Unusual Association of Intestinal Tuberculosis and Thalassemia: A Case Report
DOI:
https://doi.org/10.22516/25007440.942Keywords:
tuberculosis, thalassemia, glutathione, iron, case reportAbstract
Introduction: Tuberculosis is an infectious disease that can be prevented and cured, but it is still associated with high morbidity and mortality rates. Disseminated tuberculosis, although rare, can occur in individuals with underlying pathologies that affect the immune system. Currently, there are limited reports on disseminated tuberculosis in individuals with congenital disorders.
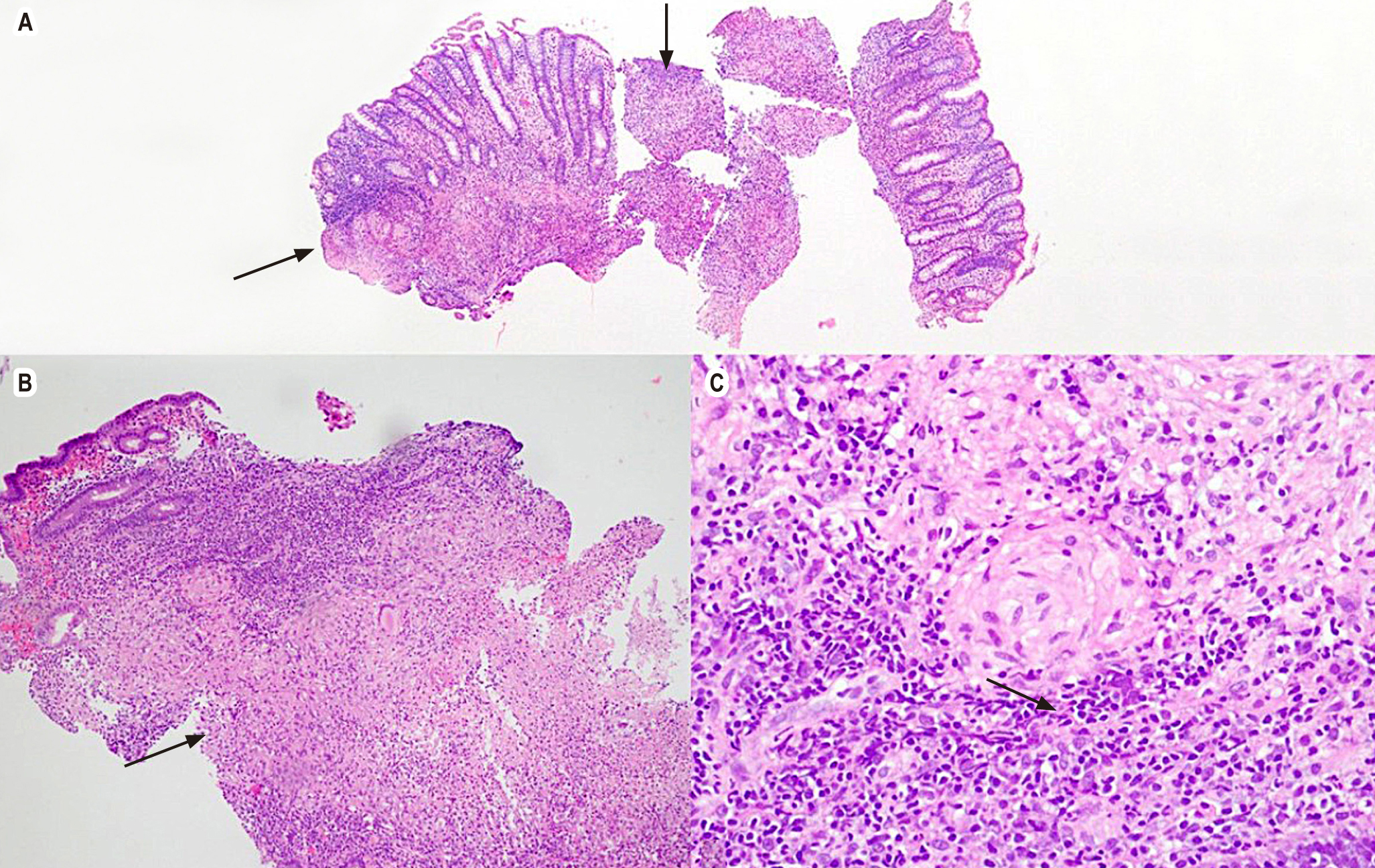
Clinical case: We present a case of a patient with a history of β thalassemia who was admitted to the emergency department with symptoms of abdominal pain and constitutional symptoms. The final diagnosis was disseminated tuberculosis. This case is of particular interest due to its atypical presentation, the initial suspicion of malignancy, and the extensive involvement of the disease despite the patient’s absence of immunosuppression history.
