Endoscopic hemostasis in intensive care unit patients with upper digestive tract bleeding
DOI:
https://doi.org/10.22516/25007440.362Keywords:
intensive care, hemorrhage, endoscopyAbstract
Introduction: Patients hospitalized in an intensive care unit (ICU) are at risk of upper gastrointestinal bleeding. Esophagogastroduodenoscopy (EGD) is the test of choice for these patients. EGD is diagnostic and therapeutic. Many endoscopically identified lesions do not require endoscopic treatment. In Colombia there are no studies on the prevalence of different upper gastrointestinal bleeding lesions in ICU patients, nor on the use of therapeutic EGD in these patients.
Materials and methods: This is a cross-sectional study conducted at the Clínica Fundadores in Bogotá Colombia between January 2003 and February 2017. Adult ICU patients who underwent EGD due to upper gastrointestinal bleeding were included.
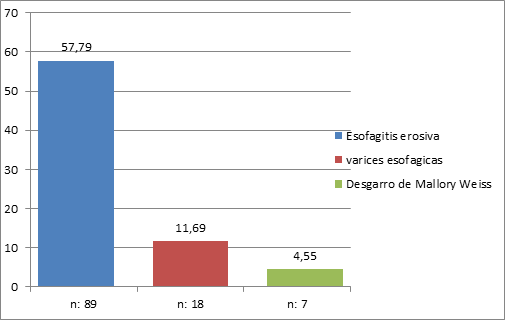
Results: In the final analysis, 156 patients who underwent EGD were included. Of these, 76.62% (118) had chronic gastritis, 57.79% (89) had erosive esophagitis grades A to D, 47.4% (73) had erosive gastritis, 21.43% (33) had erosive duodenitis, 18.18% (28) had gastric ulcer, 11.69% (18) had esophageal varices, 11.04% (17) had duodenal ulcers, and 4.55% (8) Mallory Weiss tears. Only 15% of patients, including those with esophageal varices, required endoscopic management,.
Conclusions: In this study, 15% of patients with upper gastrointestinal bleeding required endoscopic treatment. Prospective work should be done to establish risk factors to predict the need for therapeutic EGD in patients with upper gastrointestinal bleeding. Patients do not have these predictors should be treated empirically with PPI to avoid unnecessary expenses of diagnostic EGDs.
Downloads
References
Marik P, Vasu T, Hirani A, Pachinburavan M. Stress ulcer prophylaxis in the new millennium: a systematic review and meta-analysis. Crit Care Med. 2010;38(11):2222-8. doi: https://doi.org/10.1097/CCM.0b013e3181f17adf.
Krag M, Perner A, Wetterslev J, Wise M, Borthwick M, Bendel S, et al. Stress ulcer prophylaxis in the intensive care unit: an international survey of 97 units in 11 countries. Acta Anaesthesiol Scand. 2015;59(5):576-85. doi: https://doi.org/10.1111/aas.12508.
Krag M, Perner A, Wetterslev J, Wise M, Borthwick M, Bendel S, et al. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med. 2015;41(5):833-45. doi: https://doi.org/10.1007/s00134-015-3725-1.
Cook D, Griffith L, Walter S, Guyatt G, Meade M, Heyland DK, et al. The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients. Crit Care. 2001;5(6):368. doi: https://doi.org/10.1186/cc1071.
Cook D, Fuller H, Guyatt G, Marshall J, Leasa D, Hall R, et al. Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med. 1994;330(6):377-81. doi: https://doi.org/10.1056/NEJM199402103300601.
Cipolletta L, Cipolletta F, Granata A, Ligresti D, Barresi L, Tarantino I, et al. What is the best endoscopic strategy in acute non-variceal gastrointestinal bleeding? Curr Treat Optios Gastro. 2018;16(4):363-75. doi: https://doi.org/10.1007/s11938-018-0192-0.
Jean-Baptiste S, Messika J, Hajage D, Gaudry S, Barbieri J, Duboc H, et al. Clinical impact of upper gastrointestinal endoscopy in critically ill patients with suspected bleeding. Ann Intensive Care. 2018;8(1):75. doi: https://doi.org/10.1186/s13613-018-0423-5.
