Right colon neuroendocrine tumor in a patient with ulcerative colitis: A case study
DOI:
https://doi.org/10.22516/25007440.603Keywords:
Gastrointestinal neuroendocrine tumor, ulcerative colitis, inflammatory bowel disease, neuroendocrine colon tumorAbstract
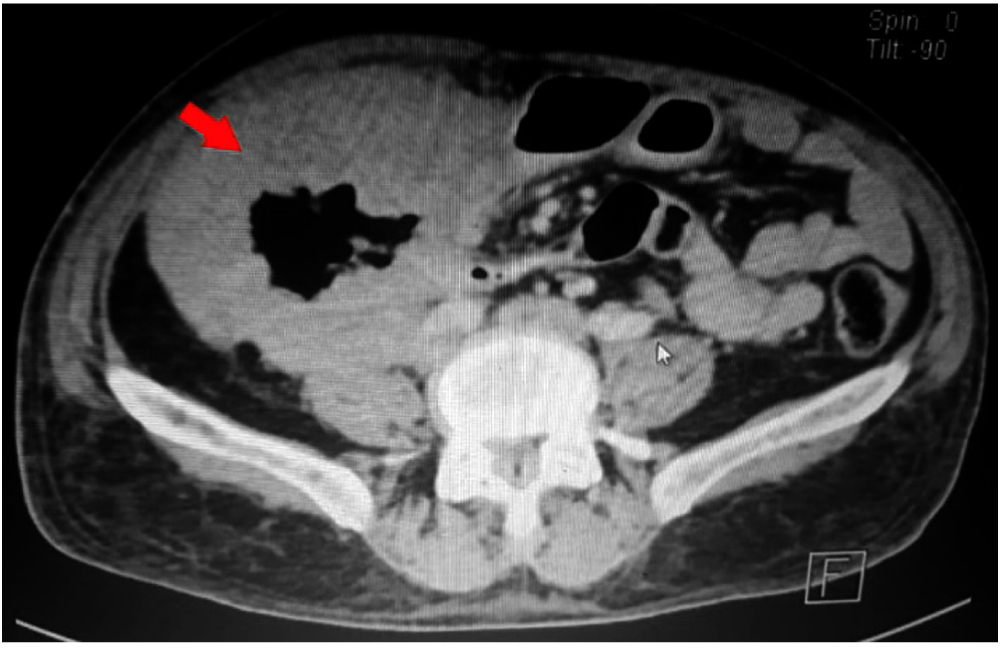
Neuroendocrine colon tumors are relatively unknown compared with sporadic colorectal cancer; its incidence is low, and it is generally located in the cecum, sigmoid colon, and rectum. The existing relation between neuroendocrine tumors and ulcerative colitis is not frequently described due to the chronic inflammation that leads to neuroendocrine cell differentiation from multipotential cells in the dysplastic epithelium, which can be responsible for colorectal neuroendocrine carcinomas development. The study refers to the case of a patient of 57 years old with ulcerative colitis, abdominal pain, weight loss, and liquid diarrhea with mucus. Physical examination revealed a hardened lesion in the right colonic framework with the tomography of a neoplastic lesion in the ascending colon. When the patient was hospitalized, he developed an intestinal obstruction. A hemicolectomy plus ileostomy procedure was performed resulting in a large cell G3 neuroendocrine tumor in the ascending colon revealed in the biopsy. In this article, the aspects related to the pathophysiology, diagnosis, and treatment of the association of these two pathologies are reviewed in a practical way.
Downloads
References
Bannura G, Barrera A, Melo C, Illanes F, Gallardo C. Tumores neuroendocrinos primarios de colon y recto. Rev Chil Cir. 2018;70(1):53-58. https://doi.org/10.4067/S0718-40262018000100053
Stoner P, Ghaffaripour T, Cohen D. Aggressive large-cell neuroendocrine carcinoma of the sigmoid colon in a patient with ulcerative colitis. BMJ Case Rep. 2017;2017:bcr2017220093. https://doi.org/10.1136/bcr-2017-220093
Grassia R, Bodini P, Dizioli P, Staiano T, Iiritano E, Bianchi G, Buffoli F. Neuroendocrine carcinomas arising in ulcerative colitis: coincidences or possible correlations? World J Gastroenterol. 2009;15(33):4193-5. https://doi.org/10.3748/wjg.15.4193
Vilallonga R, Espín Basany E, López Cano M, Landolfi S, Armengol Carrasco M. Carcinomas neuroendocrinos de colon y recto. Experiencia de una unidad en seis años. Rev Esp Enferm Dig. 2008;100(1):11-6. https://doi.org/10.4321/s1130-01082008000100003
Wong NA, Harrison DJ. Colorectal neoplasia in ulcerative colitis-recent advances. Histopathology. 2001;39(3):221-34. https://doi.org/10.1046/j.1365-2559.2001.01292.x
Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48(4):526-35. https://doi.org/10.1136/gut.48.4.526
Carvalho JR, Fernandes SR, Correia LA. Extensive Neuroendocrine Adenocarcinoma in Ulcerative Colitis. J Crohns Colitis. 2016;10(1):116-7. https://doi.org/10.1093/ecco-jcc/jjv177
Rifu K, Koinuma K, Horie H, Morimoto M, Kono Y, Tahara M, Sakuma Y, Hosoya Y, Kitayama J, Lefor AK, Sata N, Suzuki T, Fukushima N. Sigmoid colon carcinoma with focal neuroendocrine differentiation associated with ulcerative colitis: A case report. Int J Surg Case Rep. 2016;23:151-6. https://doi.org/10.1016/j.ijscr.2016.04.035
Sigel JE, Goldblum JR. Neuroendocrine neoplasms arising in inflammatory bowel disease: a report of 14 cases. Mod Pathol. 1998;11(6):537-42.
Shigaki K, Mitomi H, Fujimori T, Ichikawa K, Tomita S, Imura J, Fujii S, Itabashi M, Kameoka S, Sahara R, Takenoshita S. Immunohistochemical analysis of chromogranin A and p53 expressions in ulcerative colitis-associated neoplasia: neuroendocrine differentiation as an early event in the colitis-neoplasia sequence. Hum Pathol. 2013;44(11):2393-9. https://doi.org/10.1016/j.humpath.2013.06.008
Korse CM, Taal BG, van Velthuysen ML, Visser O. Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: experience of two decades of cancer registry. Eur J Cancer. 2013;49(8):1975-83. https://doi.org/10.1016/j.ejca.2012.12.022
Shia J, Tang LH, Weiser MR, Brenner B, Adsay NV, Stelow EB, Saltz LB, Qin J, Landmann R, Leonard GD, Dhall D, Temple L, Guillem JG, Paty PB, Kelsen D, Wong WD, Klimstra DS. Is nonsmall cell type high-grade neuroendocrine carcinoma of the tubular gastrointestinal tract a distinct disease entity? Am J Surg Pathol. 2008;32(5):719-31. https://doi.org/10.1097/PAS.0b013e318159371c
Bolzacchini E, Chini C, Cortelezzi CC, Vallini I, Pinotti G, La Rosa S, Uccella S. Poorly Differentiated Neuroendocrine Carcinoma of the Sigmoid Tract in Long-Standing Ulcerative Colitis: Report of a Case and Review of the Literature. Int J Surg Pathol. 2018;26(5):479-483. https://doi.org/10.1177/1066896917752443
Minocha V, Shuja S, Ali R, Eid E. Large cell neuroendocrine carcinoma of the rectum presenting with extensive metastatic disease. Case Rep Oncol Med. 2014;2014:386379. https://doi.org/10.1155/2014/386379
Shen C, Yin Y, Chen H, Tang S, Yin X, Zhou Z, Zhang B, Chen Z. Neuroendocrine tumors of colon and rectum: validation of clinical and prognostic values of the World Health Organization 2010 grading classifications and European Neuroendocrine Tumor Society staging systems. Oncotarget. 2017;8(13):22123-22134. https://doi.org/10.18632/oncotarget.13641
Choi CW, Kang DH, Kim HW, Park SB, Jo WS, Song GA, Cho M. Comparison of endoscopic resection therapies for rectal carcinoid tumor: endoscopic submucosal dissection versus endoscopic mucosal resection using band ligation. J Clin Gastroenterol. 2013;47(5):432-6. https://doi.org/10.1097/MCG.0b013e31826faf2b
Moertel CG, Kvols LK, O’Connell MJ, Rubin J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin. Evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer. 1991;68(2):227-32. https://doi.org/10.1002/1097-0142(19910715)68:2<227::aid-cncr2820680202>3.0.co;2-i
Sun W, Lipsitz S, Catalano P, Mailliard JA, Haller DG; Eastern Cooperative Oncology Group. Phase II/III study of doxorubicin with fluorouracil compared with streptozocin with fluorouracil or dacarbazine in the treatment of advanced carcinoid tumors: Eastern Cooperative Oncology Group Study E1281. J Clin Oncol. 2005;23(22):4897-904. https://doi.org/10.1200/JCO.2005.03.616
Kedia S, Ahuja V, Tandon R. Management of acute severe ulcerative colitis. World J Gastrointest Pathophysiol. 2014;5(4):579-88. https://doi.org/10.4291/wjgp.v5.i4.579. PMID: 25401001
Yamamoto-Furusho JK, Gutiérrez-Grobe Y, López-Gómez JG, Bosques-Padilla F, Rocha-Ramírez JL; Grupo del Consenso Mexicano de Colitis Ulcerosa Crónica Idiopática. Consenso mexicano para el diagnóstico y tratamiento de la colitis ulcerosa crónica idiopática. Rev Gastroenterol Mex. 2018;83(2):144-167. https://doi.org/10.1016/j.rgmx.2017.08.006
Li Y, Shen B. Evaluating pouch problems. Gastroenterol Clin North Am. 2012;41(2):355-78. https://doi.org/10.1016/j.gtc.2012.01.013
Gallone L, Olmi L, Marchetti V. Use of topical rectal therapy to preserve the rectum in surgery of ulcerative colitis. World J Surg. 1980;4(5):609-13. https://doi.org/10.1007/BF02401644
Trujillo-Díaz JJ, Blanco-Antona F, de Solórzano-Aurusa JO, Martínez-García G, Fernández-Salazar L, Rentería JPBHY. Neuroendocrine tumor associate with inflammatory bowel disease: two cases report. Cir Cir. 2019;87(S1):17-21. https://doi.org/10.24875/CIRU.18000519
La Rosa S, Klersy C, Uccella S, Dainese L, Albarello L, Sonzogni A, Doglioni C, Capella C, Solcia E. Improved histologic and clinicopathologic criteria for prognostic evaluation of pancreatic endocrine tumors. Hum Pathol. 2009;40(1):30-40. https://doi.org/10.1016/j.humpath.2008.06.005
Sánchez-Bueno F, Rodríguez González JM, Torres Salmerón G, Bernabé Peñalver A, Balsalobre Salmeron M, de la Peña Moral J, Fuster Quiñonero M, Parrilla Paricio P. Prognostic factors in resected pancreatic neuroendocrine tumours: Experience in 95 patients. Cir Esp. 2016;94(8):473-80. https://doi.org/10.1016/j.ciresp.2016.05.010
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