Conclusions: Disseminated tuberculosis in immunocompetent patients is a rare presentation associated with poor outcomes. The history of β thalassemia may be a risk factor to consider based on the metabolic pathways involved in the pathophysiology of both diseases.
Downloads
References
WHO Global Tuberculosis Programme. TB: a global emergency, WHO report on the TB epidemic [Internet]. Geneva: World Health Organization; 1994 [consultado el 11 de julio de 2022]. Disponible en: https://apps.who.int/iris/handle/10665/58749
Furin J, Cox H, Pai M. Tuberculosis. Lancet. 2019;393(10181):1642–56. https://doi.org/10.1016/S0140-6736(19)30308-3
Natarajan A, Beena PM, Devnikar AV, Mali S. A systemic review on tuberculosis. Indian J Tuberculosis. 2020;67(3):295–311. https://doi.org/10.1016/j.ijtb.2020.02.005
World Health Organization. Global tuberculosis report 2021 [Internet]. Geneva: World Health Organization; 2021 [onsultado el 11 de julio de 2022]. Disponible en: https://apps.who.int/iris/handle/10665/346387
Ugarte-Gil C, Carrillo-Larco RM, Kirwan DE. Latent tuberculosis infection and non-infectious co-morbidities: Diabetes mellitus type 2, chronic kidney disease and rheumatoid arthritis. International J Infect Dis. 2019;80:S29–31. https://doi.org/10.1016/j.ijid.2019.02.018
Khan FY. Review of literature on disseminated tuberculosis with emphasis on the focused diagnostic workup. J Family Community Med. 2019;26(2):83-91. https://doi.org/10.4103/jfcm.JFCM_106_18
Baby J, Poovathingal S, Valsalan P, Sunila E. Atypical Presentation of Disseminated Tuberculosis. Journal of the Royal College of Physicians of Edinburgh. 2020;50(4):405–7. https://doi.org/10.4997/jrcpe.2020.411
García-Rodríguez JF, Álvarez-Díaz H, Lorenzo-García MV, Mariño-Callejo A, Fernández-Rial Á, Sesma-Sánchez P. Extrapulmonary tuberculosis: epidemiology and risk factors. Enfermedades Infecciosas y Microbiología Clínica. 2011;29(7):502-9. https://doi.org/10.1016/j.eimc.2011.03.005
Pang Y, An J, Shu W, Huo F, Chu N, Gao M, et al. Epidemiology of Extrapulmonary Tuberculosis among Inpatients, China, 2008–2017. Emerging Infectious Diseases. 2019;25(3):457-64. https://doi.org/10.3201/eid2503.180572
Meira L, Chaves C, Araújo D, Almeida L, Boaventura R, Ramos A, et al. Predictors and outcomes of disseminated tuberculosis in an intermediate burden setting. Pulmonology. 2019;25(6):320–7. https://doi.org/10.1016/j.pulmoe.2018.11.001
Wang JY, Hsueh PR, Wang SK, Jan IS, Lee LN, Liaw YS, et al. Disseminated Tuberculosis. Medicine. 2007;86(1):39–46. https://doi.org/10.1097/MD.0b013e318030b605
Taher AT, Musallam KM, Cappellini MD. β-Thalassemias. New Eng J Med. 2021;384(8):727-43. https://doi.org/10.1056/NEJMra2021838
Wise J. WHO identifies 16 countries struggling to control tuberculosis. BMJ. 1998;316(7136):957. https://doi.org/10.1136/bmj.316.7136.955e
Fucharoen S, Winichagoon P. Haemoglobinopathies in southeast Asia. Indian J Med Res. 2011;134(4):498–506. http://www.ncbi.nlm.nih.gov/pubmed/22089614
Sriwijitalai W, Wiwanitkit V. Tuberculosis in patients with underlying thalassemia: a consideration of common antioxidative pathway − an expressional analysis. Egyptian Journal of Chest Disease and Tuberculosis. 2021;70(1):38-9. https://doi.org/10.4103/ejcdt.ejcdt_159_19
Ruoqiong C, Garrett T, Hicret I, Rachel A, Shalok M, Karo G, et al. Characterizing the Effects of Glutathione as an Immunoadjuvant in the Treatment of Tuberculosis. Antimicrobial Agents and Chemotherapy. 2018;62(11):e01132-18. https://doi.org/10.1128/AAC.01132-18
