Leukocytoclastic vasculitis as a rare extraintestinal dermatologic manifestation of inflammatory bowel disease associated with Clostridium difficile: Case repor
DOI:
https://doi.org/10.22516/25007440.500Keywords:
Leukocytoclastic vasculitis, clostridum difficile, ulcerative colitis, inflammatory bowel disease, Extraintestinal manifestationsAbstract
Leukocytoclastic vasculitis is defined as the damage and inflammation of the vascular walls. The term refers
to vasculitis of the small vessels that anatomopathologically present leukocytoclasia and it can be seen as
an extra-intestinal manifestation of inflammatory bowel disease. In ulcerative colitis, it occurs less frequently
due to immune complexes produced in the intestinal mucosa by exposure of the submucosal lymphoid tissue
to fecal antigens, which could precipitate in the walls of the small vessels. This condition can be associated
with Clostridium difficile, which is a gram-positive, sporulated, strict anaerobic bacillus, normally found in the
environment. It causes colitis that manifests as a diarrheal disease following the ingestion of antibiotics that
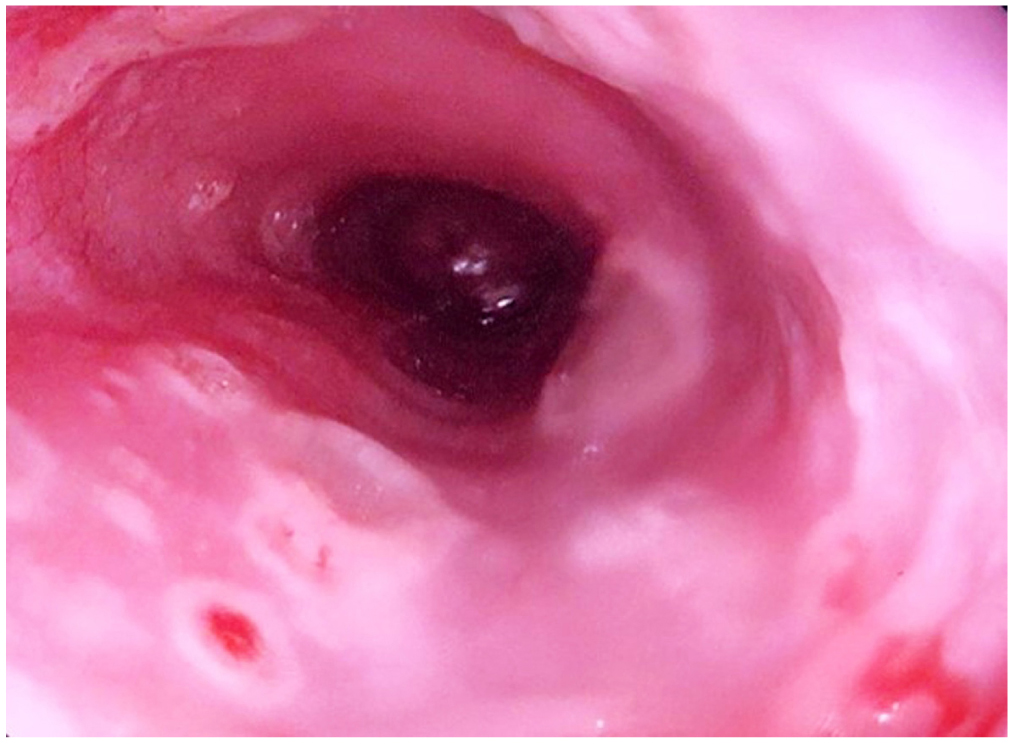
alter the common bacterial flora of this organ. This is the case report of a 36-year-old patient with liquid diarrhea with mucus and scarce bleeding. Endoscopic and anatomopathological studies were performed, finding ulcerative colitis with positive coproparasite for Clostridium difficile antigen. The patient was hospitalized, and during his stay, he presented with petechiae and necrotic skin lesions on the fourth finger of the left hand. Skin biopsy showed small vessel vasculitis. This article is a practical review of the pathophysiology, histology, treatment, and diagnosis of a rare dermatologic extraintestinal manifestation, namely, leukocytoclastic vasculitis, in patients with C. difficile–associated ulcerative colitis.
Downloads
References
Casano VJ, Fernández Carballido C, Ibero Díaz I, Contreras Blasco MA. Vasculitis Leucocitoclásticas. En: Román JA, Rosas JC, Castellano JA (editores). Enfermedades Reumáticas. Sociedad Valenciana de Reumatología; 2008. p. 289-299.
