Characteristics of Inflammatory Bowel Disease compared to other National Centers in Colombia
DOI:
https://doi.org/10.22516/25007440.752Keywords:
Inflammatory bowel disease, Colombia, Ulcertaive colitis, Crohn's disease, PhenotypeAbstract
Introduction: Inflammatory bowel disease (IBD) is an immune-mediated disease whose incidence in Latin America has increased in recent years.
Aim: To analyze the demographic and clinical characteristics of patients with IBD treated in a university hospital and present the epidemiological data compared to other centers in Colombia.
Patients and methods: Descriptive study of patients with IBD (1996-2019) at the Hospital Universitario Fundación Santa Fe de Bogotá. Analysis of data from centers in Medellín, Cali, Bogotá, and Cartagena.
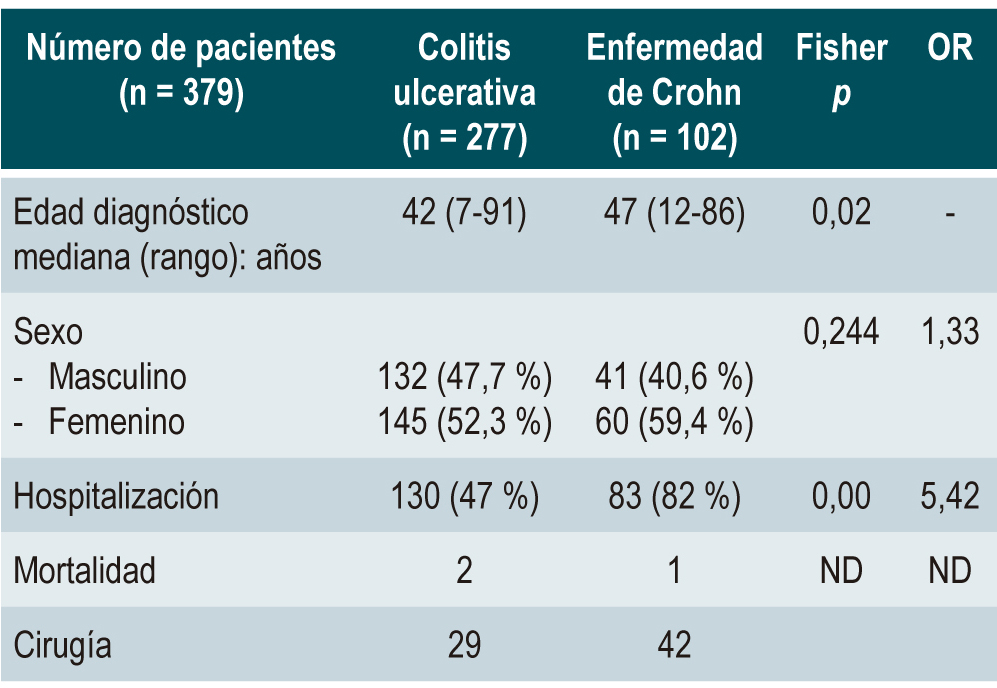
Results: Of 386 patients, 277 presented with ulcerative colitis (UC), 102 with Crohn’s disease (CD), and seven with unclassifiable colitis. IBD was more frequent in women (53 %). Mortality was less than 1 %. The involvement of UC was mainly pancolitis (42.6 %). The greater the extent of the disease, the higher the hospitalization and surgery rates (OR 3.70, P < 0.01). Thirteen percent of patients with UC received biologics. Compromise due to CD was mainly ileocolonic (43.6 %) and ileal (43.6 %). The predominant clinical pattern of CD was structuring (50%). Forty-five percent received biologicals and 56 % surgery. Primary sclerosing cholangitis (PSC) was found in 4 % of patients (n = 15). Two patients with PSC developed colorectal cancer (OR 4.18; p 0.008), while 13 patients with UC developed colon cancer and seven dysplastic changes. Three patients with CD developed colon cancer.
Conclusions: The results were compared to other reference centers. We found similar trends in the clinical behavior and treatment of IBD, with higher hospitalization and surgery rates in our cases.
