Severe flare-up in a patient with Crohn’s disease and coinfection by SARS-CoV-2: Clinical approach and treatment
DOI:
https://doi.org/10.22516/25007440.685Keywords:
Crohn’s disease, COVID-19, Inflammatory bowel disease, SARS-CoV-2, Case reportAbstract
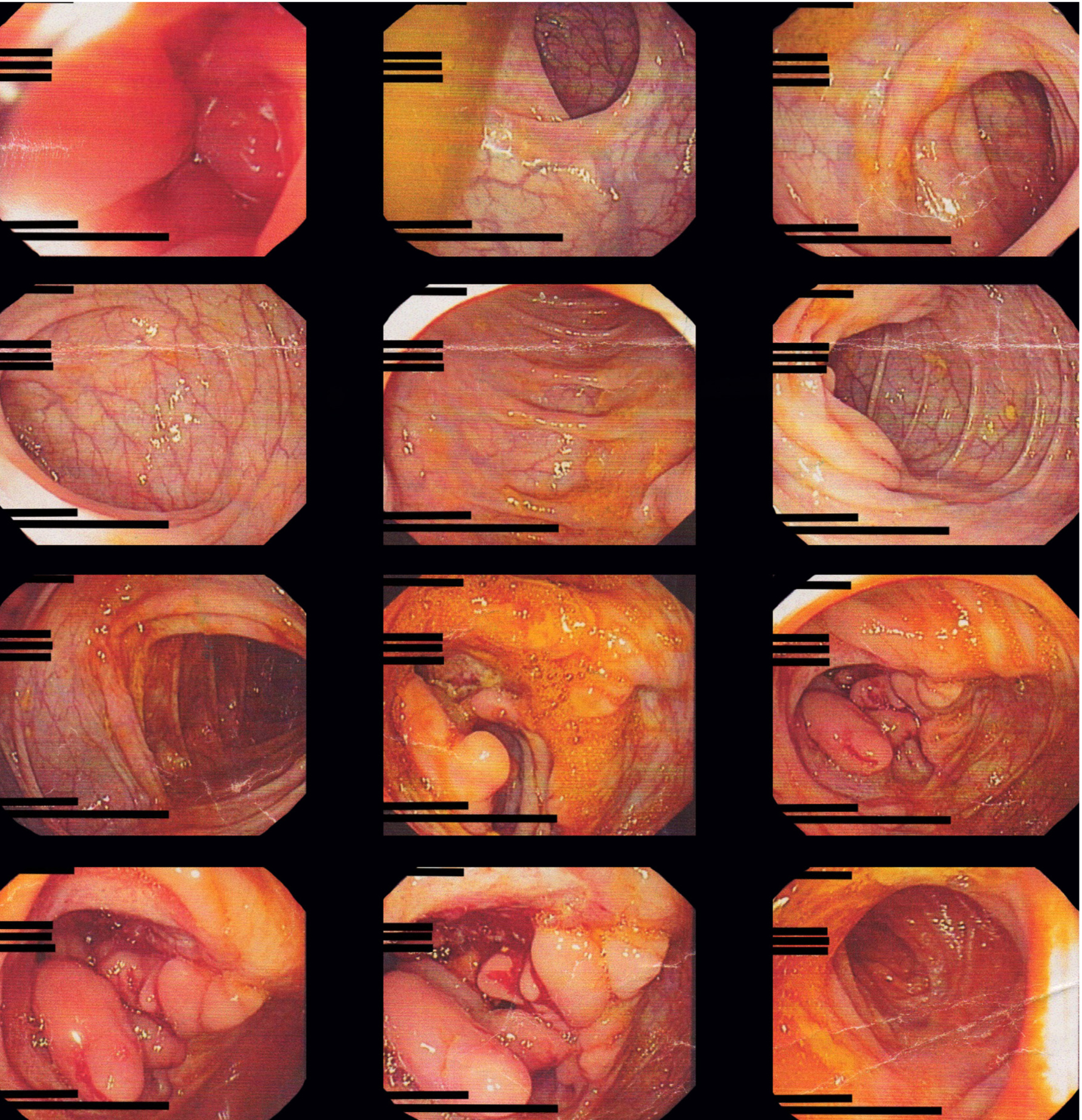
Crohn's disease is considered a chronic immune-mediated disease, which physiopathologically is characterized by being a multifactorial disease in which environmental and genetic factors intervene, among others. Patients have a risk to develop complications not only related to the disease, but also because of the medication used to treat it. This risk plays a relevant role today due to the 2019 coronavirus disease, an infection that has been shown more serious in patients with comorbidities, which increases morbidity and mortality. In this study is analyzed a young man case with underlying Crohn’s disease with symptoms and signs of intestinal obstruction and systemic inflammatory response. He was admitted for the first time with a severe flare-up in the terminal ileum, compatible with perforation associated with local collection and secondary adynamic ileus and presents a co-infection with the severe acute respiratory syndrome type 2 coronavirus (SARS-CoV-2). The case presentation, discussion, and review of the literature on the diagnosis of a severe flare-up of Crohn's disease and SARS-CoV-2 coinfection, clinical approach and treatment are carried out.
Downloads
References
Fernández-Ávila DG, Bernal-Macías S, Parra-Izquierdo V, Rincón-Riaño DN, Gutiérrez JM, Rosselli D. Prevalencia en Colombia de la enfermedad inflamatoria intestinal y el compromiso articular asociado, según información del Sistema Integral de Información de la Protección Social. Rev Colomb Reumatol. 2020;27(1)3-8. https://doi.org/10.1016/j.rcreu.2019.10.006
Macdonald TT, Monteleone G. Immunity, inflammation, and allergy in the gut. Science. 2005;307(5717):1920-5. https://doi.org/10.1126/science.1106442
Beaugerie L, Kirchgesner J. Balancing Benefit vs Risk of Immunosuppressive Therapy for Individual Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2019;17(3):370-379. https://doi.org/10.1016/j.cgh.2018.07.013
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733. https://doi.org/10.1056/NEJMoa2001017
Parra-Izquierdo V, Flórez-Sarmiento C, García del Risco F, Romero-Sánchez C. Síntomas gastrointestinales en la enfermedad por COVID-19 y sus implicaciones en enfermedad inflamatoria intestinal. Rev Colomb Gastroenterol. 2020;35(Supl. 1):45-55. https://doi.org/10.22516/25007440.532
Bezzio C, Saibeni S, Variola A, Allocca M, Massari A, Gerardi V, Casini V, Ricci C, Zingone F, Amato A, Caprioli F, Lenti MV, Viganò C, Ascolani M, Bossa F, Castiglione F, Cortelezzi C, Grossi L, Milla M, Morganti D, Pastorelli L, Ribaldone DG, Sartini A, Soriano A, Manes G, Danese S, Fantini MC, Armuzzi A, Daperno M, Fiorino G; Italian Group for the Study of Inflammatory Bowel Disease (IG-IBD). Outcomes of COVID-19 in 79 patients with IBD in Italy: an IG-IBD study. Gut. 2020;69(7):1213-1217. https://doi.org/10.1136/gutjnl-2020-321411
Rodríguez-Lago I, Ramírez de la Piscina P, Elorza A, Merino O, Ortiz de Zárate J, Cabriada JL. Characteristics and Prognosis of Patients With Inflammatory Bowel Disease During the SARS-CoV-2 Pandemic in the Basque Country (Spain). Gastroenterology. 2020;159(2):781-783. https://doi.org/10.1053/j.gastro.2020.04.043
Redd WD, Zhou JC, Hathorn KE, McCarty TR, Bazarbashi AN, Thompson CC, Shen L, Chan WW. Prevalence and Characteristics of Gastrointestinal Symptoms in Patients With Severe Acute Respiratory Syndrome Coronavirus 2 Infection in the United States: A Multicenter Cohort Study. Gastroenterology. 2020;159(2):765-767.e2. https://doi.org/10.1053/j.gastro.2020.04.045
Marín-Jiménez I, Zabana Y, Rodríguez-Lago I, Marín L, Barreiro-de Acosta M, Esteve M; en representación de GETEII y GETECCU. COVID-19 and inflammatory bowel disease: questions arising from patient care and follow-up during the initial phase of the pandemic (February-April 2020). Gastroenterol Hepatol. 2020;43(7):408-413. https://doi.org/10.1016/j.gastrohep.2020.05.003
Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831-1833.e3. https://doi.org/10.1053/j.gastro.2020.02.055
Ahlawat S, Asha, Sharma KK. Immunological co-ordination between gut and lungs in SARS-CoV-2 infection. Virus Res. 2020;286:198103. https://doi.org/10.1016/j.virusres.2020.198103
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2):271-280.e8. https://doi.org/10.1016/j.cell.2020.02.052
Garg M, Royce SG, Tikellis C, Shallue C, Batu D, Velkoska E, Burrell LM, Patel SK, Beswick L, Jackson A, Britto K, Lukies M, Sluka P, Wardan H, Hirokawa Y, Tan CW, Faux M, Burgess AW, Hosking P, Monagle S, Thomas M, Gibson PR, Lubel J. Imbalance of the renin-angiotensin system may contribute to inflammation and fibrosis in IBD: a novel therapeutic target? Gut. 2020;69(5):841-851. https://doi.org/10.1136/gutjnl-2019-318512
Juliao-Baños F. Manejo de pacientes con enfermedad inflamatoria intestinal durante la pandemia de COVID-19d-19. Rev Colomb Gastroenterol. 2020;35(Supl. 1):37-44. https://doi.org/10.22516/25007440.537
Fiorino G, Allocca M, Furfaro F, Gilardi D, Zilli A, Radice S, Spinelli A, Danese S. Inflammatory Bowel Disease Care in the COVID-19 Pandemic Era: The Humanitas, Milan, Experience. J Crohns Colitis. 2020;14(9):1330-1333. https://doi.org/10.1093/ecco-jcc/jjaa058
Rubin DT, Abreu MT, Rai V, Siegel CA; International Organization for the Study of Inflammatory Bowel Disease. Management of Patients With Crohn’s Disease and Ulcerative Colitis During the Coronavirus Disease-2019 Pandemic: Results of an International Meeting. Gastroenterology. 2020;159(1):6-13.e6. https://doi.org/10.1053/j.gastro.2020.04.002
Crespo J, Andrade R, Alberca de Las Parras F, Balaguer F, Barreiro-de Acosta M, Bujanda L, Gutiérrez A, Jorquera F, Iglesias-García J, Sánchez-Yagüe A, Calleja JL. Resumption of activity in gastroenterology departments. Recommendations by SEPD, AEEH, GETECCU and AEG. Rev Esp Enferm Dig. 2020;112(5):397-411. https://doi.org/10.17235/reed.2020.7141/2020
Kappelman MD, Brenner EJ, Colombel JF, Ungaro RC, Agrawal M. Coronavirus and IBD Reporting Database [Internet]. SECURE-IBD [consultado el 8 de enero de 2021]. Disponible en: https://covidibd.org/
Downloads
Published
How to Cite
Issue
Section
License
Aquellos autores/as que tengan publicaciones con esta revista, aceptan los términos siguientes:
Los autores/as ceden sus derechos de autor y garantizarán a la revista el derecho de primera publicación de su obra, el cuál estará simultáneamente sujeto a la Licencia de reconocimiento de Creative Commons que permite a terceros compartir la obra siempre que se indique su autor y su primera publicación en esta revista.
Los contenidos están protegidos bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.


| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |














