Endoscopic Findings in Patients with Moderate to Severe COVID-19: A Cross-sectional Study
DOI:
https://doi.org/10.22516/25007440.949Keywords:
COVID-19, Coronavirus, Endoscopy, Gastrointestinal Bleeding, Gastrointestinal diseases, Gastrointestinal TractAbstract
Introduction: SARS CoV-2 infection has diverse gastrointestinal manifestations, which on many occasions require endoscopy.
Objective: The primary objective is to describe the need for endoscopic procedures from a sample of hospitalized patients with moderate to severe COVID-19, and the secondary objective is to describe in detail the characteristics, findings and interventions.
Materials and methods: descriptive observational cross-sectional study during May 2020 to December 2021, about indications, endoscopic findings, interventions, anesthesia requirement and adverse events, from a sample of patients with moderate to severe COVID-19 in whom gastrointestinal endoscopic procedures were performed for any indication.
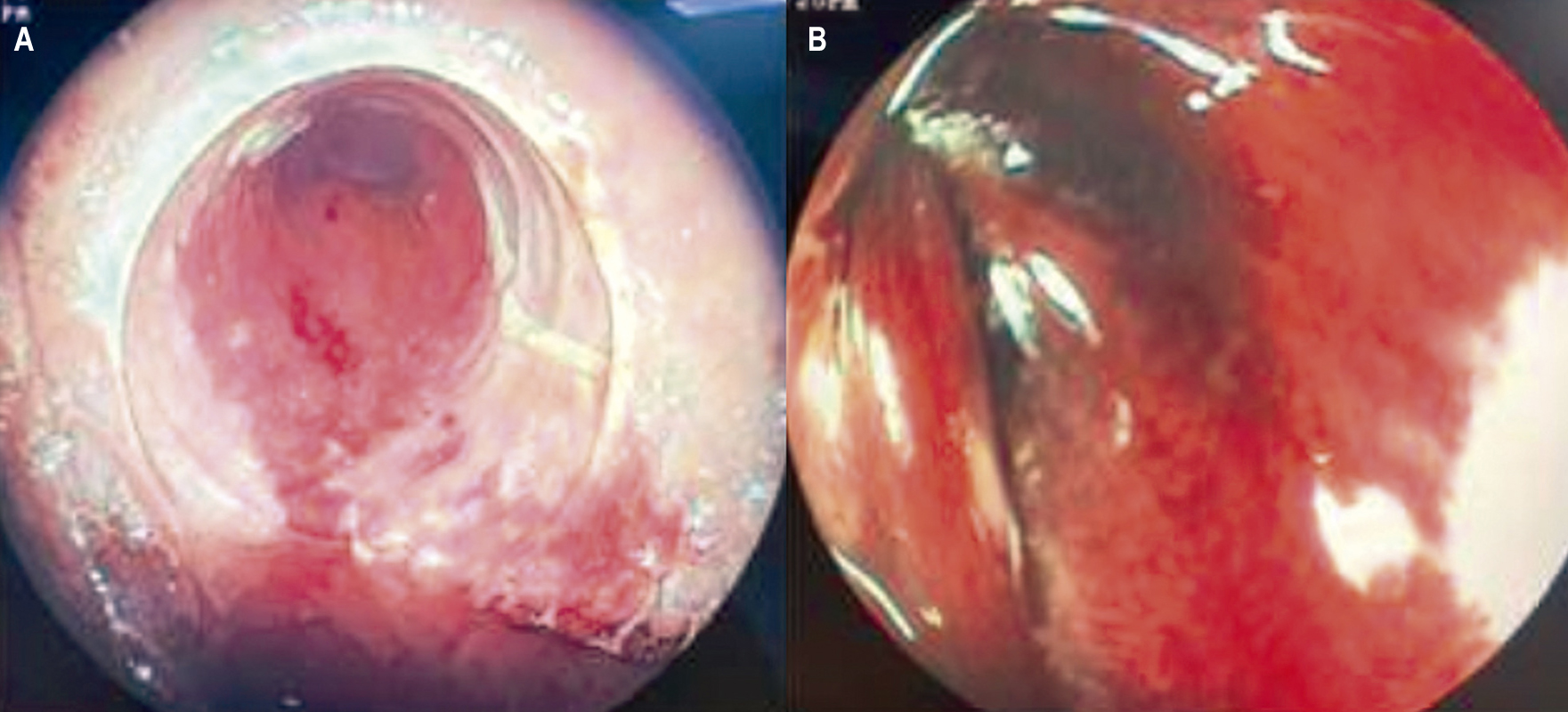
Results: of 2312 hospitalized patients with moderate to severe COVID-19, 2.72% required endoscopic procedures, with a predominance of men (75%), mean age 65.7 years, and the majority for upper gastrointestinal endoscopy (68%). The most frequent indications were gastrointestinal bleeding (62%) and enteral access (28.3%). Ischemic compromise was documented in three patients. In those with gastrointestinal bleeding, 9.5% required hemostatic therapy. 65% were on ventilatory support and sedation at the time of the endoscopic procedure, and in half of these cases anesthesiology support was required, with no peri-procedural adverse events, and no need for negative pressure room in any procedure.