Barkun A, Bardou M, Kuipers E, Sung J, Hunt R, Martel M, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Inter Med. 2010;152(2):101-13. doi: https://doi.org/10.7326/0003-4819-152-2-201001190-00009.
Lau J, Barkun A, Fan DM, Kuipers E, Yang YS, Chan F. Challenges in the management of acute peptic ulcer bleeding. Lancet. 2013;381(9882):2033-43. doi: https://doi.org/10.1016/S0140-6736(13)60596-6.
Chak A, Cooper G, Lloyd L, Kolz C, Barnhart B, Wong R. Effectiveness of endoscopy in patients admitted to the intensive care unit with upper GI hemorrhage. Gastrointest Endoscop. 2001;53(1):6-13. doi: https://doi.org/10.1067/mge.2001.108965.
Lee YC, Wang HP, Wu MS, Yang CS, Chang YT, Lin JT. Urgent bedside endoscopy for clinically significant upper gastrointestinal hemorrhage after admission to the intensive care unit. Intensive Care Med. 2003;29(10):1723-8. doi: https://doi.org/10.1007/s00134-003-1921-x.
Tam W, Bertholini D. Tension pneumoperitoneum, pneumomediastinum, subcutaneous emphysema and cardiorespiratory collapse following gastroscopy. Anaesth Intensive Care. 2007;35(2):307-9.
Conrad SA. Acute upper gastrointestinal bleeding in critically ill patients: causes and treatment modalities. Crit Care Med. 2002;30(6):S365-S8. doi: https://doi.org/10.1097/00003246-200206001-00006.
Eddleston J, Pearson R, Holland J, Tooth J, Vohra A, Doran BH. Prospective endoscopic study of stress erosions and ulcers in critically ill adult patients treated with either sucralfate or placebo. Critic Care Med. 1994;22(12):1949-54. doi: https://doi.org/10.1097/00003246-199422120-00010.
Marker S, Krag M, Møller M. What's new with stress ulcer prophylaxis in the ICU? Intensive Care Med. 2017;43(8):1132-4. doi: https://doi.org/10.1007/s00134-017-4733-0.
Granholm A, Lange T, Anthon C, Marker S, Krag M, Meyhoff T, et al. Timing of onset of gastrointestinal bleeding in the ICU: protocol for a preplanned observational study. Acta Anaesth Scand. 2018. doi: https://doi.org/10.1111/aas.13144.
Plummer M, Blaser A, Deane A. Stress ulceration: prevalence, pathology and association with adverse outcomes. Crit Care. 2014;18(2):213. doi: https://doi.org/10.1186/cc13780.
Steinberg K. Stress-related mucosal disease in the critically ill patient: risk factors and strategies to prevent stress-related bleeding in the intensive care unit. Crit Care Med. 2002;30(6):S362-S4. doi: https://doi.org/10.1097/00003246-200206001-00005.
Siddiqui F, Ahmed M, Abbasi S, Avula A, Siddiqui A, Philipose J, et al. Gastrointestinal bleeding in patients with acute respiratory distress syndrome: a national database analysis. J Clin Med Res. 2019;11(1):42-8. doi: https://doi.org/10.14740/jocmr3660.
Alvarado J. Profilaxis de sangrado digestivo en la Unidad de Cuidados Intensivos. Univ Med. 2002;43(1):33-5.
Schuster D, Rowley H, Feinstein S, McGue M, Zuckerman G. Prospective evaluation of the risk of upper gastrointestinal bleeding after admission to a medical intensive care unit. Am J med. 1984;76(4):623-30. doi: https://doi.org/10.1016/0002-9343(84)90286-9.
Huang HB, Jiang W, Wang CY, Qin HY, Du B. Stress ulcer prophylaxis in intensive care unit patients receiving enteral nutrition: a systematic review and meta-analysis. Crit Care. 2018;22(1):20. doi: https://doi.org/10.1186/s13054-017-1937-1.