Chakraborty I, Mitra S, Gachhui R, Kar M. Non-haem iron-mediated oxidative stress in haemoglobin E beta-thalassaemia. Ann Acad Med Singap. 2010;39(1):13-6. http://www.ncbi.nlm.nih.gov/pubmed/20126808
Kalpravidh RW, Tangjaidee T, Hatairaktham S, Charoensakdi R, Panichkul N, Siritanaratkul N, et al. Glutathione redox system in β -thalassemia/Hb E patients. ScientificWorldJournal. 2013;2013:543973. https://doi.org/10.1155/2013/543973
Gluba-Brzózka A, Franczyk B, Rysz-Górzyńska M, Rokicki R, Koziarska-Rościszewska M, Rysz J. Pathomechanisms of Immunological Disturbances in β-Thalassemia. International Journal of Molecular Sciences. 2021;22(18):9677. https://doi.org/10.3390/ijms22189677
Khan FA, Fisher MA, Khakoo RA. Association of hemochromatosis with infectious diseases: expanding spectrum. International Journal of Infectious Diseases. 2007;11(6):482-7. https://doi.org/10.1016/j.ijid.2007.04.007
Gangaidzo IT, Moyo VM, Mvundura E, Aggrey G, Murphree NL, Khumalo H, et al. Association of Pulmonary Tuberculosis with Increased Dietary Iron. The Journal of Infectious Diseases. 2001;184(7):936–9. https://doi.org/10.1086/323203
Centers for Disease Control and Prevention. Latent Tuberculosis Infection: a Guide for Primary Health Care Providers. Atlanta, US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of Tuberculosis Elimination, 2020. [Consultado el 11 de julio de 2022]. Disponible en:https://www.cdc.gov/tb/publications/ltbi/pdf/LTBIbooklet508.pdf
Ottenhoff THM, Verreck FAW, Hoeve MA, van de Vosse E. Control of human host immunity to mycobacteria. Tuberculosis. 2005;85(1-2):53–64. https://doi.org/10.1016/j.tube.2004.09.011
Lounis N, Truffot-Pernot C, Grosset J, Gordeuk VR, Boelaert JR. Iron and Mycobacterium tuberculosis infection. Journal of Clinical Virology. 2001;20(3):123–6. https://doi.org/10.1016/S1386-6532(00)00136-0
Ghozali M, Dewi SP, Ghrahani R, Maskoen AM, Reniarti L, Sahiratmadja E, et al. Natural resistance-associated macrophage protein 1 gene polymorphisms in thalassemia patients with tuberculosis infection. Paediatr Indones. 2016;56(2):84-9. https://doi.org/10.14238/pi56.2.2016.84-9
Agrawal A, Shrivastava J, Singh A. Multidrug-resistant tubercular liver abscess in β-thalassemia. Indian Pediatr. 2014;51(5):401-2.
Hanafiah M, Mukhari SAM, Mustapha AM, Mumin NA. Intraventricular tuberculosis abscess in an immunocompromised patient: clinical vignette. Asian Biomedicine. 2021;15(6):293-7. https://doi.org/10.2478/abm-2021-0036
Harahap S, Pramudita A, Lusiani. Cardiac tamponade as a manifestation of extrapulmonary tuberculosis in β thalassemia major patient. IOP Conference Series. 2018;125: 012120. https://doi.org/10.1088/1755-1315/125/1/012120
Kataria SP, Avasthi R. Sternal tuberculosis in combination with thalassmia. J Assoc Physicians India. 1993;41(7):472.
Chit Yee D, Aung HKK, Mg Mg B, Htun WPP, Janurian N, Bancone G, et al. Case Report: A case report of multiple co-infections (melioidosis, paragonimiasis, Covid-19 and tuberculosis) in a patient with diabetes mellitus and thalassemia-trait in Myanmar. Wellcome Open Research. 2022;7:160. https://doi.org/10.12688/wellcomeopenres.17881.1
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista colombiana de Gastroenterología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |