Cardiac hemodynamic variables and post-liver transplant outcomes in a transplant referral center in Colombia at 2,600 meters above sea level
DOI:
https://doi.org/10.22516/25007440.923Keywords:
Liver transplantation, Liver cirrhosis, Ventricular DysfunctionAbstract
Introduction: Hemodynamic assessment by Doppler echocardiography is essential in identifying systolic/diastolic changes as a predictor of outcomes in post-liver transplantation, from cardiovascular changes to graft dysfunction and mortality.
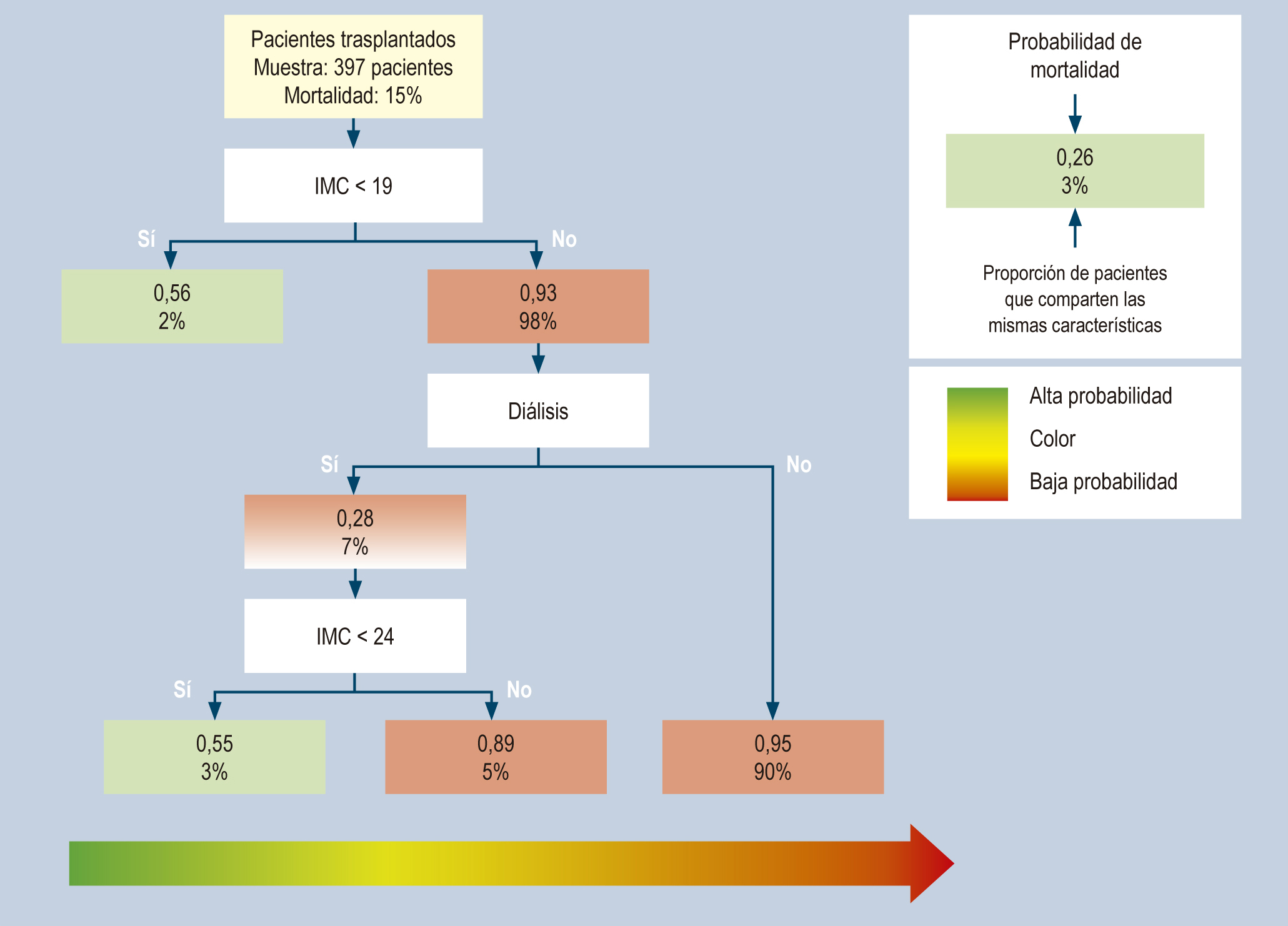
Materials and methods: Retrospective cohort study. Patient with a liver transplant at the LaCardio hospital in Bogotá, Colombia, between January 2005 and July 2021. Analysis of sociodemographic variables, comorbidities, echocardiography, and intraoperative variables with primary outcomes such as early graft dysfunction, acute kidney injury (AKI), and mortality during follow-up. A classification and regression tree (CART) was performed.
Results: 397 patients were analyzed; 54.4% were men, 71% had some degree of diastolic dysfunction and left ventricular hypertrophy (30.9%) with graft dysfunction in 8% and AKI in 21%, and a mortality of 15% during the study follow-up. In the CART model, mortality and graft dysfunction outcomes were related to a body mass index (BMI) < 19 or a combination of BMI between 19 and < 24 with dialysis.
Conclusion: Echocardiographic variables, sarcopenia, AKI, or the requirement for renal replacement therapy are related to mortality and graft dysfunction outcomes.
Downloads
References
Wiesner RH, Demetris AJ, Belle SH, Seaberg EC, Lake JR, Zetterman RK, et al. Acute hepatic allograft rejection: Incidence, risk factors, and impact on outcome. Hepatology. 1998;28(3):638-45. https://doi.org/10.1002/hep.510280306
Rdmji A, Yosbidu EM, Buin VG, Knetemun NM, Erb SR, Purtovi N, et al. The Western Canada Experience. Liver Transpl. 2002;8(10):945-51. https://doi.org/10.1053/jlts.2002.34969
Mittal C, Qureshi W, Singla S, Ahmad U, Huang MA. Pre-transplant left ventricular diastolic dysfunction is associated with post transplant acute graft rejection and graft failure. Dig Dis Sci. 2014;59(3):674-80. https://doi.org/10.1007/s10620-013-2955-8
Therapondos G, Flapan AD, Plevris JN, Hayes PC. Cardiac morbidity and mortality related to orthotopic liver transplantation. Liver Transplant. 2004;10(12):1441-53. https://doi.org/10.1002/lt.20298
Raval Z, Harinstein ME, Skaro AI, Erdogan A, Dewolf AM, Shah SJ, et al. Cardiovascular risk assessment of the liver transplant candidate. J Am Coll Cardiol. 2011;58(3):223-31. https://doi.org/10.1016/j.jacc.2011.03.026
Aghaulor B, VanWagner LB. Cardiac and Pulmonary Vascular Risk Stratification in Liver Transplantation. Clin Liver Dis. 2021;25(1):157-77. https://doi.org/10.1016/j.cld.2020.08.008
Zambruni A, Trevisani F, Caraceni P, Bernardi M. Cardiac electrophysiological abnormalities in patients with cirrhosis. J Hepatol. 2006;44(5):994-1002. https://doi.org/10.1016/j.jhep.2005.10.034
Liu H, Lee SS. Diagnostic Criteria of Cirrhotic Cardiomyopathy: Out With the Old, in With the New? Hepatology. 2021;74(6):3523-3525. https://doi.org/10.1002/hep.32021
Dowsley TF, Bayne DB, Langnas AN, Dumitru I, Windle JR, Porter TR, et al. Diastolic Dysfunction in Patients With End-Stage Liver Disease is Associated With Development of Heart Failure Early After Liver Transplantation. 2012;94(6):646-51. https://doi.org/10.1097/TP.0b013e31825f0f97
Moon YJ, Kim JW, Bang YS, Lim YS, Ki Y, Sang BH. Prediction of all-cause mortality after liver transplantation using left ventricular systolic and diastolic function assessment. PLoS One. 2019;14(1):e0209100. https://doi.org/10.1371/journal.pone.0209100
Josefsson A, Fu M, Allayhari P, Björnsson E, Castedal M, Olausson M, et al. Impact of peri-transplant heart failure & left-ventricular diastolic dysfunction on outcomes following liver transplantation. Liver Int. 2012;32(8):1262-9. https://doi.org/10.1111/j.1478-3231.2012.02818.x
Rayes N, Bechstein WO, Keck H, Blumhardt G, Lohmann R, Neuhaus P. Changing patterns of causes of death after liver transplantation: an analysis of 41 cases in 382 patients. Transplant Proc. 1995;27(1):1237-8.
Raevens S, De Pauw M, Geerts A, Berrevoet F, Rogiers X, Troisi RI, et al. Prevalence and outcome of diastolic dysfunction in liver transplantation recipients. Acta Cardiol. 2014;69(3):273-80. https://doi.org/10.1080/AC.69.3.3027830
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29(4):277-314. https://doi.org/10.1016/j.echo.2016.01.011
Therneau T, Atkinson B, Ripley B. Rpart: Recursive Partitioning. R Package Version 4.1-3. 2013. Disponible en: http://CRAN.R-project.org/package=rpart
Moon AM, Singal AG, Tapper EB. Contemporary Epidemiology of Chronic Liver Disease and Cirrhosis. Clin Gastroenterol Hepatol. 2020;18(12):2650-2666. https://doi.org/10.1016/j.cgh.2019.07.060
Escorcia Charris EJ, Marrugo Balceiro WR. Caracterización epidemiológica y clínica de la cirrosis hepática en un centro regional del caribe colombiano: clínica general del norte. Enero 2012 a marzo 2017. Biociencias. 2018;13(1):17-30. https://doi.org/10.18041/2390-0512/bioc.1.2242
Axelrod DA, Schnitzler M, Salvalaggio PR, Swindle J, Abecassis MM. The economic impact of the utilization of liver allografts with high donor risk index. Am J Transplant. 2007;7(4):990-7. https://doi.org/10.1111/j.1600-6143.2006.01724.x
Qureshi W, Mittal C, Ahmad U, Alirhayim Z, Hassan S, Qureshi S, et al. Clinical predictors of post-liver transplant new-onset heart failure. Liver Transplant. 2013;19(7):701-10. https://doi.org/10.1002/lt.23654
VanWagner LB, Lapin B, Levitsky J, Wilkins JT, Abecassis MM, Skaro AI, et al. High early cardiovascular mortality after liver transplantation. Liver Transplant Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc. 2014;20(11):1306-16. https://doi.org/10.1002/lt.23950
Chen Y, Chan AC, Chan S, Chok S, Sharr W, Fung J, et al. Original article A detailed evaluation of cardiac function in cirrhotic patients and its alteration with or without liver transplantation. J Cardiol. 2016;67(2):140-6. https://doi.org/10.1016/j.jjcc.2015.08.001
Ruíz-del-Árbol L, Achécar L, Serradilla R, Rodríguez-Gandía MÁ, Rivero M, Garrido E, et al. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology. 2013;58(5):1732-41. https://doi.org/10.1002/hep.26509
Bianchi G, Marchesini G, Marzocchi R, Pinna AD, Zoli M. Metabolic syndrome in liver transplantation: relation to etiology and immunosuppression. Liver Transplant Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc. 2008;14(11):1648-54. https://doi.org/10.1002/lt.21588
Leithead JA, Kandiah K, Steed H, Gunson BK, Steeds RP, Ferguson JW. Tricuspid regurgitation on echocardiography may not be a predictor of patient survival after liver transplantation. Am J Transplant. 2014;14(9):2192-3. https://doi.org/10.1111/ajt.12821
Batra S, Machicao VI, Bynon JS, Mehta S, Tanikella R, Krowka MJ, et al. The impact of left ventricular hypertrophy on survival in candidates for liver transplantation. Liver Transpl. 2014;20(6):705-12. https://doi.org/10.1002/lt.23875
Sonny A, Ibrahim A, Schuster A, Jaber WA, Cywinski JB. Impact and persistence of cirrhotic cardiomyopathy after liver transplantation. Clin Transplant. 2016;30(9):986-93. https://doi.org/10.1111/ctr.12778
Krag A, Bendtsen F, Henriksen JH, Møller S. Low cardiac output predicts development of hepatorenal syndrome and survival in patients with cirrhosis and ascites. Gut. 2010;59(1):105-10. https://doi.org/10.1136/gut.2009.180570
Chaney A. A Review for the Practicing Clinician: Hepatorenal Syndrome, a Form of Acute Kidney Injury, in Patients with Cirrhosis. Clin Exp Gastroenterol. 2021;14:385-96. https://doi.org/10.2147/CEG.S323778
Bushyhead D, Kirkpatrick JN, Goldberg D. Pretransplant echocardiographic parameters as markers of posttransplant outcomes in liver transplant recipients. Liver Transpl. 2016;(3):316-23. https://doi.org/10.1002/lt.24375
Habash F, Gurram P, Almomani A, Duarte A, Hakeem A, Vallurupalli S, et al. Correlation between echocardiographic pulmonary artery pressure estimates and right heart catheterization measurement in liver transplant candidates. J Cardiovasc Imaging. 2018;26(2):75-84. https://doi.org/10.4250/jcvi.2018.26.e2
Hsieh CE, Hsu YL, Lin KH, Lin PY, Hung YJ, Lai YC, et al. Association between surgical volumes and hospital mortality in patients: a living donor liver transplantation single center experience. BMC Gastroenterol. 2021;21(1):228. https://doi.org/10.1186/s12876-021-01732-6
Bajaj JS, Kamath PS, Reddy KR. The Evolving Challenge of Infections in Cirrhosis. N Engl J Med. 2021;384(24):2317-30. https://doi.org/10.1056/NEJMra2021808
Dhaliwal A, Armstrong MJ. Sarcopenia in cirrhosis: A practical overview. Clin Med (Lond). 2020;20(5):489-492. https://doi.org/10.7861/clinmed.2020-0089
Montano-Loza AJ, Meza-Junco J, Prado CMM, Lieffers JR, Baracos VE, Bain VG, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2012;10(2):166-73, 173.e1. https://doi.org/10.1016/j.cgh.2011.08.028
Lee J, Jeong WK, Kim JH, Kim JM, Kim TY, Choi GS, et al. Serial Observations of Muscle and Fat Mass as Prognostic Factors for Deceased Donor Liver Transplantation. Korean J Radiol. 2021;22(2):189-97. https://doi.org/10.3348/kjr.2019.0750
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