Downloads
References
Sairenji T, Collins KL, Evans DV. An update on inflammatory bowel disease. Primary Care. 2017;44(4):673-92. https://doi.org/10.1016/j.pop.2017.07.010
Johnston RD, Logan RF. What is the peak age for onset of IBD? Inflamm Bowel Dis. 2008;14 Suppl 2:S4-5. https://doi.org/10.1002/ibd.20545
Khalili H. The changing epidemiology of inflammatory bowel disease: What goes up may come down. Inflamm Bowel Dis. 2020;26(4):591-2. https://doi.org/10.1093/ibd/izz186
Torabi M, Bernstein CN, Yu BN, Wickramasinghe L, Blanchard JF, Singh H. Geographical variation and factors associated with inflammatory bowel disease in a central Canadian province. Inflamm Bowel Dis. 2020;26(4):581-90. https://doi.org/10.1093/ibd/izz168
Ciapponi A, Virgilio SA, Berrueta M, Soto NC, Ciganda Á, Rojas Illanes MF, et al. Epidemiology of inflammatory bowel disease in Mexico and Colombia: Analysis of health databases, mathematical modelling and a case-series study. PLoS One. 2020;15(1):e0228256. https://doi.org/10.1371/journal.pone.0228256
Juliao-Baños F, Puentes F, López R, Saffon MA, Reyes G, Parra V, et al. Caracterización de la enfermedad inflamatoria intestinal en Colombia: resultados de un registro nacional. Rev Gastroenterol Mex. 2021;86(2):153-62. https://doi.org/10.1016/j.rgmx.2020.05.005
Kucharzik T, Ellul P, Greuter T, Rahier JF, Verstockt B, Abreu C, et al. ECCO guidelines on the prevention, diagnosis, and management of infections in inflammatory bowel disease. Crohns Colitis. 2021;15(6):879-913. https://doi.org/10.1093/ecco-jcc/jjab052
Lichtenstein G, Loftus Jr EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. Management of Crohn’s disease in adults. Am J Gastroenterol. 2018;113(4):481-517. https://doi.org/10.1038/ajg.2018.27
Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: Ulcerative colitis in adults. Am J Gastroenterol. 2019;114(3):384-413. https://doi.org/10.14309/ajg.0000000000000152
Sehgal R, Koltun WA. Scoring systems in inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2010;4(4):513-21. https://doi.org/10.1586/egh.10.40
Juliao Baños F, Ruiz Vélez MH, Flórez Arango JF, Donado Gómez JH, Marín Zuluaga JI, Monsalve Arango C, et al. Fenotipo e historia natural de la enfermedad inflamatoria intestinal en un centro de referencia en Medellín-Colombia. Rev Col Gastroenterol. 2010;25(3):240-51.
Rojas Rodríguez CA, Sánchez Londoño S, Rojas N, Sepúlveda Copete M, García Abadía JA, Jiménez Rivera DF, et al. Descripción clínico-epidemiológica de pacientes con enfermedad inflamatoria intestinal en una clínica de cuarto nivel en Cali. Rev Colomb Gastroenterol. 2020;35(2):166-73. https://doi.org/10.22516/25007440.409
Reyes Medina GA, Gil Parada FL, Carvajal Patiño GD, Sánchez Luque CB, Aponte Martin DM, González CA, et al. Enfermedad inflamatoria intestinal: características de fenotipo y tratamiento en un hospital universitario de Bogotá, Colombia. Rev Colomb Gastroenterol. 2018;33(2):117-26. https://doi.org/10.22516/25007440.196
Yepes Barreto IJ, Carmona R, Díaz F, Marín-Jiménez I. Prevalencia y características demográficas de la enfermedad inflamatoria intestinal en Cartagena, Colombia. Rev Col Gastroenterol. 2010;25(2):107-11.
Aguirre D, Archila PE, Carrera J, Castaño R, Escobar CM, García Duperly R, et al. Consenso colombiano de enfermedad inflamatoria intestinal. Rev Col Gastroenterol. 2012;27(Supl 1):s1-s44.