Hong JS, Jin SP, Choi M, Lee KL, Lee JH, Cho S. Annular leukocytoclastic vasculitis in a patient with ulcerative colitis. Ann Dermatol. 2011;23(Suppl 3):S338-40. https://doi.org/10.5021/ad.2011.23.S3.S338
Butts GT, Bishop PR, Wyatt JP, Nowicki MJ. Leukocytoclastic vasculitis in an adolescent with ulcerative colitis: Report of a case and review of the literature. SAGE Open Med Case Rep. 2014;2:2050313X14547609. https://doi.org/10.1177/2050313X14547609
Piche T, Vanbiervliet G, Pipau FG, Dainese R, Hébuterne X, Rampal P, Collins SM. Low risk of irritable bowel syndrome after Clostridium difficile infection. Can J Gastroenterol. 2007;21(11):727-31. https://doi.org/10.1155/2007/262478
Vieira Teixeira F, Saad Hosne R, Sobrado CW.Management of ulcerative colitis: a clinical update. 4, 2015, J Coloproctol. 2015;35(04):230-7. https://doi.org/10.1016/j.jcol.2015.08.006
Davis SC, Robinson BL, Vess J, Lebel JS. Primary care management of ulcerative colitis. Nurse Pract. 2018;43(1):11-19. https://doi.org/10.1097/01.NPR.0000527565.05934.14
Gota CE, Calabrese LH. Diagnosis and treatment of cutaneous leukocytoclastic vasculitis. Int J Clin Rheumatol. 2013;8(1):49-60. https://doi.org/10.2217/ijr.12.79
Liste Rodríguez S, Chamizo Cabrera MG, Paz Enrique LE; Hernández Alfonso EA. Vasculitis leucocitoclástica. Revista Cubana de Medicina General Integral. 2013;30(4):415-420.
Langan RC, Gotsch PB, Krafczyk MA, Skillinge DD. Ulcerative colitis: diagnosis and treatment. Am Fam Physician. 2007;76(9):1323-30.
Baigrie D, Bansal P, Goyal A, Crane JS. Leukocytoclastic Vasculitis. 2020 Aug 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
Cerezo Ruiz A, Lenzano Grande F, Pérez De Luque DJ, Domínguez Jiménez JL, Rodríguez-Mancheño AL, Cortés Rodríguez B, Serrano Muñoz A. Vasculitis leucocitoclástica asociada a colitis ulcerosa. Gastroenterol Hepatol. 2010;33(9):682-3. https://doi.org/10.1016/j.gastrohep.2010.03.002
Callen JP. Severe cutaneous vasculitis complicating ulcerative colitis. Arch Dermatol. 1979;115(2):226-7.
Einhorn J, Levis JT. Dermatologic Diagnosis: Leukocytoclastic Vasculitis. Perm J. 2015;19(3):77-8. https://doi.org/10.7812/TPP/15-001
Agrawal D, Rukkannagari S, Kethu S. Pathogenesis and clinical approach to extraintestinal manifestations of inflammatory bowel disease. Minerva Gastroenterol Dietol. 2007;53(3):233-48.
Leukocytoclastic Vasculitis [internet]. American Osteopathic College of Dermatology [citado el 9 de septiembre de 2019]. Disponible en: https://www.aocd.org/page/LeukocytoclasticVas
Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am J Gastroenterol. 2019;114(3):384-413. https://doi.org/10.14309/ajg.0000000000000152
Plaza Santos R, Jaquotot Herranz M, Froilán Torres C, Poza Cordón J, Casado Verrier B, de Tena Díaz-Agero FL, Vázquez López P, Suárez de Parga JM. Vasculitis leucocitoclástica asociada a enfermedad de Crohn. Gastroenterol Hepatol. 2010;33(6):433-5. https://doi.org/10.1016/j.gastrohep.2009.07.004
Rodríguez-Pardo D, Mirelis B, Navarro F. Infecciones producidas por Clostridium difficile. Enferm Infecc Microbiol Clin. 2013;31(4):254-63. https://doi.org/10.1016/j.eimc.2012.12.010
Khan FY, Elzouki AN. Clostridium difficile infection: a review of the literature. Asian Pac J Trop Med. 2014;7S1:S6-S13. https://doi.org/10.1016/S1995-7645(14)60197-8
Zacharioudakis IM, Zervou FN, Shehadeh F, Mylona EK, Mylonakis E. Association of Community Factors with Hospital-onset Clostridioides (Clostridium) difficile Infection: A Population Based U.S.-wide Study. EClinicalMedicine. 2019;8:12-19. https://doi.org/10.1016/j.eclinm.2019.02.001
Ford AC, Moayyedi P, Hanauer SB. Ulcerative colitis. BMJ. 2013;346:f432. https://doi.org/10.1136/bmj.f432
Institut national d’excellence en santé et en services sociaux (INESSS) [Internet]. Treatment of Clostridium difficile- Associated Diarrhea or Colitis. Quebec: INESSS; 2017. Disponible en: https://www.inesss.qc.ca/fileadmin/doc/INESSS/Rapports/Traitement/Guide_Cdifficile-EN.pdf
Lital Meyer S, Espinoza AR, Quera PR. Infección por clostridium difficile: epidemiología, diagnóstico y estrategias terapéuticas. Revista Médica Clínica Las Andes. 2014;25(3):473-84. https://doi.org/10.1016/S0716-8640(14)70064-1
Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015;313(4):398-408. https://doi.org/10.1001/jama.2014.17103
Seicean A, Moldovan-Pop A, Seicean R. Ulcerative colitis worsened after Clostridium difficile infection: efficacy of infliximab. World J Gastroenterol. 2014;20(17):5135-40. https://doi.org/10.3748/wjg.v20.i17.5135
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.

| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |















