2010 vs. 2019 ASGE criteria for choledocholithiasis in patients undergoing endoscopic retrograde cholangiopancreatography
DOI:
https://doi.org/10.22516/25007440.883Keywords:
Choledocholithiasis, Endoscopic Retrograde Cholangiopancreatography, Health SystemsAbstract
Introduction: With the update of the American Society for Gastrointestinal Endoscopy (ASGE) 2019 guidelines, the criteria for patients with suspected choledocholithiasis became stricter when choosing who should be taken directly to endoscopic retrograde cholangiopancreatography (ERCP). This study aimed to compare patients taken directly to ERCP according to the 2010 vs. 2019 ASGE guidelines versus the 2019 guide.
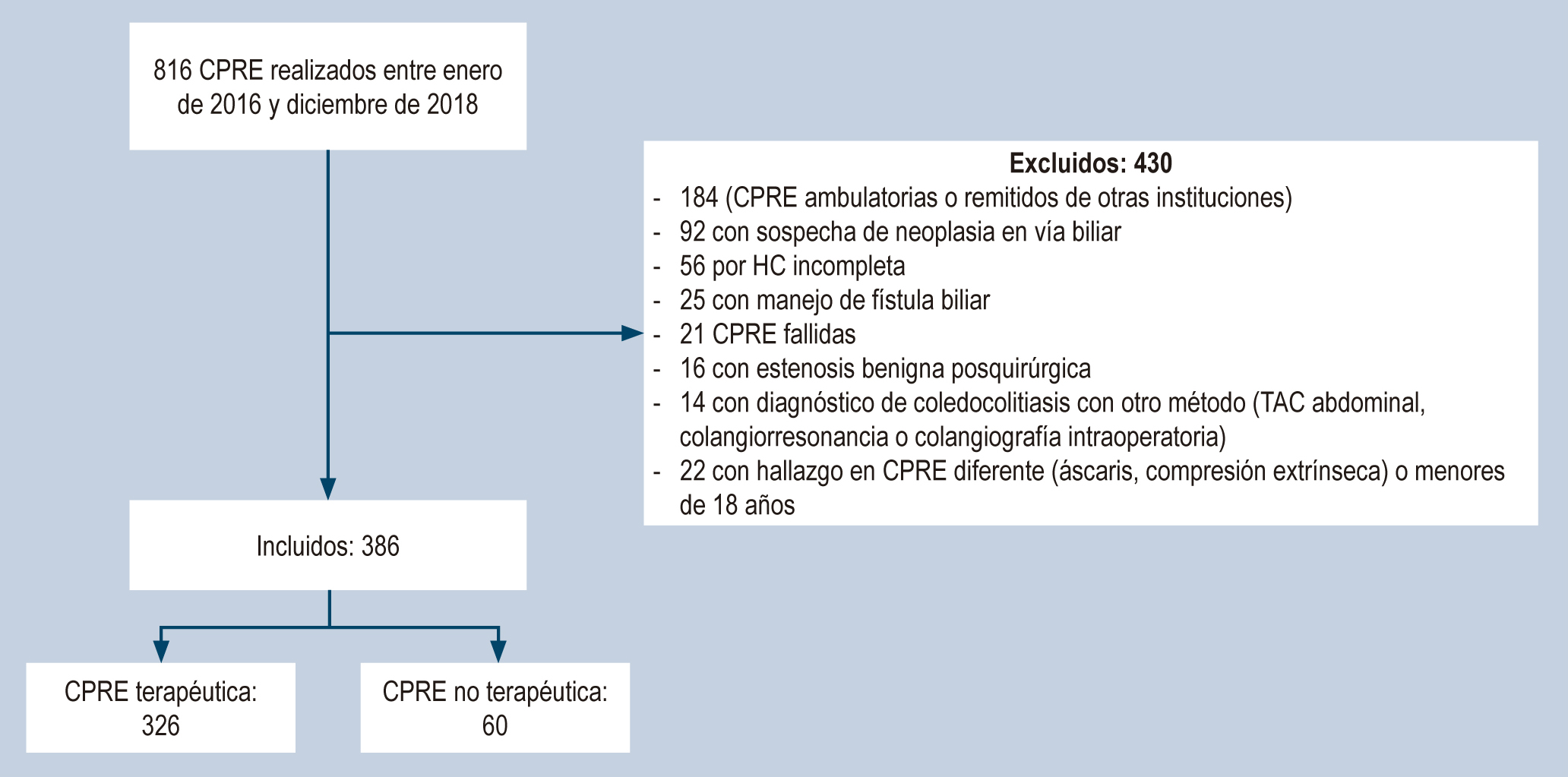
Materials and methods: A retrospective study of ERCPs performed between January 2016 and December 2018 evaluated the diagnostic performance of paraclinical and ultrasound variables individually and collectively to compare their sensitivity, specificity, predictive values, and high probability precision according to 2019 and 2010 guidelines regarding the presence of stones in ERCPs.
Results: 386 patients underwent ERCP due to suspicion of choledocholithiasis; 84.5% were therapeutic procedures. The high probability group had a higher rate of therapeutic ERCP: 89.3% according to the 2019 guidelines compared to those of 2010 with 86.3% (p < 0.001). The sensitivity and specificity of high probability according to the 2010 guidelines were 86.8% and 25.0%, respectively, with a positive predictive value (PPV) of 86.3% and an accuracy of 77.2%. According to the 2019 guidelines, high probability showed lower sensitivity (74%) but higher specificity (51.7%), a PPV of 89.3%, and an accuracy of 70.7%.
Conclusions: The implementation of the ASGE 2019 guidelines on the indications for ERCP should consider the resources of hospitals, especially in low- and middle-income countries. The ASGE 2010 guidelines show good sensitivity and precision to guide the performance of ERCP.
Downloads
References
ASGE Standards of Practice Committee, Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1-9. https://doi.org/10.1016/j.gie.2009.09.041
He H, Tan C, Wu J, Dai N, Hu W, Zhang Y, et al. Accuracy of ASGE high-risk criteria in evaluation of patients with suspected common bile duct stones. Gastrointest Endosc. 2017;86(3):525-32. https://doi.org/10.1016/j.gie.2017.01.039
Adams MA, Hosmer AE, Wamsteker EJ, Anderson MA, Elta GH, Kubiliun NM, et al. Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc. 2015;82(1):88-93. https://doi.org/10.1016/j.gie.2014.12.023
Sethi S, Wang F, Korson AS, Krishnan S, Berzin TM, Chuttani R, et al. Prospective assessment of consensus criteria for evaluation of patients with suspected choledocholithiasis. Dig Endosc Off J Jpn Gastroenterol Endosc Soc. 2016;28(1):75-82. https://doi.org/10.1111/den.12506
Ripari G, Wulfson A, Guerrina C, Perroud H. Correlación entre predictores de litiasis coledociana y los hallazgos en la colangiopancreatografía retrógrada endoscópica. Acta Gastroenterol Latinoam. 2017;47(4):269-76.
Rubin MIN, Thosani NC, Tanikella R, Wolf DS, Fallon MB, Lukens FJ. Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: testing the current guidelines. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2013;45(9):744-9. https://doi.org/10.1016/j.dld.2013.02.005
Gómez Hinojosa P, Espinoza-Ríos J, Bellido Caparo A, Pinto Valdivia JL, Rosado Cipriano M, Prochazka Zarate R, et al. Precisión de los predictores de la ASGE en el diagnóstico de coledocolitiasis en un hospital público de Lima, Perú. Rev Gastroenterol Perú. 2018;38(1):22-8.
ASGE Standards of Practice Committee, Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89(6):1075-1105.e15. https://doi.org/10.1016/j.gie.2018.10.001
Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102(8):1781-8. https://doi.org/10.1111/j.1572-0241.2007.01279.x
Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepato-Biliary-Pancreat Sci. 2018;25(1):17-30. https://doi.org/10.1002/jhbp.515
Chandran A, Rashtak S, Patil P, Gottlieb A, Bernstam E, Guha S, et al. Comparing diagnostic accuracy of current practice guidelines in predicting choledocholithiasis: outcomes from a large healthcare system comprising both academic and community settings. Gastrointest Endosc. 2021;93(6):1351-9. https://doi.org/10.1016/j.gie.2020.10.033
Hasak S, McHenry S, Busebee B, Fatima S, Sloan I, Weaver M, et al. Validation of choledocholithiasis predictors from the «2019 ASGE Guideline for the role of endoscopy in the evaluation and management of choledocholithiasis.» Surg Endosc. 2022;36(6):4199-206. https://doi.org/10.1007/s00464-021-08752-z
Jacob JS, Lee ME, Chew EY, Thrift AP, Sealock RJ. Evaluating the Revised American Society for Gastrointestinal Endoscopy Guidelines for Common Bile Duct Stone Diagnosis. Clin Endosc. 2021;54(2):269-74. https://doi.org/10.5946/ce.2020.100
Montoya-Botero J, Oliveros-Wilches R, Abadía-Díaz M, Sánchez-Pedraza R, Garrido-Bohórquez A de J, Manrique-Acevedo ME, et al. Colangiopancreatografía retrógrada endoscópica en una institución de referencia en cáncer. Rev Colomb Gastroenterol. 2020;35(4):430-5. https://doi.org/10.22516/25007440.512
Garcés Otero JS, Mejía Henao PA, Uribe A, Serrano Otero JA, Velásquez A, Agudelo Posada JJ, et al. Complicaciones y factores de riesgo en pacientes sometidos a colagiopancreatografía retrógrada endoscópica en una clínica de tercer nivel de Medellín desde el 2014 hasta el 2017. Rev Colomb Cir 2020;35(1):57-65. https://doi.org/10.30944/20117582.588
Lee HJ, Cho CM, Heo J, Jung MK, Kim TN, Kim KH, et al. Impact of Hospital Volume and the Experience of Endoscopist on Adverse Events Related to Endoscopic Retrograde Cholangiopancreatography: A Prospective Observational Study. Gut Liver. 2020;14(2):257-64. https://doi.org/10.5009/gnl18537
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