Beejay U, Wolfe M. Acute gastrointestinal bleeding in the intensive care unit: the gastroenterologist's perspective. Gastroenterol Clin North Am. 2000;29(2):309-36. doi: https://doi.org/10.1016/S0889-8553(05)70118-7.
Morales C, Sierra S, Hernández A, Arango A, López G. Hemorragia digestiva alta: factores de riesgo para mortalidad en dos centros urbanos de América Latina. Rev Esp Enferme Dig. 2011;103(1):20-4. doi: https://doi.org/10.4321/S1130-01082011000100004.
Lewis J, Shin E, Metz D. Characterization of gastrointestinal bleeding in severely ill hospitalized patients. Crit Care Med. 2000;28(1):46-50. doi: https://doi.org/10.1097/00003246-200001000-00007.
Kim J, Kim J, Chun J, Lee C, Im J, Kim J. Early versus late bedside endoscopy for gastrointestinal bleeding in critically ill patients. Korean J Intern med. 2018;33(2):304-12. doi: 10.3904/kjim.2016.182.
Hayden S, Albert T, Watkins T, Swenson E. Anemia in critical illness: insights into etiology, consequences, and management. American J Respir Crit Care Med. 2012;185(10):1049-57. doi: https://doi.org/10.1164/rccm.201110-1915CI.
Sesler J. Stress-related mucosal disease in the intensive care unit. AACN Advanced Crit Care. 2007;18(2):119-28. doi: https://doi.org/10.4037/15597768-2007-2004.
Silverstein F, Gilbert D, Tedesco F, Buenger N, Persing J. The national ASGE survey on upper gastrointestinal bleeding: II. Clinical prognostic factors. Gastrointest Endoscop. 1981;27(2):80-93. doi: https://doi.org/10.1016/S0016-5107(81)73156-0.
van Leerdam M. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22(2):209-24. doi: https://doi.org/10.1016/j.bpg.2007.10.011.
Ovenden C, Plummer M, Selvanderan S, Donaldson T, Nguyen N, Weinel L, et al. Occult upper gastrointestinal mucosal abnormalities in critically ill patients. Acta Anaesthesiol Scand. 2017;61(2):216-23. doi: https://doi.org/10.1111/aas.12844.
Rich K. Overview of Mallory-Weiss syndrome. J Vasc Nurs. 2018;36(2):91-3. doi: https://doi.org/10.1016/j.jvn.2018.04.001.
Guelrud M. Mallory-Weiss syndrome. UptoDate. 2017. Último acceso: 15 de junio de 2018. Disponible en: https://www.uptodate.com/contents/mallory-weiss-syndrome
Cucci M, Capputo F, Fraternali G, Roncallo A, Ventura F. Transition of a Mallory-Weiss syndrome to a Boerhaave syndrome confirmed by anamnestic, necroscopic, and autopsy data. A case report. Medicine (Baltimore). 2018;97(49):e13191. doi: https://doi.org/10.1097/MD.0000000000013191.
Skok P, Sinkovič A. Upper gastrointestinal haemorrhage: predictive factors of in-hospital mortality in patients treated in the medical intensive care unit. J Int Med Res. 2011;39(3):1016-27. doi: https://doi.org/10.1177/147323001103900337.
Gralnek I, Dumonceau J, Kuipers E, Lanas A, Sanders D, Kurien M, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47(10):a1-a46. doi: https://doi.org/10.1055/s-0034-1393172.
Krag M, Marker S, Perner A, Wetterslev J, Wise M, Schefold J, et al. Pantoprazole in patients at risk for gastrointestinal bleeding in the ICU. N Engl J Med. 2018;379(23):2199-208.
Rehman A, Iscimen R, Yilmaz M, Khan H, Belsher J, Gomez JF, et al. Prophylactic endotracheal intubation in critically ill patients undergoing endoscopy for upper GI hemorrhage. Gastrointest Endoscop. 2009;69(7):e55-e9. doi: https://doi.org/10.1016/j.gie.2009.03.002.
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














