Periampullary duodenal diverticula and technical-therapeutic failure during endoscopic retrograde cholangiopancreatography (ERCP)
DOI:
https://doi.org/10.22516/25007440.706Keywords:
Duodenal diverticulum, periampullary, Endoscopic retrograde cholangiopancreatography, cannulation, Papilla of VaterAbstract
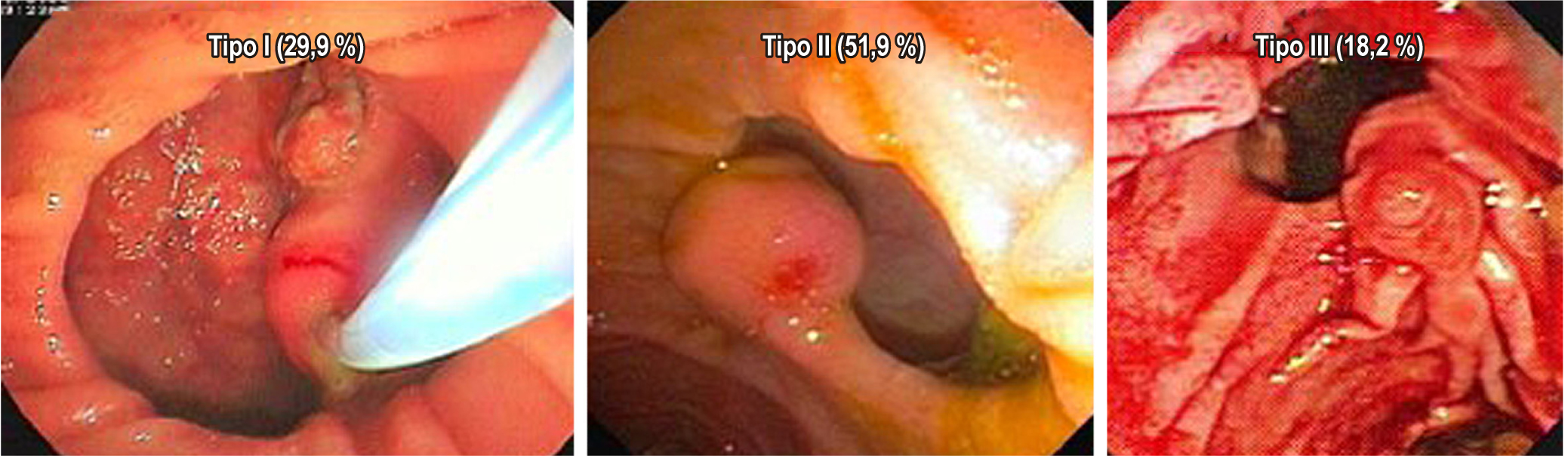
Introduction and aims: Periampullary duodenal diverticula (PDD) are rare and their finding is incidental. In addition, they are classified into three types according to Boix due to their proximity to the larger blister. The aim of this study was to describe our experience with this anatomical anomaly and to demonstrate how this affects the technical and therapeutic success rate of the procedure.
Materials and methods: A cross-sectional study was performed, with data collection retrospectively. Over a 5-year period of patients with duodenal periampullary diverticula. Therapeutic failure, complications and difficulty of cannulation of the bile duct were evaluated.
Results: 214 were assessed, with a women-men rate 2,15:1. The distribution of subjects by PDD was: Type I (29.9%), II (51.9%) y III (18. 2%). The most frequent indication of ERCP were the common bile duct stones at 53.3%. The PDD type I presented greater difficulty of cannulation (11.6%) and therapeutic failure (28.12%).
Conclusion: The presence of PDD during ERCP is associated with greater technical failure (failure in cannulation) and therapeutic failure (persistence of biliary obstruction). In addition, it is considerably increased when it is a Type I intradiverticular papilla of the Boix classification. Therefore, we suggest that biliary endoscopic procedures in these conditions be performed by endoscopists with great experience in order to minimize the probability of technical and therapeutic failure and associated complications.
Downloads
References
Boix J, Lorenzo-Zúñiga V, Añaños F, Domènech E, Morillas RM, Gassull MA. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surg Laparosc Endosc Percutan Tech. 2006;16(4):208-11. https://doi.org/10.1097/00129689-200608000-00002
Chen L, Xia L, Lu Y, Bie L, Gong B. Influence of periampullary diverticulum on the occurrence of pancreaticobiliary diseases and outcomes of endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol. 2017;29(1):105-111. https://doi.org/10.1097/MEG.0000000000000744
Coman IS, Radu EV, Șandru V, Bârsan IC, Badiu CD, Constantinescu G, Grigorean VT; -. Retained Common Bile Duct Lithiasis at a Pacient with Periampullary Duodenal Diverticulum. Chirurgia (Bucur). 2016;111(6):517-521. https://doi.org/10.21614/chirurgia.111.6.517
Ospina Nieto J. Impacto verdadero del divertículo periampular en la CPRE. Rev Colomb Gastroenterol. 2007;22(4):297-301.
Sun Z, Bo W, Jiang P, Sun Q. Different Types of Periampullary Duodenal Diverticula Are Associated with Occurrence and Recurrence of Bile Duct Stones: A Case-Control Study from a Chinese Center. Gastroenterol Res Pract. 2016;2016:9381759. https://doi.org/10.1155/2016/9381759
Sfarti VC, Bălan G Jr, Chiriac AŞ, Stanciu C, Bălan G, Gafencu-Şavlovschi D, Trifan AV. Endoscopic retrograde cholangiopancreatography (ERCP) in patients with periampullary diverticula. Rom J Morphol Embryol. 2018;59(3):833-837.
Karaahmet F, Kekilli M. The presence of periampullary diverticulum increased the complications of endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol. 2018;30(9):1009-1012. https://doi.org/10.1097/MEG.0000000000001172
Altonbary AY, Bahgat MH. Endoscopic retrograde cholangiopancreatography in periampullary diverticulum: The challenge of cannulation. World J Gastrointest Endosc. 2016;8(6):282-7. https://doi.org/10.4253/wjge.v8.i6.282
Gallego F, Gallardo F, Martínez G. Complicaciones de la colangiopancreatografía retrógrada endoscópica (CPRE). Identificación, prevención y manejo. PAPD. 2010; 33(1):22-36.
Declaración de Helsinki de la AMM-principios éticos para las investigaciones médicas en seres humanos [Internet]. AMM [consultado el 10 de junio de 2020]. Disponible en: https://www.wma.net/es/policies-post/declaracion-de-helsinki-de-la-amm-principios-eticos-para-las-investigaciones-medicas-en-seres-humanos/
Jakubczyk E, Pazurek M, Mokrowiecka A, Woźniak B, Małecka-Panas E, Podgórski M, Polguj M, Topol M. The position of a duodenal diverticulum in the area of the major duodenal papilla and its potential clinical implications. Folia Morphol (Warsz). 2021;80(1):106-113. https://doi.org/10.5603/FM.a2020.0012
Loffeld RJ, Dekkers PE. The Impact of Duodenal Diverticuli and the Execution of Endoscopic Retrograde Cholangiopancreaticography. Int Sch Res Notices. 2016;2016:5026289. https://doi.org/10.1155/2016/5026289
Güitrón-Cantú A, Adalid-Martínez R, Gutiérrez-Bermúdez JA, Segura-López KF, García-Vázquez A. Grado de dificultad para canular papila de Vater en presencia de divertículo duodenal periampular. Rev Gastroenterol Méx. 2010;75(3):273-80.
Major P, Dembiński M, Winiarski M, Pędziwiatr M, Rubinkiewicz M, Stanek M, Dworak J, Pisarska M, Rembiasz K, Budzyński A. A Periampullary Duodenal Diverticula in Patient with Choledocholithiasis - Single Endoscopic Center Experience. Pol Przegl Chir. 2016;88(6):328-333. https://doi.org/10.1515/pjs-2016-0072
Mahajan S, Rajesh K, Upender C, Mokta J, Satinder M. Duodenal diverticulum: Review of literature. Indian Journal of Surgery. 2004;66(3):140-5.
Örmeci N, Deda X, Kalkan Ç, Tüzün AE, Karakaya F, Dökmeci A, Bahar DK, Özkan H, İdilman R, Çınar K. Impact of Periampullary Diverticula on Bile Duct Stones and Ampullary Carcinoma. Euroasian J Hepatogastroenterol. 2016;6(1):31-34. https://doi.org/10.5005/jp-journals-10018-1162
Lee JJ, Brahm G, Bruni SG, Thipphavong S, Sreeharsha B. Biliary dilatation in the presence of a periampullary duodenal diverticulum. Br J Radiol. 2015;88(1053):20150149. https://doi.org/10.1259/bjr.20150149
Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(7):657-83. https://doi.org/10.1055/s-0042-108641
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