Conclusions: In patients with moderate-severe COVID-19 and requiring gastrointestinal endoscopy, clinical judgment is required to define the pertinence of the procedure, and in many cases conservative management can be considered.
Downloads
References
Hunt RH, East JE, Lanas A, Malfertheiner P, Satsangi J, Scarpignato C, et al. COVID-19 and Gastrointestinal Disease: Implications for the Gastroenterologist. Dig Dis. 2021;39(2):119-39. https://doi.org/10.1159/000512152
Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382(10):929-36. https://doi.org/10.1056/NEJMoa2001191
Dhar J, Samanta J, Kochhar R. Corona Virus Disease-19 pandemic: The gastroenterologists' perspective. Indian J Gastroenterol. 2020;39(3):220-31. https://doi.org/10.1007/s12664-020-01075-2
Sultan S, Altayar O, Siddique SM, Davitkov P, Feuerstein JD, Lim JK, et al. AGA Institute Rapid Review of the Gastrointestinal and Liver Manifestations of COVID-19, Meta-Analysis of International Data, and Recommendations for the Consultative Management of Patients with COVID-19. Gastroenterology. 2020;159(1):320-334.e27. https://doi.org/10.1053/j.gastro.2020.05.001
Kuftinec G, Elmunzer BJ, Amin S, Elmunzer J, Spitzer RL, Foster LD, et al. The role of endoscopy and findings in COVID-19 patients, an early North American Cohort. BMC Gastroenterol. 2021;21(1):1-2. https://doi.org/10.1186/s12876-021-01796-4
Massironi S, Viganò C, Dioscoridi L, Filippi E, Pagliarulo M, Manfredi G, et al. Endoscopic Findings in Patients Infected With 2019 Novel Coronavirus in Lombardy, Italy. Clin Gastroenterol Hepatol. 2020;18(10):2375-7. https://doi.org/10.1016/j.cgh.2020.05.045
Vanella G, Capurso G, Burti C, Fanti L, Ricciardiello L, Souza Lino A, et al. Gastrointestinal mucosal damage in patients with COVID-19 undergoing endoscopy: An international multicentre study. BMJ Open Gastroenterol. 2021;8(1):19-21. https://doi.org/10.1136/bmjgast-2020-000578
Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667-78. https://doi.org/10.1016/S2468-1253(20)30126-6
D'Amico F, Baumgart DC, Danese S, Peyrin-Biroulet L. Diarrhea During COVID-19 Infection: Pathogenesis, Epidemiology, Prevention, and Management. Clin Gastroenterol Hepatol. 2020;18(8):1663-72. https://doi.org/10.1016/j.cgh.2020.04.001
Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51(9):843-51. https://doi.org/10.1111/apt.15731
Elmunzer BJ, Spitzer RL, Foster LD, Merchant AA, Howard EF, Patel VA, et al. Digestive Manifestations in Patients Hospitalized With Coronavirus Disease 2019. Clin Gastroenterol Hepatol. 2021;19(7):1355-1365.e4.
COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Available at https://www.covid19treatmentguidelines.nih.gov/.
Armstrong D, Bennett JR, Blum AL, Dent J, De Dombal FT, Galmiche P, et al. The endoscopic assessment of esophagitis: A progress report on observer agreement. Gastroenterology. 1996;111(1):85-92. https://doi.org/10.1053/gast.1996.v111.pm8698230
Blackett JW, Kumta NA, Dixon RE, David Y, Nagula S, DiMaio CJ, et al. Characteristics and Outcomes of Patients Undergoing Endoscopy During the COVID-19 Pandemic: A Multicenter Study from New York City. Dig Dis Sci. 2021;66(8):2545-54. https://doi.org/10.1007/s10620-020-06593-9
Goudra B, Nuzat A, Singh PM, Borle A, Carlin A, Gouda G. Association between type of sedation and the adverse events associated with gastrointestinal endoscopy: An analysis of 5 years' data from a Tertiary center in the USA. Clin Endosc. 2017;50(2):161-9. https://doi.org/10.5946/ce.2016.019
Cooper GS, Kou TD, Rex DK. Complications following colonoscopy with anesthesia assistance: A population-based analysis. JAMA Intern Med. 2013;173(7):551-6. https://doi.org/10.1001/jamainternmed.2013.2908
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