Loftus EV Jr, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Crohn’s disease in Olmsted County, Minnesota, 1940-1993: Incidence, prevalence, and survival. Gastroenterology. 1998;114(6):1161-8. https://doi.org/10.1016/S0016-5085(98)70421-4
Zelinkova Z. Gender and inflammatory bowel disease. J Clin Cel Immunol. 2014;5(4):245. https://doi.org/10.4172/2155-9899.1000245
Rottoli M, Remzi FH, Shen B, Kiran RP. Gender of the patient may influence perioperative and long-term complications after restorative proctocolectomy. Colorectal Dis. 2012;14(3):336-41. https://doi.org/10.1111/j.1463-1318.2011.02634.x
Samuel S, Ingle SB, Dhillon S, Yadav S, Harmsen WS, Zinsmeister AR, et al. Cumulative incidence and risk factors for hospitalization and surgery in a population-based cohort of ulcerative colitis. Inflamm Bowel Dis. 2013;19(9):1858-66. https://doi.org/10.1097/MIB.0b013e31828c84c5
Sulz MC, Siebert U, Arvandi M, Gothe RM, Wurm J, von Känel R, et al. Predictors for hospitalization and outpatient visits in patients with inflammatory bowel disease: Results from the Swiss Inflammatory Bowel Disease Cohort Study. Eur J Gastroenterol Hepatol. 2013;25(7):790-7. https://doi.org/10.1097/MEG.0b013e32836019b9
Núñez F P, Quera P R, Gomollón F. Primary sclerosing cholangitis and inflammatory bowel disease: Intestine-liver interrelation. Gastroenterol Hepatol. 2019;42(5):316-25. https://doi.org/10.1016/j.gastrohep.2019.02.004
Culver EL, Bungay HK, Betts M, Forde C, Buchel O, Manganis C, et al. Prevalence and long-term outcome of sub-clinical primary sclerosing cholangitis in patients with ulcerative colitis. Liver Int. 2020;40(11):2744-57. https://doi.org/10.1111/liv.14645
Palmela C, Peerani F, Castaneda D, Torres J, Itzkowitz SH. Inflammatory bowel disease and primary sclerosing cholangitis: A review of the phenotype and associated specific features. Gut Liver. 2018;12(1):17-29. https://doi.org/10.5009/gnl16510
Mertz A, Nguyen NA, Katsanos KH, Kwok RM. Primary sclerosing cholangitis and inflammatory bowel disease comorbidity: An update of the evidence. Ann Gastroenterol. 2019;32(2):124-33. https://doi.org/10.20524/aog.2019.0344
Greuter T, Vavricka S, König AO, Beaugerie L, Scharl M; Swiss IBDnet, an official working group of the Swiss Society of Gastroenterology. Malignancies in inflammatory bowel disease. Digestion. 2020;101(1):136-45. https://doi.org/10.1159/000509544
Althumairi AA, Lazarev MG, Gearhart SL. Inflammatory bowel disease associated neoplasia: A surgeon’s perspective. World J Gastroenterol. 2016;22(3):961-73. https://doi.org/10.3748/wjg.v22.i3.961
Choi CR, Al Bakir I, Ding NJ, Lee GH, Askari A, Warusavitarne J, et al. Cumulative burden of inflammation predicts colorectal neoplasia risk in ulcerative colitis: A large single-centre study. Gut. 2019;68(3):414-22. https://doi.org/10.1136/gutjnl-2017-314190
Hnatyszyn A, Hryhorowicz S, Kaczmarek-Ryś M, Lis E, Słomski R, Scott RJ, et al. Colorectal carcinoma in the course of inflammatory bowel diseases. Hered Cancer Clin Prac. 2019;17(18):1-9. https://doi.org/10.1186/s13053-019-0118-4
Stidham RW, Higgins PDR. Colorectal cancer in inflammatory bowel disease. Clin Colon Rectal Surg. 2018;31(3):168-78. https://doi.org/10.1055/s-0037-1602237
Levesque BG, Sandborn WJ, Ruel J, Feagan BG, Sands BE, Colombel JF. Converging goals of treatment of inflammatory bowel disease from clinical trials and practice. Gastroenterology. 2015;148(1):37-51.e1. https://doi.org/10.1053/j.gastro.2014.08.003
Hazel K, O’Connor A. Emerging treatments for inflammatory bowel disease. Ther Adv Chronic Dis. 2020;11:2040622319899297. https://doi.org/10.1177/2040622319899297
Sampietro GM, Colombo F, Corsi F. Sequential approach for a critical view colectomy (SACCO): A laparoscopic technique to reduce operative time and complications in IBD acute severe colitis. J Clin Med. 2020;9(10):3382. https://doi.org/10.3390/jcm910338
Sica GS, Biancone L. Surgery for inflammatory bowel disease in the era of laparoscopy. World J Gastroenterol. 2013;19(16):2445-8. https://doi.org/10.3748/wjg.v19.i16.2445
Peyrin-Biroulet L, Loftus Jr EV, Colombel JF, Sandborn WJ. The natural history of adult Crohn’s disease in population-based cohorts. Am J Gastroenterol. 2010;105(2):289-97. https://doi.org/10.1038/ajg.2009.579
Azolas Marcos R, Díaz Beneventi M. Tratamiento quirúrgico de la enfermedad de Crohn [Internet]. Chile: Equipo de Cirugía Colorrectal (consultado el 12 de marzo de 2021). Disponible en: http://medfinis.cl/img/manuales/e_crohn.pdf
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














