi.org/10.1053/j.gastro.2013.08.015
Hirano I, Aceves SS. Clinical implications and pathogenesis of esophageal remodeling in eosinophilic esophagitis. Gastroenterol Clin North Am. 2014;43(2):297-316. https://doi.org/10.1016/j.gtc.2014.02.015
Chen JW, Pandolfino JE, Lin Z, Ciolino JD, Gonsalves N, Kahrilas PJ, et al. Severity of endoscopically identified esophageal rings correlates with reduced esophageal distensibility in eosinophilic esophagitis. Endoscopy. 2016;48(9):794-801. https://doi.org/10.1055/s-0042-107340
Carlson DA, Hirano I, Zalewski A, Gonsalves N, Lin Z, Pandolfino JE. Improvement in Esophageal Distensibility in Response to Medical and Diet Therapy in Eosinophilic Esophagitis. Clin Transl Gastroenterol. 2017;8(10):e119. https://doi.org/10.1038/ctg.2017.47
Kappelle WF, Bogte A, Siersema PD. Hydraulic dilation with a shape-measuring balloon in idiopathic achalasia: a feasibility study. Endoscopy. 2015;47(11):1028-34. https://doi.org/10.1055/s-0034-1392481
Baumann AJ, Carlson DA. EsoFLIP for esophageal dilation: proposed advantages. Curr Opin Gastroenterol. 2020;36(4):329-335. https://doi.org/10.1097/MOG.0000000000000639
O’Dea J, Siersema PD. Esophageal dilation with integrated balloon imaging: initial evaluation in a porcine model. Therap Adv Gastroenterol. 2013;6(2):109-14. https://doi.org/10.1177/1756283X12467566
Nicodème F, Hirano I, Chen J, Robinson K, Lin Z, Xiao Y, et al. Esophageal distensibility as a measure of disease severity in patients with eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2013;11(9):1101-1107.e1. https://doi.org/10.1016/j.cgh.2013.03.020
Teitelbaum EN, Boris L, Arafat FO, Nicodème F, Lin Z, Kahrilas PJ, et al. Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc. 2013;27(12):4547-55. https://doi.org/10.1007/s00464-013-3121-2
Wu PI, Szczesniak MM, Craig PI, Choo L, Engelman J, Terkasher B, et al. Novel Intra-Procedural Distensibility Measurement Accurately Predicts Immediate Outcome of Pneumatic Dilatation for Idiopathic Achalasia. Am J Gastroenterol. 2018;113(2):205-212. https://doi.org/10.1038/ajg.2017.411
Sloan JA, Triggs JR, Pandolfino JE, Dbouk M, Brewer Gutierrez OI, El Zein M, et al. Treatment experience with a novel 30-mm hydrostatic balloon in esophageal dysmotility: a multicenter retrospective analysis. Gastrointest Endosc. 2020;92(6):1251-1257. https://doi.org/10.1016/j.gie.2020.04.076
Schnurre L, Murray FR, Schindler V, Runggaldier D, Fischbach L, Bordier V, et al. Short-term outcome after singular hydraulic EsoFLIP dilation in patients with achalasia: A feasibility study. Neurogastroenterol Motil. 2020;32(9):e13864. https://doi.org/10.1111/nmo.13864
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |
















